Evaluation With Cardiac Imaging
Recommendations for Evaluation With Cardiac Imaging
Referenced studies that support the recommendations are summarized in the .
| COR | |
|---|---|
| C-LD | |
| 1. |
In patients with suspected or new-onset HF, or those presenting with acute decompensated HF, a chest x-ray should be performed to assess heart size and pulmonary congestion and to detect alternative cardiac, pulmonary, and other diseases that may cause or contribute to the patients symptoms . |
1C-LD
| 2. |
In patients with suspected or newly diagnosed HF, transthoracic echocardiography should be performed during initial evaluation to assess cardiac structure and function . |
1C-LD
| 3. |
In patients with HF who have had a significant clinical change, or who have received GDMT and are being considered for invasive procedures or device therapy, repeat measurement of EF, degree of structural remodeling, and valvular function are useful to inform therapeutic interventions . |
1C-LD
| 4. |
In patients for whom echocardiography is inadequate, alternative imaging is recommended for assessment of LVEF . |
2aB-NR
| B-NR | |
| 1. |
In ambulatory or hospitalized patients with HF, validated multivariable risk scores can be useful to estimate subsequent risk of mortality . |
Synopsis
Table 8 Selected Multivariable Risk Scores to Predict Outcome in HF
| Risk Score |
|---|
| 2010 |
Recommendation-Specific Supportive Text
| 1. |
Heart Failure Criteria Classification And Staging
Guideline contributor: Henry H Ooi, MD, MRCPI, Director, Advanced Heart Failure and Cardiac Transplant Program, Nashville Veterans Affairs Medical Center Assistant Professor of Medicine, Vanderbilt University School of Medicine.
Heart failure criteria, classification, and staging
Framingham classification
In the Framingham classification, the diagnosis of heart failure is based on the concurrent presence of either two major criteria or one major and two minor criteria.
Major criteria comprise the following:
- Paroxysmal nocturnal dyspnea
- Weight loss of 4.5 kg or more in 5 days in response to treatment
- Neck vein distention
- Central venous pressure greater than 16 cm water
- Circulation time of 25 seconds or longer
- Radiographic cardiomegaly
- Pulmonary edema, visceral congestion, or cardiomegaly at autopsy
Minor criteria are as follows:
- Nocturnal cough
- A decrease in vital capacity by one third the maximal value recorded
- Pleural effusion
- Bilateral ankle edema
New York Heart Association classification
The NYHA functional classification of heart failure is widely used in practice and in clinical studies. It is based on symptom severity and the amount of exertion needed to provoke symptoms. NYHA heart failure classes are as follows :
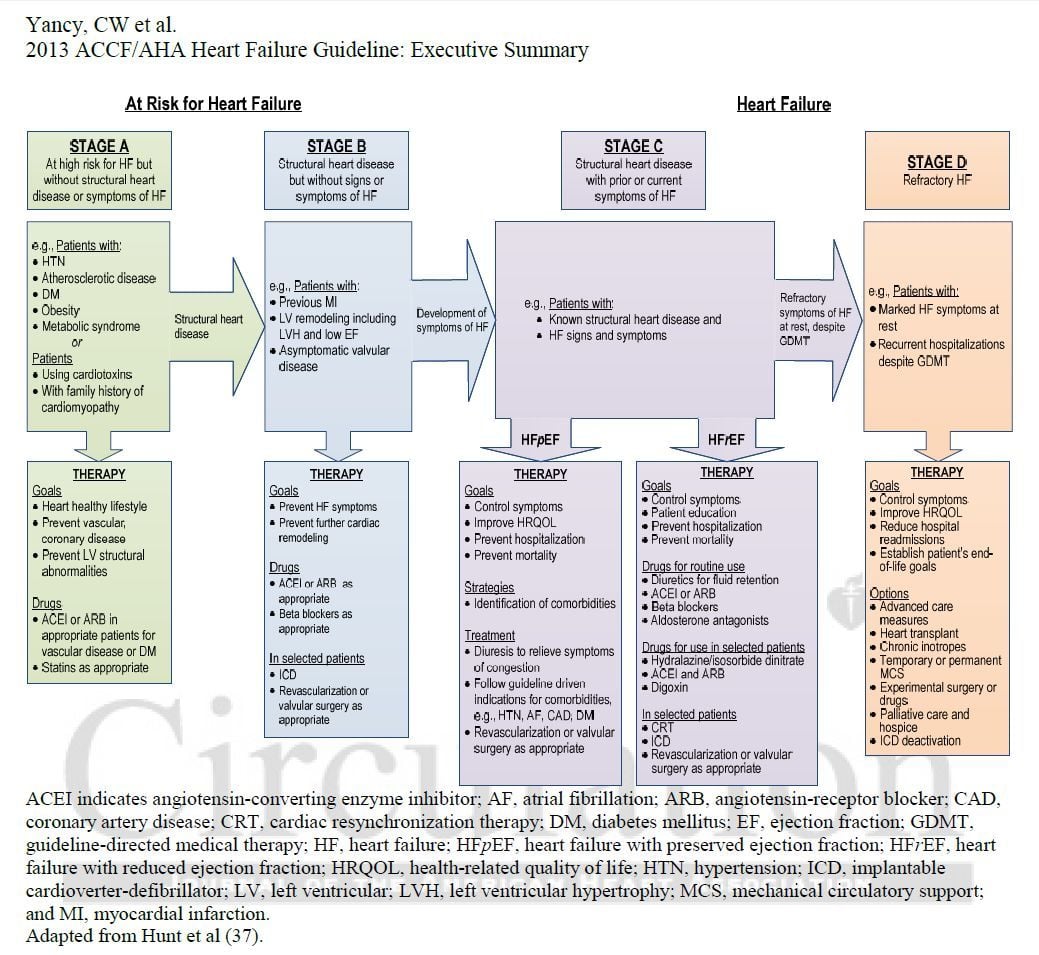
American College of Cardiology Foundation/American Heart Association staging systems
The 2013 ACCF/AHA staging system complements the NYHA classification to reflect the progression of disease and comprises four stages, as shown in Table 3. below.
How To Address Challenges Of Care Coordination
Delivering optimal patient-centered HF care is complex. The range of treatments available, particularly those for patients with HFrEF, include multiple medications, cardiac devices, surgery, and lifestyle adaptations, all of which require education, monitoring, and engagement. For example, patients with HFrEF frequently require consultative care delivered by electrophysiology specialists to implant, monitor, and adjust devices such as implantable cardioverter-defibrillator or cardiac resynchronization therapy devices. As outlined in , the complexity of HF care is further exacerbated by the frequent coexistence of both cardiac and noncardiac comorbidities found in patients with HF. Comorbidities are particularly common in the elderly. More than 50% of patients with HF on Medicare have 4 or more non-CV comorbidities and more than 25% have 6 or more . The care needs for comorbidities can complicateand in some cases preventthe optimal use of HF therapies. Finally, the medical complexity inherent in most patients with HF generally requires the involvement of multiple clinicians across many care settings . This raises the risk of inefficiencies in care delivery, miscommunication, potential drugdrug interactions and drugdisease interactions, and missed opportunities to achieve optimal HF outcomes.
Table 7 Essential Skills for an HF Team
|
Coordination of care for concomitant comorbidities |
HF = heart failure.
| Modality |
|---|
|
Prompts for medication and lifestyle adherence |
Don’t Miss: Does Drinking Increase Heart Rate
Esc Clinical Practice Guidelines
The aim of this ESC guideline is to help health professionals manage people with heart failure according to the best available evidence. Fortunately, we now have a wealth of clinical trials to help us select the best management to improve the outcomes for people with HF for many, it is now both preventable and treatable. This guideline provides practical, evidence-based recommendations. The format of the previous 2016 ESC HF Guidelines was revised to make each phenotype of HF stand-alone in terms of its diagnosis and management. The therapy recommendations mention the treatment effect supported by the class and level of evidence and are presented in tables. In this guideline, we have decided to focus on the diagnosis and treatment of HF, not on its prevention.
Guidelines and related materials are for use by individuals for personal or educational purposes. No commercial use is allowed. Re-use permission must be correctly obtained .
Acc/aha/hfsa Guideline For The Management Of Heart Failure
On April 1, 2022, a new joint guideline for the management of heart failure was published from the American College of Cardiology, the American Heart Association, and the Heart Failure Society of America.
The 2022 ACC/AHA/HFSA Guideline for the Management of Heart Failure increases the focus on preventing HF, updates treatment strategies for people with symptomatic heart failure to include SGLT-2 inhibitor medicines and emphasizes care coordination with a heart failure specialty team. The guideline also offers recommendations for managing cardiac amyloidosis, cardio-oncology complications, comorbidities in the setting of heart failure, as well as consideration for implantable devices and advanced therapies for people with stage D heart failure.
Supplemental resources to help you apply the guidelines to your practice are available to download below.
Also Check: How To Lower Heart Rate On Vyvanse
Value Statement: Sglt2 Inhibitors In Hfref
A key addition to the updated guideline is the incorporation of value statements for select recommendations.1 The guideline includes a value statement for its class 1a recommendation for the use of SGLT2 inhibitors in patients with symptomatic chronic HFrEF that is based upon the results of 2 model-based economic evaluations of the use of dapagliflozin.13,14 Recognizing the wide range of costs currently associated with dapagliflozin, guideline authors indicate that treatment with SLGT2 inhibitors in this patient population provides intermediate economic value.1
Heart Failure Guideline Updates In 2021
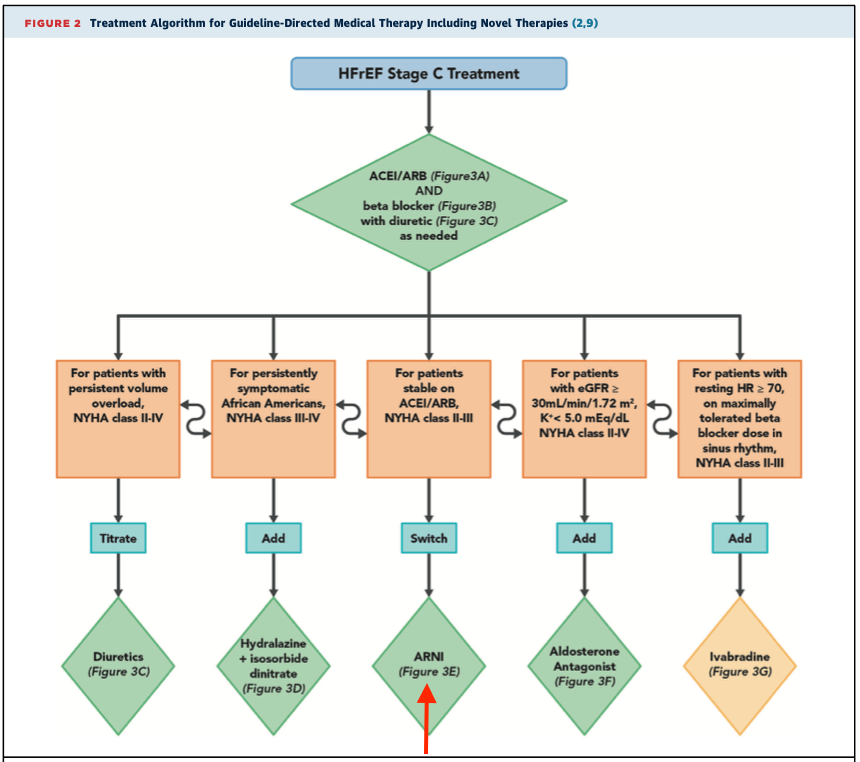
There are a few important heart failure guideline updates in the works to the American College of Cardiologys Heart Failure Guidelines, last published in 2013. Prior to the full guideline release, the organization recently printed their updated Expert Consensus Decision Pathway for treatment of patients with heart failure with reduced ejection fraction . This document serves as up-to-date interim guidance until the full guideline is released.
With regard to medications and guideline-directed medical therapy , two major changes appear as considerations for patients with Stage C HFrEF based on data from new studies. The angiotensin receptor neprilysin inhibitor sacubitril/valsartan is now preferred compared to ACEI/ARBs and sodium-glucose cotransporter-2 inhibitors are now an option for patients with or without diabetes after ARNI/ACEI/ARB and BB treatment has started.
The clinicians toolkit of medications in HFrEF is growing. Many of these agents have shown additive morbidity and mortality benefits on top of the gold-standard ARNI/ACEI/ARB and BB and should be added when possible for patients who qualify. See the ACCs flowchart below for an updated guide to GDMT for stage C HFrEF. Additionally, always remember to check patients medication list for drugs to avoid in heart failure!
Have you seen ARNIs used prior to ACEI/ARBs or SGLT2 inhibitors in HFrEF in advance of or since the recent heart failure guideline updates? Comment below!
You May Like: How Accurate Is Fitbit Heart Rate
Acc Foundation/aha Guidelines For Screening And Genetic Testing For Dcm
Familial DCM
- First-degree relatives not known to be affected should undergo periodic, serial echocardiographic screening with assessment of LV function and size.
- Although the screening frequency is uncertain, every 3-5 years is reasonable.
- Consider genetic testing in conjunction with genetic counseling.
- Inform first-degree relatives of index diagnosis.
- Relatives should discuss with their clinicians whether they should undergo echocardiographic screening.
- Although the value of genetic testing is unclear in this setting, it is potentially valuable in patients with significant cardiac conduction disease and/or a family history of premature sudden cardiac death.
Acc Aha And Hfsa Partner To Release 2022 Heart Failure Guidelines
Released on the eve of ACC.22, the 2022 heart failure guidelines represent a collaborative effort by the ACC/AHA/HFSA and include major additions, including a new focus on the use of SGLT2 inhibitors and revisions to the ACC/AHA stages of heart failure.
The American College of Cardiology, American Heart Association, and Heart Failure Society of America have released a new joint guideline outlining evidence-based strategies for prevention, diagnosis, and management of heart failure.
One primary goal with the new guideline was to use recently published data to update our recommendations for the evaluation and management of heart failure, said Paul A. Heidenreich, MD, MS, guideline writing committee chair, in a statement from the American College of Cardiology. One focus was prevention of heart failure through optimizing blood pressure control and adherence to a healthy lifestyle.
Published on April 1, which is just a day prior to the start of the American College of Cardiologys 71st annual Scientific Session , the 159-page document broken down into 14 sections with multiple subsections and cites more than 700 reference documents. Composed by Heidenreich and a team of more than 50 fellow authors, the guideline is based on an evidence review of relevant studies and data published through September 2021.
You May Like: Best Food For Heart Failure
Classification Of Hf By Left Ventricular Ejection Fraction
LVEF is considered important in the classification of patients with HF because of differing prognosis and response to treatments and because most clinical trials select patients based on ejection fraction . RCTs with evidence of survival benefit in patients with HF have mainly enrolled patients with HF with an LVEF 35% or 40%, often labeled HF with reduced ejection fraction . In this guideline, HFrEF is defined as LVEF 40% . HF with preserved EF represents at least 50% of the population with HF, and its prevalence is increasing . HFpEF has been variably classified as LVEF > 40%, > 45%, or 50%. Because some of these patients do not have entirely normal LVEF but also do not have major reduction in systolic function, the term preserved EF has been used. In this guideline, the threshold for HFpEF is an LVEF 50% .
Table 4 Classification of HF by LVEF
| Type of HF According to LVEF | Criteria |
|---|
|
Previous LVEF 40% and a follow-up measurement of LVEF > 40% |
|
LVEF 41%49% |
|
|
Evidence of spontaneous or provokable increased LV filling pressures |
|
LVEF 50% |
|
|
Evidence of spontaneous or provokable increased LV filling pressures |
Please see for suggested thresholds for structural heart disease and evidence of increased filling pressures.
HF indicates heart failure LV, left ventricular and LVEF, left ventricular ejection fraction.
Figure 3
Classification and Trajectories of HF Based on LVEF
Universal Definition And Classification Of Heart Failure: A Step In The Right Direction From Failure To Function
- A
Quick Takes
- The proposed universal definition describes HF as a clinical syndrome with symptoms and/or signs caused by a structural and/or functional cardiac abnormality and corroborated by elevated natriuretic peptide levels and/or objective evidence of pulmonary or systemic congestion.
- HF stages have been revised to emphasize symptomatic nature of HF as a clinical syndrome: At risk for HF , PreHF , Symptomatic HF and Advanced HF .
- Classification of HF according to LVEF now includes:
- HFrEF: symptomatic HF with LVEF 40%
- HFmrEF: symptomatic HF with LVEF 41-49%
- HFpEF: symptomatic HF with LVEF 50%
- HFimpEF: symptomatic HF with a baseline LVEF 40%, a 10-point increase from baseline LVEF, and a second measurement of LVEF > 40%
A revised classification of HF by left ventricular ejection fraction was also proposed and is as follows:
Figure 1. Courtesy of Gibson GT, Blumer V, Mentz RJ, Lala A.
Figure 1
The new Universal Definition and Classification of HF represents a landmark advancement in our field. The standardization of the definition of HF is valuable for several reasons:
References
Don’t Miss: Why Is It Important To Know Your Resting Heart Rate
Acc/aha Joint Committee Members
Joshua A. Beckman, MD, MS, FAHA, FACC, Chair
Patrick T. OGara, MD, MACC, FAHA,Immediate Past Chair
Sana M. Al-Khatib, MD, MHS, FACC, FAHA
Anastasia L. Armbruster, PharmD, FACC
Kim K. Birtcher, PharmD, MS, AACC
Joaquin E. Cigarroa, MD, FACC
Lisa de las Fuentes, MD, MS, FAHA
Anita Deswal, MD, MPH, FACC, FAHA
Dave L. Dixon, PharmD, FACC
Lee A. Fleisher, MD, FACC, FAHA
Federico Gentile, MD, FACC
Zachary D. Goldberger, MD, FACC, FAHA
Bulent Gorenek, MD, FACC
Adrian F. Hernandez, MD, MHS
Mark A. Hlatky, MD, FACC, FAHA
José A. Joglar, MD, FACC, FAHA
W. Schuyler Jones, MD, FACC
Joseph E. Marine, MD, FACC
Daniel B. Mark, MD, MPH, FACC, FAHA
Debabrata Mukherjee, MD, FACC, FAHA
Latha P. Palaniappan, MD, MS, FACC, FAHA
Tanveer Rab, MD, FACC
Erica S. Spatz, MD, MS, FACC
Jacqueline E. Tamis-Holland, MD, FAHA, FACC
Duminda N. Wijeysundera, MD, PhD
Y. Joseph Woo, MD, FACC, FAHA
Former Joint Committee member current member during the writing effort.
How To Achieve Optimal Therapy Given Multiple Drugs For Hf Including Augmented Clinical Assessment That May Trigger Additional Changes In Gdmt
5.2.1 Target Doses
To achieve the maximal benefits of GDMT in patients with chronic HFrEF, therapies must be initiated and titrated to maximally tolerated doses . Doses of GDMT higher than those studied in randomized clinical trials, even if tolerated, are not known to provide incremental benefits, and are generally not recommended.
Strategies for titration are detailed in and . Achieving target or maximally tolerated doses of GDMT is the goal of titration. Beta-blocker doses should be adjusted every 2 weeks in a patient with no evidence of decompensated HF and no contraindications to higher doses. Longer time periods may be needed for frail patients or those with marginal hemodynamics, whereas more rapid titration may be reasonable in clinically stable patients without hypotension. Following adjustment, patients should be cautioned that there may be a transient worsening of HF symptoms such as dyspnea, fatigue, erectile dysfunction, or dizziness.
For several reasons, HYD/ISDN-indicated therapy for HF is often neglected in eligible patients. However, given the benefits of this combination and the favorable impact on health status , African-American patients should receive these drugs once target or maximally tolerated doses of beta-blocker, ARNI/ACEI/ARB, and aldosterone antagonists are achieved . This combination of drugs is especially important for those patients with NYHA class III to IV symptoms.
5.2.2 Barriers to Medication Titration
5.2.3 Clinical Assessment
Also Check: What Causes Congestive Heart Failure
Heart Failure Society Of America Recommendations For Genetic Evaluation Of Cardiomyopathy
Note the following :
- For all patients with cardiomyopathy, obtain a detailed family history for at least 3 generations
- Carefully assess the patients medical history as well as that of asymptomatic first-degree relatives, with special focus on heart failure symptoms, arrhythmias, presyncope, and syncope.
- Screen asymptomatic first-degree relatives for cardiomyopathy
- Screen for cardiomyopathy at intervals in asymptomatic at-risk relatives who are known to carry the disease-causing mutation 00174-0/fulltext#sec18.1 rel=nofollow> HFSA Guideline Approach to Medical Evidence for Genetic Evaluation of Cardiomyopathy )
- Screen for cardiomyopathy in asymptomatic at-risk first-degree relatives who have not undergone genetic testing or in whom a disease-causing mutation has not been identified.
Note: Due to the complexity of genetic evaluation, testing, and counseling of patients with cardiomyopathy, it is recommended that patients be referred to centers with expertise in these matters and in family-based management.
Relationships With Industry And Other Entities
The ACC and AHA have rigorous policies and methods to ensure that documents are developed without bias or improper influence. The complete policy on relationships with industry and other entities can be found online. of the guideline lists writing committee members relevant RWI for the purposes of full transparency, their comprehensive disclosure information is available in a . Comprehensive disclosure information for the Joint Committee is also available online.
Don’t Miss: What Foods Should Be Avoided With Congestive Heart Failure
The Role Of Sglt2 Inhibitors In Patients At Risk For Hf
In patients with T2D who have or are at high risk for CVD, SGLT2 inhibitors have a class 1 recommendation to prevent HF-related hospitalizations.1 Such patients are at risk for HF . The recommendation is based on results from the randomized CANVAS program, DECLARE-TIMI 58, and EMPA-REG OUTCOME clinical trials, which examined the impact of SGLT2 inhibitor therapy on HF-related hospitalizations in this patient population.6-8
The 2022 HF guideline notes that HF was present at baseline in approximately only 10% to 14% of participants in these trials.1,6-8 Thus, prevention of primary HF symptoms accounted for most of the reduction of HF-related hospitalizations following SGLT2 inhibitor therapy.1 The recommendation for the use of SGLT2 inhibitors in patients at risk for HF due to T2D and established or high risk of CVD also applies to patients with pre-HF, as management strategies instituted in stage A should be continued through stage B .
Palliative And Supportive Care Shared Decision
Recommendations for Palliative and Supportive Care, Shared Decision-Making, and End-of-Life
Referenced studies that support the recommendations are summarized in the Online Data Supplements.
| COR | |
|---|---|
| C-LD | |
| 1. |
For all patients with HF, palliative and supportive careincluding high-quality communication, conveyance of prognosis, clarifying goals of care, shared decision-making, symptom management, and caregiver supportshould be provided to improve QOL and relieve suffering. |
1C-LD
| 2. |
For patients with HF being considered for, or treated with, life-extending therapies, the option for discontinuation should be anticipated and discussed through the continuum of care, including at the time of initiation, and reassessed with changing medical conditions and shifting goals of care . |
2aB-R
| 3. |
For patients with HFparticularly stage D HF patients being evaluated for advanced therapies, patients requiring inotropic support or temporary mechanical support, patients experiencing uncontrolled symptoms, major medical decisions, or multimorbidity, frailty, and cognitive impairmentspecialist palliative care consultation can be useful to improve QOL and relieve suffering. |
2aC-LD
| 4. |
For patients with HF, execution of advance care directives can be useful to improve documentation of treatment preferences, delivery of patient-centered care, and dying in preferred place. |
2aC-LD
Also Check: What Are The Signs And Symptoms Of A Heart Attack
