Hr Models And Parameters
The above analysis shows that AP initiation and propagation could meet the NLARI conditions: a cardiac disturbance , to which modulation of PNS versus SNS activity occur in response, potentially causing the heartbeat to deviate from equilibrium a restoring force that reduces the positive deviation from equilibrium by increasing the relative strength of PNS against SNS activity and a myocardial electrical resistive force that hinders a fast change in heart rate . For these reasons, we introduced the NLARI process in Eq. to understand the control mechanisms of heart rate dynamics. Notice that \t\) if \\). Let \t\) express the removed-mean/tended HR . Equation can be rewritten as
The stability involved in homeostasis has never been explicitly stated. Here we define that the NLARI process in the stable fixed-point range is stable homeostasis. The NLARIs stable fixed point is exponentially asymptotically stable but not globally stable. Formally we introduce the HR models and parameters:
Definition 1. Equation is called the NLARI-HR model . Equation is called the NLARI-HRV responder . The HRV responder in the stable fixed-point range is called the stable homeostatic HRV responder and the noise- or stimulus-driven homeostatic HRV responder for noise or cardiac stress. The HR parameters are assumed to be the physiological indicators as follows:
The restoration coefficient is used to measure the relative strength of PNS against SNS activity as the PNS-SNS activity coefficient
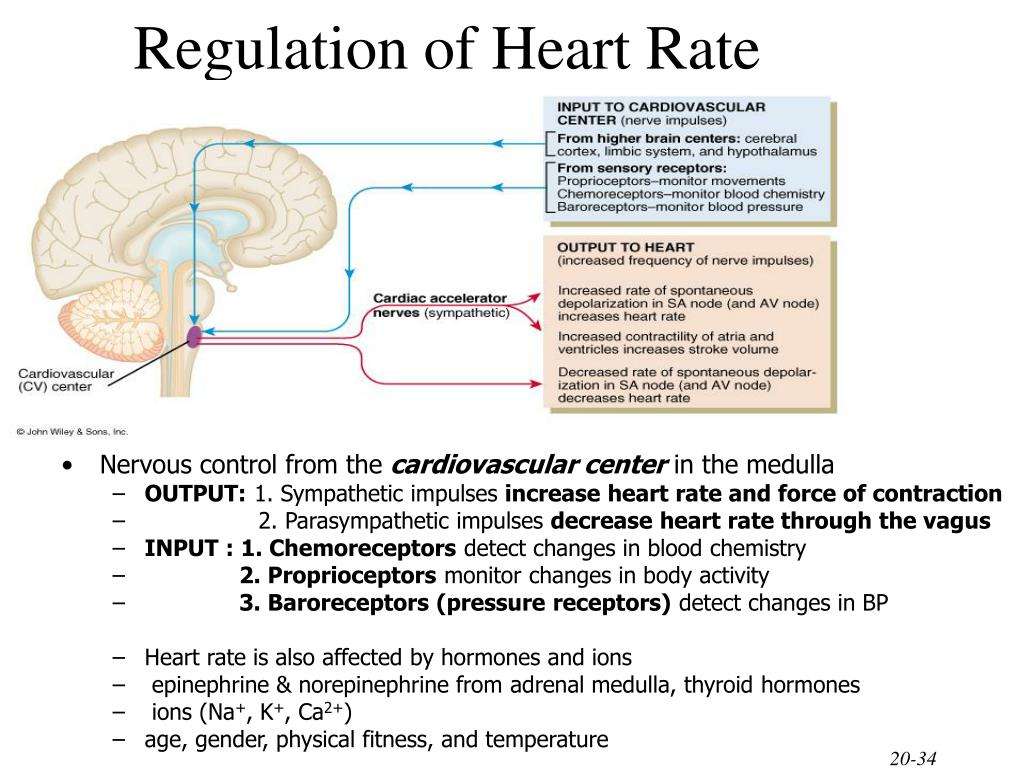
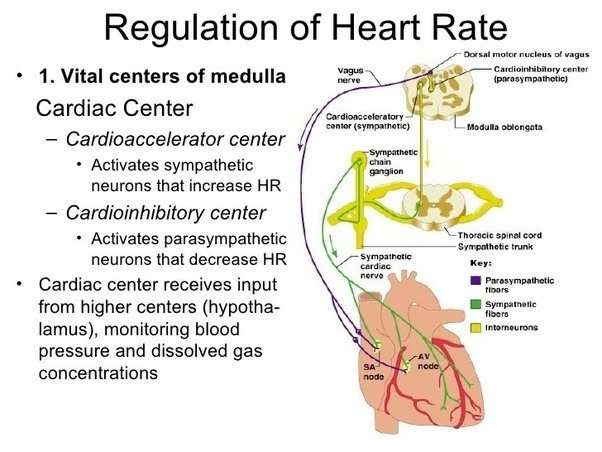
Neural Control Of The Heart Is A Balance Between Sympathetic And Parasympathetic Influences
Heart rate is established by spontaneously depolarizing pacemaker cells in the sinoatrial node, and the rate of depolarization of these pacemaker cells is modulated by parasympathetic and sympathetic neural activity. Under basal resting conditions, heart rate reflects the balance of sympathetic and parasympathetic tone to the heart in humans at rest, parasympathetic tone predominates and therefore resting heart rate is lower than is the intrinsic rate of the sinoatrial node. Due to the basal tonic autonomic control of the heart, heart rate can be increased by reducing parasympathetic activity and/or increasing sympathetic activity the opposite responses slow the heart. These autonomic systems function in an integrated manner, and opposite changes in sympathetic and parasympathetic activity typically occur simultaneously to modulate heart rate.
The basal drive of cardiac sympathetic outflow, like sympathetic outflow to the vasculature, emanates principally from the RVLM, although the factors imparting this tonic discharge of RVLM neurons are not fully understood. Cardiac parasympathetic preganglionic neurons in the brain stem are tonically active in vivo, largely reflecting input from the cardiovascular and respiratory systems. Indeed, heart rate fluctuates in phase with breathing, as a result of changes in cardiac vagal activity.
Javier Gonzalez-Sanchez, … Winslow Burleson, in, 2017
Experimental Animals And Endurance Exercise Protocols
This study was carried out in accordance with the recommendations of the Canadian Council of Animal Care. The protocol was approved by the Division of Comparative Medicine at the University of Toronto and York University Animal Care Committee. 6-week-old CD1 male mice were housed in a room with a constant temperature with a 12-h:12-h light-dark cycle and fed a standard laboratory mouse diet ad libitum with free access to water. Mice were randomly assigned to sedentary or 6-week swimming or free-wheel running groups. For 6-week swim exercised mice, mice swam during the light phase of their light-dark cycle in swim containers at 33°C . To avoid drowning stress associated with the use of tail-weights, bubbling, or detergents, swim exercised mice swam in tanks equipped with pumps to generate steady currents , which we previously showed does not cause plasma elevations in stress hormones . Swim training began with 30-min swim sessions that were increased to 90-min by 10-min increments per day followed by 6 weeks of training. For free-wheel running, cages were equipped with unlocked free-wheels which mice were allowed to voluntarily use over the course of 6 weeks. Speed and daily wheel revolutions were recorded digitally using custom software running on Raspberry Pi computers and distance was calculated by the formula:
Table 1. Physical characteristics of mice.
You May Like: Where Does Blood Low In Oxygen Enter First
Spontaneous Local Ca2+ Releases In Sanc The Primary Hearts Pacemaker
In rabbit SANC, fluorescence imaging over the last decade has documented the occurrence of an AP-induced Ca2+ transient, and, importantly, in the absence of Ca2+ overload, confocal imaging has permitted detection of the occurrence of localized, Ca2+ releases during normal cell function . During spontaneous beating, LCRs occur during late DD in the form of multiple locally propagating wavelets beneath the cell surface membrane , larger than the spontaneous Ca2+ sparks in ventricular cells, but markedly less than well organized Ca2+ waves that can propagate the length of ventricular cells. While LCRs occur during the spontaneous diastolic depolarization in spontaneously firing rabbit SANC, they do not require triggering by the depolarization: spontaneous LCRs in SANC occur in the absence of membrane potential changes, i.e., during voltage clamp , or following chemical skinning of the surface membrane with the detergent saponin . Of note, however, in cat, latent atrial pacemaker cells, T-type Ca2+ current, activated during DD, is thought to trigger LCRs, as these are blocked by 50 M Ni2+ in concentrations that inhibit T-type Ca2+ channels in contrast, in primary rabbit SANC, Ni2+ at these concentrations does not inhibit LCRs .
Heart Rate And Heart Rate Variability In Posttraumatic Disorder
Increased heart rate is a determinant of physiological arousal seen in PTSD. Subjects who develop PTSD have been shown to have higher heart rates during the immediate aftermath of the trauma compared to traumatized individuals who do not develop PTSD. The elevated heart rate is caused by the increased noradrenergic tone, suggesting that increased noradrenergic activity immediately after the trauma may play an important role in the neurobiological processes involved in the development of PTSD. From a clinical perspective, this finding suggests that elevated heart rate immediately after the trauma is a predictor of PTSD.
J.R. Jennings, in, 2007
Recommended Reading: Tylenol Heart Palpitations
How The Heart Beats 24/7
The heart doesn’t stop beating because two opposing mechanisms, the sympathetic and parasympathetic nervous systems, work in sync to regulate the heart rate. The constant beating of the heart is the responsibility of the parasympathetic nervous system. When the sympathetic nervous system is activated, it causes the heart rate to speed up. The parasympathetic system brings the heart rate down again to the background level when the heart rate is high.
In a part of the brain called the medulla, a cardiac center receives information from different parts of the body and decides whether to activate the parasympathetic system to slow the heart rate or to stimulate the sympathetic system to increase the heart rate.
Reduced Basal And Exercise
To investigate how the cellular changes in isolated SAN pacemaker cells influence the heart rates of intact animals, we used ECG telemetry in conscious mice. First, we tested whether pharmacologic blockade of If differently affected the heart rate of mutants and controls using IVA . IVA inhibits f-channels by entering the intracellular side of the channel pore in a manner independent of cAMP binding to the CNBD . In the presence of IVA, blocking of If was comparable in the control and mutant SAN cells . The use of experimental doses of IVA in in vivo pilot experiments showed that IVA-induced heart rate reduction in the control mice was maximal at doses ranging from 3 to 6 mg/kg of body weight . Intraperitoneal administration of 3 or 6 mg/kg IVA caused a significant decrease in heart rate in the controls . In striking contrast, IVA had no effect on heart rate in the mutants , demonstrating that the contribution of If to SAN function was specifically and completely eliminated by the hHCN4573X transgene.
You May Like: Can Ibs Cause Heart Palpitations
Control Of Heart Rate By Camp Sensitivity Of Hcn Channels
See allHide authors and affiliations
Chemicals Regulate Heart Beat
Neurotransmitters are substances or chemicals that activate nerve cells and allow them to communicate with other nerve and muscle cells. Norepinephrine and epinephrine activate the sympathetic nervous system and cause the heart rate to speed up. Acetylcholine stimulates the parasympathetic nervous system and lowers the heart rate. Thyroid hormones, which affect almost all cells in the body, increase the heart rate. During hyperthyroidism, thyroid hormone levels are abnormally high and force the heart to beat at a rate that can harm the heart muscle.
Also Check: Can Antihistamines Cause Heart Palpitations
Applications Of Hr Parameters
We compared the HR parameter estimates in five groups with those in healthy young group. Figure showed the HR parameter alterations in the five conditions on the group-average estimate. We explored the possible relations of HR parameter alterations to cardiac, metabolic, and autonomic nervous functions based on physiological knowledge.
Figure 11
How Does The Body Regulate Heart Rate
A human heart circulates a massive volume of blood over its lifetime, enough to fill a trio of oil supertankers. The blood travels through the four heart chambers. One of these chambers, the right atrium, contains the sinus node, which acts as the pacemaker for the heart. The body’s nervous system, neurotransmitters and hormones regulate the sinus node and play a huge role in how the body regulates heart rate.
Each contraction of the heart muscle regulates the flow of blood in the form of a pulse or heart rate. The pulse is measured in beats per minute. Emotional and physical stress, exercise and other physical activities affect the heart rate because the blood needs to travel faster through the body to cope with the demand for oxygen.
Also Check: Unsafe Heart Rate During Exercise
Young Versus Elder Subjects
Comparison between the HR parameter estimates in the YOUNG and ELDER groups showed that healthy older subjects at rest had increased myocardial electrical resistance coefficient , decreased PNS-SNS activity coefficient , a near zero average value of myocardial metabolism leading primarily to a near zero HR slope indicator , and an ultradepressed standard deviation of myocardial metabolism leading primarily to decreased HR amplitude indicator . These results suggested that aging was related to increased myocardial electrical resistance, decreased PNS-SNS activity , and ultradepressed basal metabolism.
The ELDER parameter alterations suggested that ultradepressed basal metabolic rate related to decreased HRV with aging , because decreased PNS-SNS activity led to increased HRV, rather than decreased HRV , according to the HRV amplitude indicator .
What Is Heart Rate
The cardiovascular system circulates blood throughout the body in order to supply oxygen and other nutrients and to remove waste products. Each time the heart beats blood is pumped out of the heart and into the body to supply oxygen to working muscles or to the lungs for re-oxygenation. Heart rate refers to the number of times the heart beats per minute, and is directly related to the workload being placed on the heart. When the body is in a resting state , resting heart rate is measured. A normal resting heart rate ranges from 60-100 beats per minute . Resting rates higher than 100 bpm suggest that the heart is working too hard to circulate blood, and thus may indicate a serious problem that should be monitored by a physician. Resting rates lower than 60 bpm occur more often with endurance-trained athletes whose bodies are more efficient at utilizing oxygen from the blood.
Don’t Miss: What Causes Left Sided Heart Failure
What Regulates The Fetal Heart Rate
The heart is a muscle with its own pacemaker, conducting system, numerous types of receptors and direct neuronal connections to both the sympathetic and parasympathetic systems.
The overarching mission of the cardiovascular system is to deliver sufficient oxygen to key organs. Heart rate is an important determinant of this mission.
Ultimately, any influence on heart rate is mediated by one or more of these structures. The basic anatomy and physiology of heart rate control are described in physiology textbooks. In the simple schematic diagram shown in Figure 1, factors which increase heart rate are shown on the left and factors which decrease heart rate are on the right. While this summary provides the basics for understanding heart rate regulation, it is important to remember that our understanding of this physiology continues to evolve.
The cardioregulatory center in the medulla oblongata contains an acceleratory center and an inhibitory center. The cardioregulatory center receives input from the central nervous system, reflex pathways and circulating catecholamines. An example of central nervous system influence on the acceleratory response is seen with vibroacoustic stimulation. In response to sudden auditory stimulation, the central nervous system activates the cardioacceleratory center. The cardioacceleratory center increases heart rate directly via sympathetic cardiac nerves which interact with the sinoatrial node to increase the heart rate.
Generation Of Conditional Hhcn4573x Transgenic Mice
We generated transgenic mice with alpha-myosin heavy-chain promoter and Tet-Off systemcontrolled cardiac-specific expression of an engineered HCN4 subunit carrying a human mutation that we had previously identified in a patient with SAN dysfunction . The mutation results in deletion of the CNBD from HCN4 subunits and causes cAMP insensitivity of heterologously coexpressed wild-type HCN4 subunits in a dominant-negative manner . The extent of MHC promoterdriven transgene expression in the murine SAN region was assessed by crossbreeding MHC-tTA promoter mice with mice expressing EGFP under control of a bidirectional tetracycline-response element . Examination of EGFP autofluorescence in excised atria from double-transgenic animals revealed strong signals in central and peripheral SAN areas and acutely isolated SAN pacemaker cells , indicating that MHC-tTA promoter mice are well suited to direct transgene expression to the SAN.
Double-transgenic mutants from both founder lines were born at Mendelian ratios and were viable. Echocardiography showed normal ventricular size and function in the line F mutants , which had detectable levels of hHCN4573X in their ventricles . The left ventricular mass to body weight and atrial mass to body weight ratios were normal as well .
Don’t Miss: What Are The Early Signs Of Congestive Heart Failure
Hhcn4573x Expression Eliminates Camp Sensitivity Of If And Affects San Pacemaker Cell Activity
To characterize the consequences of hHCN4573X expression on the properties of SAN pacemaker cells, we obtained perforated patch-clamp recordings from acutely isolated SAN cells . Compared with controls, If recorded from mutant cells exhibited similar current densities but slower activation kinetics . In addition, If was insensitive to -adrenergic stimulation with isoproterenol across the entire voltage range tested . The If half-activation voltage recorded from mutant SAN cells was about 20 mV more negative than that of control SAN cells and did not respond to ISO stimulation , resulting in an If activation range beyond physiologically relevant diastolic membrane potentials, that is, negative to that spanning the diastolic depolarization . In contrast, the ISO response of the L-type Ca2+ current was unaffected in mutant and control SAN cells .
Properties of If in SAN cells of control and mutant mice
Pacemaker activity and action potential properties in SAN cells of control and mutant mice
Taken together, our data indicate that an hHCN4573Xlinked loss of cAMP sensitivity of f-channels causes impaired basal cellular automaticity and a reduction in the maximum firing rate of SAN pacemaker cells, but no elimination of -adrenergic regulation of cellular automaticity.
Hr And Hr Variability Analysis In Conscious Mice
To assess the effects of exercise on HR and HRV in conscious mice, we inserted ECG telemetry devices into the abdominal cavity. Briefly, the negative lead was tunneled subcutaneously from the thorax to the neck and fixed between the muscles located to the right of the trachea. The positive electrode was sutured to the xiphoid process such that it was located between the liver and the diaphragm in the left upper abdominal region. After 10 days of recovery, mice underwent the swim training protocol. Data analysis on conscious, telemetry-implanted mice was processed using DataQuest A.R.T. Analysis software and ECG recordings were exported to Kubios HRV software and analyzed by performing FFTs, as described above.
Also Check: Heart Attack Grill Blair River
Recording Of Cardiac Sna And
Recordings of cardiac SNA, arterial blood pressure , and left ventricular cardiac function were performed in 12 nondiabetic and 12 type 2 diabetic ZDF rats in vivo, as previously described . In brief, animals were anesthetized with urethane , intubated, and ventilated . A blood sample was taken to measure blood glucose and insulin levels. A left thoracotomy was performed between the first and second rib, exposing the stellate ganglion. The cardiac sympathetic nerve was identified as a branch from the stellate ganglion and was dissected free of surrounding connective tissue. After cutting the nerve, the proximal section was placed on a pair of platinum recording electrodes to measure nerve activity. Consequently, the nerve activity being measured was from the efferent sympathetic nerves. The recorded signal was filtered , amplified, and subsequently passed through an amplitude discriminator to quantify nerve discharge frequency . The raw signal was rectified and integrated online, and the integrated nerve signal was displayed in real time. At the end of the experiments, a postmortem nerve activity measurement was performed for background subtraction of noise level, which was not different between groups.
Baseline cardiac SNA was recorded, and administration of dobutamine tested the in vivo cardiac response to -AR stimulation.
Role Of Cardiac Pacemaker
The sinus node is called the cardiac pacemaker as it regulates cardiac contractility and thus, the heart rate. The sinus node is a small ellipsoidal strip of specialized cardiac muscles located in the superior corner of the right atrium.
The cells in the sinus node have automatic electrical rhythmicity. Certain sodium channels are present in these cells that allow the slow diffusion of sodium ions from the extracellular environment into the cells. This inflow of sodium ions causes depolarization in the absence of any electrical stimulus.
The rhythmic cardiac impulses generated in the sinus node are spread to the rest of the cardiac muscles via the conduction system. The rate of impulse generation in the sinus node controls the heart rate. This automatic rhythmicity of the sinus node is controlled by the innervation from the sympathetic and parasympathetic nervous systems.
Also Check: What Causes Left Ventricular Systolic Dysfunction
