Maximum And Target Heart Rate
Its important to know what your maximum heart rate should be to avoid causing harm to your heart or body. To calculate your maximum heart rate, subtract your age from 220. According to the American Heart Association , your target heart rate while doing moderately intense activities should be about 50% to 70% of your maximum heart rate. During vigorous exercise, it should be about 70% to 85% of your maximum heart rate.
If you exceed your maximum heart rate, you may experience sore joints, sore muscles, or musculoskeletal injuries. Heart rate monitors are great to wear while exercising because they tell you your heart rate in real-time.
Can Postural Orthostatic Tachycardia Syndrome Be Fatal
While POTS can be life-changing, it is not life-threatening. One of the biggest risks for people with POTS is falls due to fainting. Not everyone who has POTS faints. And, for those who do, it may be a rare event. But, if you dont know that you have POTS, you may not take precautions against trauma from falls.
What Exactly Is Postural Orthostatic Tachycardia Syndrome Or Pots
POTS is a form of dysautonomia, which means dysregulation of the autonomic nervous system. The autonomic nervous system regulates the bodily processes that happen automatically, without any thought on our part . Normally, when we stand up, our body performs automatic responses to compensate for this positional change so that we remain conscious. In someone with POTS, this response doesnt quite work as it should. And guess what happens then? Their heart races when standing up.
While there are several different subtypes of POTS , the orthostatic intolerance that occurs in POTS is because of inadequate circulation. Poor tightening of blood vessels in the lower body when upright leads to heightened and rapid blood pooling in the pelvis and legs.
And guess where blood needs to be to maintain consciousness? Your brain! When you have POTS and you ask yourself why your heart races when standing up its because your brain is shouting at your heart to pump more blood, faster. This rapid increase in standing heart rate is your body trying desperately to pump more blood up to your brain because too much of it is pooling in your lower body.
Make sense so far?
Recommended Reading: How To Calculate Target Heart Rate Zone
Who Treats Postural Orthostatic Tachycardia Syndrome
In many cases, your primary care physician is qualified to treat POTS. For complex POTS cases, it is often helpful to have input from a neurologist or cardiologist experienced in this condition. Rehabilitation physicians can help as well in developing an exercise plan that works for you.
Myositis and Neuromuscular Diseases | Q& A with Dr. Tae Chung
Heart Rate Suddenly Jumps: Why And How To Help
Under normal conditions, a healthy adults heart rate range from 60 to 100 beats per minute. There may be a sudden occasional increase in heart beat, which resolves in a couple of minutes. The condition is referred to as tachycardia and is generally harmless. However, if your increased heart beat is recurring or persistent or if other symptoms are also present, then you should consult a physician.
Also Check: Tylenol Heart Palpitations
Why Is My Heart Rate Constantly Above 100
Heart rates that are consistently above 100, even when the patient is sitting quietly, can sometimes be caused by an abnormal heart rhythm. A high heart rate can also mean the heart muscle is weakened by a virus or some other problem that forces it to beat more often to pump enough blood to the rest of the body.
Postural Tachycardia Syndrome: Multiple Symptoms But Easily Missed
ADDRESS FOR CORRESPONDENCE Lesley Kavi
The evolution of upright posture is usually considered an advantage in humans. For people with postural tachycardia syndrome it can present a daily challenge. Although orthostatic intolerance is often associated with older people, PoTS tends to affect young women who present with multiple, non-specific symptoms and significant functional impairment.
PoTS was characterised in 1993, but previously existed under various names including irritable heart, soldier’s heart, and idiopathic orthostatic intolerance. It is a heterogeneous group of disorders sharing similar characteristics as a consequence of abnormal autonomic nervous system response to assuming upright posture.
Also Check: Does Benadryl Lower Heart Rate
Heart Rate Questions: Rate Increases When Standing Or Waking Up
Well I know it does not seem ok. Last time I went to see the doctor, he said my resting heart rate was high 85 to 90. But I think I do have white coat syndrome cuz when I go to see docs, I will would be very nervous. He prescribed me the antenolol 50mg, for the first three weeks, I was fine but aferwards I started to have side effect dizziness, one night felt like blacked out and then cold hand and feet, ringing in ear, shortness of breath So I reduced the dosage to 25mg and took it for about a week and a half and then stopped for 3 days and it was worse, heart palpitation every night so I reduced the dosage to 12.5mg and then took it a couple days and then stopped cold turkey.
I did not tell my primary doctor when I stopped because he said that all these symptoms are due to my anxiety. I said that was a side effect and he did no t believe it and he said he is taking it too but 25mg.
At first I thought it was withdrawal symptom, cuz I had heart palpitations every morning when I woke up and that came with dizziness as well as shortness of breath on exertion and I ignored it but now it has been almost 4 months and it is getting worse.
3) Whenever I talk, no more than a few seconds I have to pause and take deep breath before continuing. The breathlessness on exertion does not go away and still exists.
Postural Orthostatic Tachycardia Syndrome Diet
The foundation of treating POTS is to drink fluids frequently throughout the day. For most POTS patients, the goal is at least 64-80 ounces a day. You would also need to increase your intake of salty foods and add more salt to your diet with a saltshaker or salt tablets. These dietary modifications help keep water in the bloodstream, which helps more blood reach the heart and the brain.
Certain foods or drinks can have an adverse effect on POTS symptoms in some patients. For example, alcohol almost always aggravates POTS. It diverts blood away from the central circulation to the skin and increases loss of fluids through urine. Caffeine can make some people more nervous and lightheaded, but for some it can help improve constriction of blood vessels. Your regular physician or POTS specialist can help you determine how your diet and certain medications could be helping or hindering your treatment.
Also Check: Does Benadryl Lower Heart Rate
Exercise For Postural Orthostatic Tachycardia Syndrome
Physical therapy can make a difference for some people with POTS. Because sometimes POTS symptoms can worsen with exercise, physical therapy has to start slowly and advance based on your tolerance rather than a rigid plan. As your blood circulation improves with medications and diet, the exercise intensity may be gradually increased. The goal is to retrain the autonomic nervous system to allow for more exercise, which then helps increase the blood volume.
Those who cant stand upright may start exercising in a horizontal or reclined position. Aquatic therapy may work for some POTS patients due to the water creating pressure around the body. Many experts find that manual physical therapy that addresses issues with nerve tightness and range of motion works as a bridge to build better tolerance of exercise.
How Do You Test For Pots Syndrome
POTS is diagnosed using either a 10-minute standing test or a head-up tilt table test occasionally other tests are performed to identify specific characteristics of POTS present in some patients. Most peoples POTS symptoms respond to a combination of diet, medications, physical therapy and other treatments.
Also Check: Tylenol Heart Rate
What To Expect At The Doctors
Your doctor may use a variety of diagnostic tools to help diagnose your condition, including:
- Electrocardiogram. Also referred to as an ECG or EKG, this diagnostic tool uses small electrodes to record the electrical activity of your heart. Your doctor can use the information collected to determine if heart abnormalities are contributing to your condition.
- Imaging tests. Imaging can be used to assess if there are any structural abnormalities in your heart that may be contributing to your condition. Possible imaging tests can include echocardiogram, CT scan, and MRI scan.
- Laboratory tests. Your doctor may order blood tests to determine if your condition is caused by something such as an electrolyte imbalance or thyroid disease.
Once a diagnosis is made, your doctor will work with you to develop a plan to treat and manage your condition.
Depending on the findings from the diagnostic tests, your doctor may refer you to a cardiologist. A cardiologist specializes in treating and preventing diseases of the heart and circulatory system.
Increase In Resting Heart Rate Is A Signal Worth Watching
- By Howard E. LeWine, MD, Chief Medical Editor, Harvard Health Publishing
When you sit quietly, your heart slips into the slower, steady pace known as your resting heart rate. An increase in your resting heart rate over time may be a signal of heart trouble ahead.
Your heart rate changes from minute to minute. It depends on whether you are standing up or lying down, moving around or sitting still, stressed or relaxed. Your resting heart rate, though, tends to be stable from day to day. The usual range for resting heart rate is anywhere between 60 and 90 beats per minute. Above 90 is considered high.
Many factors influence your resting heart rate. Genes play a role. Aging tends to speed it up. Regular exercise tends to slow your heart rate down. Stress, medications, and medical conditions also influence your resting heart rate.
Results of observational research studies support a link between health and heart rate. Researchers from Norway previously reported the results of a large study looking at changes in resting heart rate over 10 years. They recruited more than 29,000 people without any history or heart disease, high blood pressure, or any other type of cardiovascular disorder, and measured their resting heart rates when they started the study and again 10 years later. This study was published in the Journal of the American Medical Association.
How to lower your resting heart rate
Don’t Miss: How Does Heart Disease Affect The Skeletal System
Anita’s Story And Pregnancy Updates
My problems with pre-syncope spells began 13 years ago when I was 16. I had multiple dizzy spells when standing up the kind that most people have had at some point in their lives, maybe when standing up from a hot bath. Everything closes in and goes black and blurry. The GP put it down to hormones and being a teenager. The spells became more frequent and caused me to collapse to the floor, though I never lost consciousness. I was referred to a neurologist who also dismissed it as the result of being a young female.
Whats A Normal Heart Rate
A heart rate is a measurement of the number of times the heart muscle beats per minute. Healthy kids and adults will have hearts that beat at different speeds because of their age and body size. If the heart is beating too fast or too slow, this could mean you have an underlying health problem. Your resting heart rate will also allow you to gauge your current heart health.
In general, a lower resting heart rate means the heart is beating less per minute, which likely means its more efficient. Your resting heart rate tells you how fast your heart is beating when youre in a relaxed state, like sitting or laying down. If your resting heart rate is too high, this might mean you have lower physical fitness, or that youre at risk of developing a heart condition.
Knowing what your target heart rate should be for your age can help you recognize if and when your heart rate is abnormal, which may be an indication that its time to go to the doctor.
| Normal heart rate by age | |
|---|---|
| Age | |
| 18 and older | 60-100 bpm |
As we get older, the range of whats considered to be a healthy normal resting heart rate will change.
The average healthy adult will have a resting heart rate of 60 bpm or higher. Although in clinical practice, the resting heart rate between 60 and 100 bpm is considered to be normal, people with a resting heart rate higher than 80 bpm could have an increased risk of developing cardiovascular disease.
RELATED: Heart disease statistics
You May Like: Benadryl Heart Arrhythmia
Heart Rate Variability In Head
- 1Department of Clinical Neurophysiology, HUS Medical Imaging Center, Helsinki University Hospital, Helsinki, Finland
- 2Department of Neurological Sciences, University of Helsinki, Helsinki, Finland
- 3Vitalmed Helsinki Sleep Clinic, Helsinki, Finland
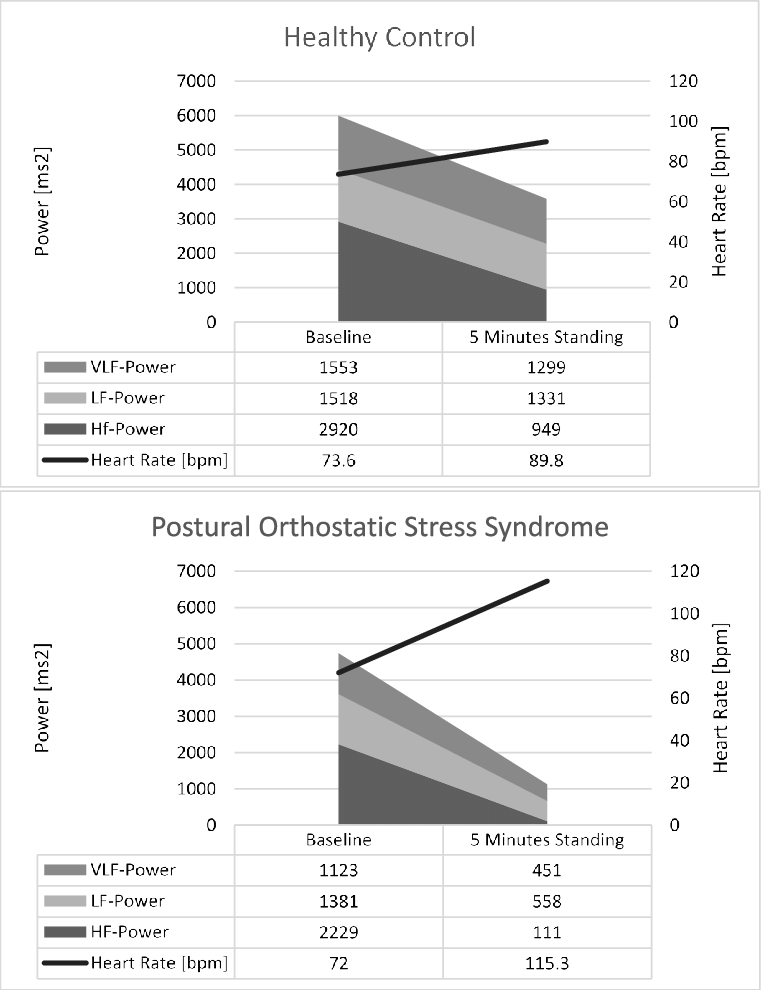
Introduction: Postural tachycardia syndrome is a suspected dysautonomia with symptoms of orthostatic intolerance and abnormally increased heart rate while standing. We aimed to study cardiac autonomic nervous system functioning in head-up tilt in adolescents with POTS to find out if parasympathetic tone is attenuated in the upright position.
Methods: We compared characteristics of a group of 25 adolescents with POTS and 12 without POTS aged 917 years. We compared heart rate variability with high- and low-frequency oscillations, and their temporal changes in HUT.
Results: The high-frequency oscillations, i.e., HF, attenuated in both groups during HUT , but the attenuation was bigger in POTS . In the beginning of HUT, low-frequency oscillations, i.e., LF, increased more in POTS , but in the end of HUT, an attenuation in LF was seen in the POTS group , but not in the subjects without POTS. There were no associations of previous infections or vaccinations with POTS. Subjects with POTS were sleepier and their overall quality of life was very low.
How Is Postural Orthostatic Tachycardia Syndrome Diagnosed
There’s no single test to diagnose POTS. Doctors start by doing a complete physical exam and taking a medical history.
POTS causes a heart rate increase of 40 or more beats per minute within 10 minutes of when someone moves from a supine position to a standing one. The heart rate goes up dramatically, with little if any drop in blood pressure. Doctors can measure this easily.
Sometimes, doctors do a “tilt-table test.” In this test, a person is strapped to a table, then tilted from a supine position into a standing position while heart rate and blood pressure are monitored.
Doctors also make sure the problem isn’t due to anything besides the autonomic nervous system. Depending on the symptoms, tests might be done on other parts of the body. These might check the blood, heart, brain, eyes, ears, kidneys, muscles, nerves, hormones, digestive tract, and more. Typically, a diagnosis of POTS is confirmed when symptoms have lasted for several months and no other causes are found.
If someone has POTS, the medical team will look for reasons that the autonomic nervous system doesn’t respond normally to standing. Finding an answer can help treatments work well.
You May Like: Why Do Av Nodal Cells Not Determine The Heart Rate
Types And Causes Of Pots
The causes of POTS vary from person to person. Researchers dont entirely understand the origins of this disorder. The classification of POTS is the subject of discussion, but most authorities recognize different characteristics in POTS, which occur in some patients more than others. Importantly, these characteristics are not mutually exclusive person with POTS may experience more than of these at the same time:
Neuropathic POTS is a term used to describe POTS associated with damage to the small fiber nerves . These nerves regulate the constriction of the blood vessels in the limbs and abdomen.
Hyperadrenergic POTS is a term used to describe POTS associated with elevated levels of the stress hormone norepinephrine.
Hypovolemic POTS is a term used to describe POTS associated with abnormally low levels of blood .
Secondary POTS means that POTS is associated with another condition known to potentially cause autonomic neuropathy, such as diabetes, Lyme disease, or autoimmune disorders such as lupus or Sjögrens syndrome.
What Are Everyday Ways To Help Manage Pots
Diet and nutrition
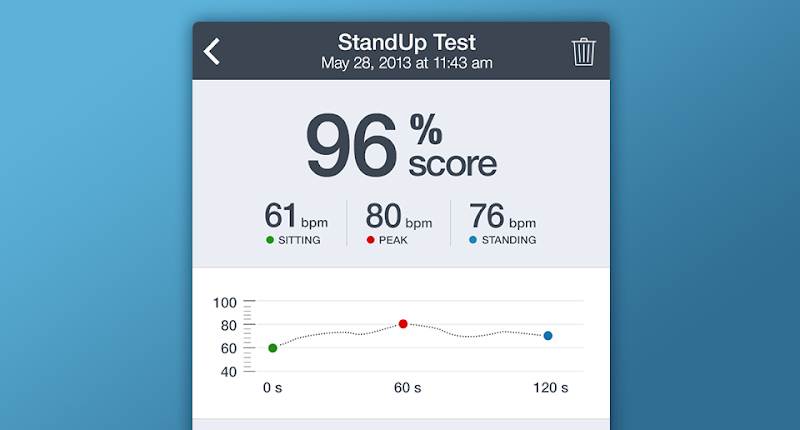
Monitoring POTS
Taking and writing down your vital information can give you insight and better control over your POTS, and helps your doctor fine tune your treatment.
Check blood pressure and pulse at the same time daily . Its very helpful to do this for the first few months of your diagnosis. Also check blood pressure and pulse when you aren’t feeling well.
Heart rate/pulse
Measuring heart rate can give you insight as you deal with POTS. Other facts about heart rate and POTS:
- A normal heart rate is between 60 to 100 beats per minute.
- A fast heart rate over 100 beats per minute can be a condition called tachycardia.
- A slow heart rate under 60 beats per minute is called bradycardia.
- High or low rates can cause symptoms of POTS.
Blood pressure
Blood pressure is the pressure of the blood in the blood vessels in the circulatory system. Blood pressure is related to the heart beating and the diameter and elasticity of the artery walls.
Exercise and physical activity
Exercise and physical activity are key to managing POTS. Here are important things to know as you undergo an exercise program such as cardiac rehab, as well as other physical activities. Talk with your healthcare provider for specific instructions on these exercises.
As you do better with your POTS, more fitness and exercise regimens may be started.
Sleep
Also Check: Benadryl Arrhythmia
