What Does The Heart Do
As described above, the heart pumps a tremendous amount of blood almost nonstop throughout a persons lifetime.
Why is this so? It is because the pumping of the heart is what ensures that the blood flow in the human body is maintained. Without the constant pumping of the heart muscle, blood cant circulate throughout the body.
This means that in the absence of that activity, nutrients wont be able to travel around the body.
Also, oxygen wouldnt be able to reach the various organs within the frame needing it to function.
So, more concisely, cited below, are the significant functions and purposes of the human heart.
- Serves as the primary organ for pumping blood throughout the human body.
- Facilitates the delivery of various materials such as oxygen-rich blood, glucose, and various essential hormones to different locations in the body where they are required.
- It is also instrumental in maintaining the appropriate level of blood pressure required for the body to function correctly.
- Once blood that contains oxygen has been used up and replaced with deoxygenated blood, the heart is responsible for moving it from the right atrium by the tricuspid valve through the channel of the right ventricle straight to the lungs to be replenished and vice versa.
- It primarily serves as a conduit, opening into various major arteries, arterioles, and capillaries that transport fluids and essential materials to multiple regions of the body.
How Do You Calm A Racing Heart
If you think youre having an attack, try these to get your heartbeat back to normal:
Rate Control In The Medical Management Of Atrial Fibrillation
A J CammI SavelievaG Y H Lip
Two main strategies are available for management of atrial fibrillation: rate control and rhythm control.
The aims of heart rate control in atrial fibrillation are to minimise symptoms associated with excessive heart rates and to prevent tachycardiaassociated cardiomyopathy. Rate control involves the use of negatively chronotropic drugs or electrophysiological/surgical interventions to reduce the rapid ventricular rate often found in patients with atrial fibrillation. Although the atria continue to fibrillate, this strategy is considered an effective treatment as it can improve symptoms and reduce the risk of associated morbidity. However, the risk of stroke and occurrence of thromboembolic events occurring is reduced by giving antithrombotic drugs.
Rhythm control involves the use of electrical or pharmacological cardioversion or electrophysiological/surgical interventions to convert the arrhythmia associated with atrial fibrillation to normal sinus rhythm. Patients who have been successfully cardioverted are generally given antiarrhythmic drugs for the long term to help prevent the recurrence of atrial fibrillation. Rhythm control strategies also require the appropriate antithrombotic treatment to reduce the risk of stroke and thromboembolism.
Also Check: Unsafe Heart Rate During Exercise
The Cardiac Electrical System And How The Heart Beats
The electrical system of the heart is critical to how it functions. It determines heart rate and also coordinates and organizes the beating of the heart muscles, so that the heart works efficiently with each heartbeat.
Abnormalities in the hearts electrical system can cause heart rate to be too fast or too slow or entirely disrupt the normal functioning of the hearteven if the hearts muscles and valves themselves are entirely normal.
Talking about the cardiac electrical system and abnormal heart rhythms can be very confusing. When we talk about heart disease, many people think of blocked coronary arteries that can result in a heart attack or the need for bypass surgery. Yet, problems with the electrical system may occur even if your heart muscle is normal.
It’s helpful to picture your heart as a house and the cardiac electrical system as the wiring that provides power throughout the structure. It’s possible to have problems related to faulty wiring even if the building itself is completely normal. Likewise, your heart could be normal but an electrical problem may occur causing an abnormal heart rhythm.
Let’s take a look at how the cardiac electrical system works to make your heart beat, as well as medical conditions which can affect your pulse.
How Fast Does The Normal Heart Beat
How fast the heart beats depends on the body’s need for oxygen-rich blood. At rest, the SA node causes your heart to beat about 50 to 100 times each minute. During activity or excitement, your body needs more oxygen-rich blood the heart rate rises to well over 100 beats per minute.
Medications and some medical conditions may affect how fast your heart-rate is at rest and with exercise.
You May Like: Tylenol Effect On Blood Pressure
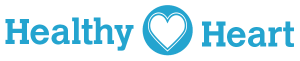
Nervous Regulation: Baroreceptor Reflex
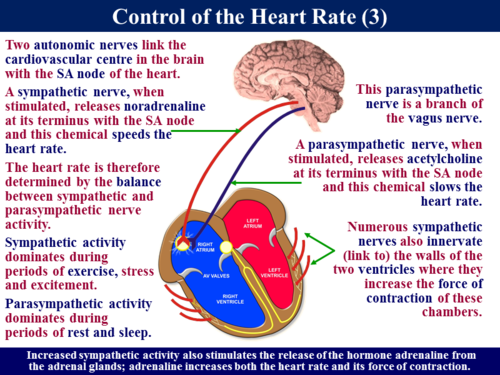
Nervous influences of heart activity are carried through the auto-nomic nervous system. Both sympathetic and parasympathetic nerve fibers innervate the heart and have a major effect on the SA node. Stimulation by sympathetic nerve fibers causes the heart rate and the stroke volume to increase, whereas stimulation by parasympathetic nerve fibers causes the heart rate to decrease.
The baroreceptorreflex is a mechanism of the nervous system that plays an important role in regulating heart function. Baroreceptors are stretch receptors that monitor blood pressure in the aorta and in the wall of the internal carotid arteries, which carry blood to the brain. Changes in blood pressure result in changes in the stretch of the walls of these blood vesselsand changes in the frequency of action potentials produced by the baroreceptors. The action potentials are transmitted along nerve fibers from the stretch receptors to the medulla oblongata of the brain.
Within the medulla oblongata is a cardioregulatory center, which receives and integrates action potentials from the barore-ceptors. The cardioregulatory center controls the action potential frequency in sympathetic and parasympathetic nerve fibers that extend from the brain and spinal cord to the heart. The cardio-regulatory center also influences sympathetic stimulation of the adrenal gland. Epinephrine and norepinephrine, released from the adrenal gland, increase the stroke volume and heart rate.
Read Also: Corpus Callosum Diagram
Regions Of The Brain:
The major regions of the brain are scientifically known as the forebrain, including the telencephalon and diencephalon, the midbrain, including the mesencephalon, and the hindbrain, containing the metencephalon and the myelencephalon. More commonly the brain regions are known as the cerebrum, cerebellum and the brainstem. The cerebrum is the biggest section and has four lobes called the frontal, temporal, parietal and occipital lobes. The brainstem is divided into the midbrain and the pons and medulla oblongata . The cerebellum sits at the base of the brain and the diencephalon resides deep inside of the brain.
Read Also: What Happens Inside The Heart To Cause A Heart Attack
How To Lower Your Resting Heart Rate
In general, people who are more fit and less stressed are more likely to have a lower resting heart rate. A few lifestyle changes can help you slow it down:
- Exercise regularly. It raises your pulse for a while, but over time, exercise makes your heart stronger so it works better.
- Eat right. Losing weight may slow your resting heart rate. And studies have found lower heart rates in men who eat more fish.
- Tackle stress. Set aside time to disconnect from electronic devices and relax each day. Meditation, tai chi, and breathing exercises can also help.
- Stop smoking. Itâs one of the best things you can do for your overall health.
Role Of Chemoreceptors In Increasing Breathing Rate
When we exercise, respiration increases so more carbon dioxide is produced. Carbon dioxide dissolves in the blood to form a weakly acidic solution . The slight decrease in pH that occurs during exercise is detected by special receptors which can detect the presence of chemicals, called chemoreceptors. Chemoreceptors are found in the medulla oblongata, in aortic bodies and in carotid bodies . When blood pH drops, the chemoreceptors are activated and send a nerve impulse to the medulla oblongata. The ventilation centres in the medulla oblongata respond by increasing the frequency of nerve impulses sent to the diaphragm and intercostal muscles. The diaphragm and intercostal muscles contract and relax faster, increasing the rate of breathing.
Recommended Reading: Does Tylenol Help With High Blood Pressure
Control Of Heart Rate:
Action potentials originate in the sinoatrial node and travel across the wall of the atrium to the atrioventricular node on the right side of the heart. This passes slowly giving time for the atria to contract and empty all the blood into the ventricle. This is then passed along the atrioventricular bundle into the interventricular septum along the bundle of His. This bundle separates into two at the apex of the ventricles and goes upwards along each of the ventricle walls. The action potentials travel along this pathway and is carried deeper into the ventricular walls by the Purkinje fibres. This provides unison of a strong contraction by both the ventricles and allowing the ventricles to empty properly.
Chemoreceptors, located in the aorta and the carotid artery, monitor the CO2 levels, O2 levels and pH levels in the blood. When the receptor picks up the stimulant it transfers it to the sensory neurone to the medulla oblongata which also has chemoreceptors. The impulse then travels along the sympathetic neurone or parasympathetic neurone depending on the stimuli to the sinoatrial node. The effector, the cardiac muscle, can have two responses depending on the stimulus and route it takes:
Baroreceptors, located in the carotid artery and aorta only, detect changes in the pressure in the blood. The routes are exactly the same for which the nerve impulses take:
Effect Of Exercise Intensity
Several studies have investigated the effect of exercise intensity on HRV during exercise. In addition to different modalities being utilized between these studies, the duration for which participants exercised at each intensity varies greatly, such as 2 min , 3 min , 5 min , 8 min , 10 min and 15 or more min . Nevertheless, an analysis of the literature allows us to identify some general responses for some HRV measures as a function of exercise intensity.
Time-Domain Measures
Exercise elicits a reduction in HRV when expressed in the time domain, regardless of whether the HRV metric is based on overall HRV calculated from R-R intervals , or beat-to-beat HRV metrics based on the difference in R-R intervals . Several studies have reported that higher exercise intensity is associated with a lower SDRR . Compared to resting values which vary greatly , there is a somewhat consistent intensity dose-response, namely a curvilinear decay to 310 ms for exercise > 160 b.min1. The results of some studies indicate that SDRR reaches a minimum at moderate-high intensity, and does not change substantially thereafter, whereas other studies suggest that small decreases in SDRR continue as intensity is increased toward maximal. Regardless, it is clear that SDRR is drastically reduced as a function of exercise intensity. When natural-log transformed, SDRR demonstrates a somewhat linear decrease as a function of exercise intensity.
Frequency Domain Measures
Recommended Reading: What Causes Left Ventricular Diastolic Dysfunction
Parasympathetic Nervous System And Your Heart
There are a number of special receptors for the PSNS in your heart called muscarinic receptors. These receptors inhibit sympathetic nervous system action. This means theyre responsible for helping you maintain your resting heart rate. For most people, the resting heart rate is between 60 and 100 beats per minute.
On the other hand, the sympathetic nervous system increases heart rate. A faster heart rate pumps more oxygen-rich blood to the brain and lungs. This can give you the energy to run from an attacker or heighten your senses in another scary situation.
According to an article in the journal Circulation from the American Heart Association, a persons resting heart rate can be one indicator of how well a persons PSNS, specifically the vagus nerve, is working. This is usually only the case when a person doesnt take medications that affect heart rate, like beta-blockers, or have medical conditions affecting the heart.
For example, heart failure reduces the response of the parasympathetic nervous system. The results can be an increased heart rate, which is the bodys way of trying to improve the amount of blood it pumps through the body.
Recommended Reading: What Branch Of Medicine Deals With Heart Disease
What Constitutes Adequate Rate Control
The optimal heart rate in atrial fibrillation is not known. Current guidelines define adequate rate control in atrial fibrillation as maintenance of the ventricular rate response between 60 and 80beats/min at rest and between 90 and 115beats/min during moderate exercise. A consensus statement has suggested a target heart rate of < 90 at rest and < 180bpm during exercise in patients with atrial fibrillation. However, no controlled clinical trials have validated these target rates for preventing allcause cardiovascular morbidity or mortality, and such recommendations may be flawed. Few data exist that define the most robust method for the assessment of rate control.
Adequate rate control may encompass more than the prevention of fast ventricular rates. However, few systematic studies have explored the effect of rateslowing drugs on chronotropic competence in atrial fibrillation. The effect of rate regularisation is rarely acknowledged in practice, despite evidence that the mere presence of irregular RR intervals may also contribute to impairment of ventricular haemodynamic function irrespective of heart rate. Furthermore, atrial contraction contributes between 20% and 40% of the total stroke volume. A marked decrease in cardiac output may occur in atrial fibrillation with the loss of atrial contraction, especially in patients with impaired diastolic filling, hypertension and left ventricular hypertrophy.
Table 1Recommendations for rate control
Recommended Reading: Will Tylenol Raise Blood Pressure
Influences From The Central Nervous System
Cardiovascular centres
The heart rate is rhythmically generated by the sinoatrial node. It is also influenced by central factors through sympathetic and parasympathetic nerves. Nervous influence over the heart rate is centralized within the two paired cardiovascular centres of the medulla oblongata. The cardioaccelerator regions stimulate activity via sympathetic stimulation of the cardioaccelerator nerves, and the cardioinhibitory centers decrease heart activity via parasympathetic stimulation as one component of the vagus nerve. During rest, both centers provide slight stimulation to the heart, contributing to autonomic tone. This is a similar concept to tone in skeletal muscles. Normally, vagal stimulation predominates as, left unregulated, the SA node would initiate a sinus rhythm of approximately 100 bpm.
Norepinephrine binds to the beta1 receptor. High blood pressure medications are used to block these receptors and so reduce the heart rate.
Input to the cardiovascular centres
Increased metabolic byproducts associated with increased activity, such as carbon dioxide, hydrogen ions, and lactic acid, plus falling oxygen levels, are detected by a suite of chemoreceptors innervated by the glossopharyngeal and vagus nerves. These chemoreceptors provide feedback to the cardiovascular centers about the need for increased or decreased blood flow, based on the relative levels of these substances.
Cardiac Autonomic Regulation During Exercise And Recovery
Figure 1. Key aspects of cardiovascular autonomic regulation, particularly during exercise and recovery. Blood pressure appears to be the primary regulated variable. Acetylcholine-esterase at the parasympathetic-cardiac junction facilitates rapid On and Off signaling , whereas sympathetic Off effects are substantially slower . Note the indirect nature of HRV and PEP as indices of cardiac parasympathetic and sympathetic activity, respectively, as well as the substantial cross talk of cardiac sympathetic/parasympathetic effects. Also note the common pathways through which different dosages of exercise may influence cardiac autonomic regulation. AC-cAMP-PKA, adenylate-cyclase/cyclic-AMP/Protein-kinase-A cascade ACh, acetylcholine aS, sympathetic outflow to adrenal medulla 1 , Beta1 adrenergic receptors Ca2+, calcium ions cP, cardiac parasympathetic outflow cS, cardiac sympathetic outflow CVLM, caudal ventrolateral medulla E, epinephrine Gi, G-protein inhibitory subunit Gs, G-protein stimulatory subunit HR, heart rate HRV, heart rate variability K+, potassium ions M2, M2 muscarinic receptor MLC, myosin light chain NA, nucleus ambiguus Na+, sodium ions NE, norepinephrine NPY, neuropeptide Y NTS, Nucleus Tractus Solitarii P-, phosphorylation PEP, pre-ejection period PG, parasympathetic ganglia Q, cardiac output RVLM, rostro ventrolateral medulla SG, sympathetic ganglia SV, stroke volume vS, vascular sympathetic outflow.
Recommended Reading: Tylenol Raise Blood Pressure
Health And Performance Considerations
Higher heart rates may be an indication of poor heart function and higher than usual stress being placed on the hearts ability to circulate blood. This may further indicate heart disease conditions.
From a performance stand point knowing specific heart rate training zones can optimize our bodys ability to adapt to performance requirements. Determining these zones can be done through many different methods, including VO2 or lactate testing, formulas and general training regimens. It then becomes necessary to monitor intensity in order to optimize your chances for success. To monitor your intensity there are several methods available to you. First is the perceived exertion method in which you rate your perception of how hard you are exerting yourself during a workout. The acronym for this is RPE . The scale on which to base your perceptions range from 1 – 10. See below.
The scale can be broken down as follows:
Where Is The Medulla Oblongata Located
Your medulla oblongata looks like a rounded bulge at the end of your brain stem, or the part of your brain that connects with your spinal cord. It also lies in front of the part of your brain called the cerebellum.
Your cerebellum looks like a tiny brain joined onto the back of your brain. In fact, its name literally translates to little brain from Latin.
The hole in your skull that lets your spinal cord pass through is called your foramen magnum. Your medulla oblongata is located at about the same level or slightly above this hole.
The top of your medulla creates the floor of the fourth ventricle of your brain. Ventricles are cavities filled with cerebral spinal fluid that help provide your brain with nutrients.
cranial nerves originate on this region.
Your brain and spine communicate through columns of nerve fibers that run through your medulla called spinal tracts. These tracts can be ascending or descending .
Each of your spinal tracts carries a specific type of information. For example, your lateral spinothalamic tract carries information related to pain and temperature.
If part of your medulla becomes damaged, it can lead to an inability to relay a specific type of message between your body and brain. The types of information carried by these spinal tracts include:
- pain and sensation
You May Like: Chronic Systolic Heart Failure Life Expectancy