Acc/aha/hfsa Guideline For The Management Of Heart Failure
On April 1, 2022, a new joint guideline for the management of heart failure was published from the American College of Cardiology, the American Heart Association, and the Heart Failure Society of America.
The 2022 ACC/AHA/HFSA Guideline for the Management of Heart Failure increases the focus on preventing HF, updates treatment strategies for people with symptomatic heart failure to include SGLT-2 inhibitor medicines and emphasizes care coordination with a heart failure specialty team. The guideline also offers recommendations for managing cardiac amyloidosis, cardio-oncology complications, comorbidities in the setting of heart failure, as well as consideration for implantable devices and advanced therapies for people with stage D heart failure.
Supplemental resources to help you apply the guidelines to your practice are available to download below.
Heart Failure Society Of America Recommendations For Genetic Evaluation Of Cardiomyopathy
Note the following :
- For all patients with cardiomyopathy, obtain a detailed family history for at least 3 generations
- Carefully assess the patient’s medical history as well as that of asymptomatic first-degree relatives, with special focus on heart failure symptoms, arrhythmias, presyncope, and syncope.
- Screen asymptomatic first-degree relatives for cardiomyopathy
- Screen for cardiomyopathy at intervals in asymptomatic at-risk relatives who are known to carry the disease-causing mutation 00174-0/fulltext#sec18.1″ rel=”nofollow”> HFSA Guideline Approach to Medical Evidence for Genetic Evaluation of Cardiomyopathy )
- Screen for cardiomyopathy in asymptomatic at-risk first-degree relatives who have not undergone genetic testing or in whom a disease-causing mutation has not been identified.
Note: Due to the complexity of genetic evaluation, testing, and counseling of patients with cardiomyopathy, it is recommended that patients be referred to centers with expertise in these matters and in family-based management.
New Hf Definition Stage Updates Outlined In 2022 Acc/aha/hfsa Guidelines
The new guidelines also call for better incorporation and addressing of social determinants of health.
During a panel at the American College of Cardiologys 70th Scientific Session, experts highlighted updates to the 2022 American Heart Association /ACC/Heart Failure Society of America guidelines for the management of heart failure and offered a new definition of the condition.
The syndrome of HF is defined as a complex clinical syndrome with symptoms and signs that result from structural or functional impairment, said Biykem Bozkurt, MD, PhD, guideline writing committee vice-chair and professor of Medicine-Cardiology at Baylor College of Medicine.
With regard to terminologies for HF trajectory, the guidelines emphasized the use of persistent HF as opposed to stable HF, as the term stable creates inertia, while persistent HF requires optimization, Bozkurt added. The phrase HF in remission is also preferred over HF in recovery as the majority of patients who withdraw from therapy will relapse.
Among the updates included are a redefinition of HF stages to emphasize prevention and the addition of sodiumglucose co-transporter 2 inhibitors for the treatment of symptomatic HF.
This latter inclusion comes off the heels of an FDA approval for empagliflozin, for a broader range of patients with HF, including those with preserved ejection fraction a condition with a poor prognosis and very limited treatment options.
Recommended Reading: What Age Can You Have A Heart Attack
Document Review And Approval
This document was reviewed by 2 official reviewers nominated by the AHA 1 official reviewer nominated by the ACC 2 official reviewers from the HFSA 1 official Joint Committee on Clinical Practice Guidelines reviewer and 32 individual content reviewers. Reviewers RWI information was distributed to the writing committee and is published in this document .
This document was approved for publication by the governing bodies of the ACC, AHA, and HFSA.
European Society Of Cardiology Guidelines For Genetic Counseling And Testing
Arrhythmogenic cardiomyopathy
Offer genetic counseling and testing all patients with suspected ACM and all first-degree adult relatives of patients with ACM and a disease-causing mutation, regardless of their phenotype to preclinically identify genetically affected individuals.
Genetic family screening may also be used for arrhythmic risk stratification.
First-degree relatives with the same definite disease-causing mutation as the patient should undergo clinical evaluation, electrocardiography , echocardiography, and possibly cardiac magnetic resonance imaging . In the setting of no definite identified genetic mutation in the patient or no genetic testing is undertaken, consider clinical evaluation in first-degree adult relatives with ECG and echocardiography, and repeat every 2-5 years or less if nondiagnostic abnormalities are present.
Dilated cardiomyopathy or hypokinetic nondilated cardiomyopathy
All patients with suspected DCM or HNDC and all first-degree adult relatives of such patients and a definite disease-causing mutation, regardless of their phenotype, should undergo genetic counseling and testing to preclinically identify genetically affected individuals. Repeat the evaluation every 5 years or less in first-degree adult relatives when aged younger than 50 years or in the presence of nondiagnostic abnormalities.
All first-degree relatives of patients should undergo clinical evaluation, ECG, echocardiography, and possibly CMRI.
Hypertrophic cardiomyopathy
Also Check: Cough Congestive Heart Failure
Expert Decision Pathway For Hfref Treatment Optimization
Jan 11, 2021 | Supriya Shore, MD
- Maddox TM, Januzzi JL Jr, Allen LA, et al.
- Citation:
- 2021 Update to the 2017 ACC Expert Consensus Decision Pathway for Optimization of Heart Failure Treatment: Answers to 10 Pivotal Issues About Heart Failure With Reduced Ejection Fraction: A Report of the American College of Cardiology Solution Set Oversight Committee. J Am Coll Cardiol 2021 Jan 11:.
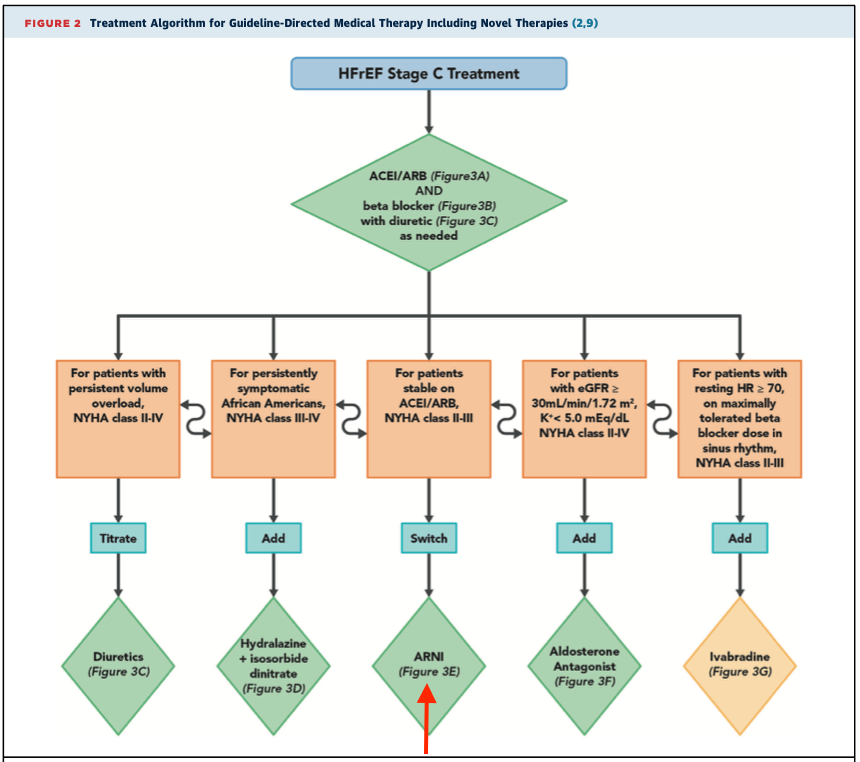
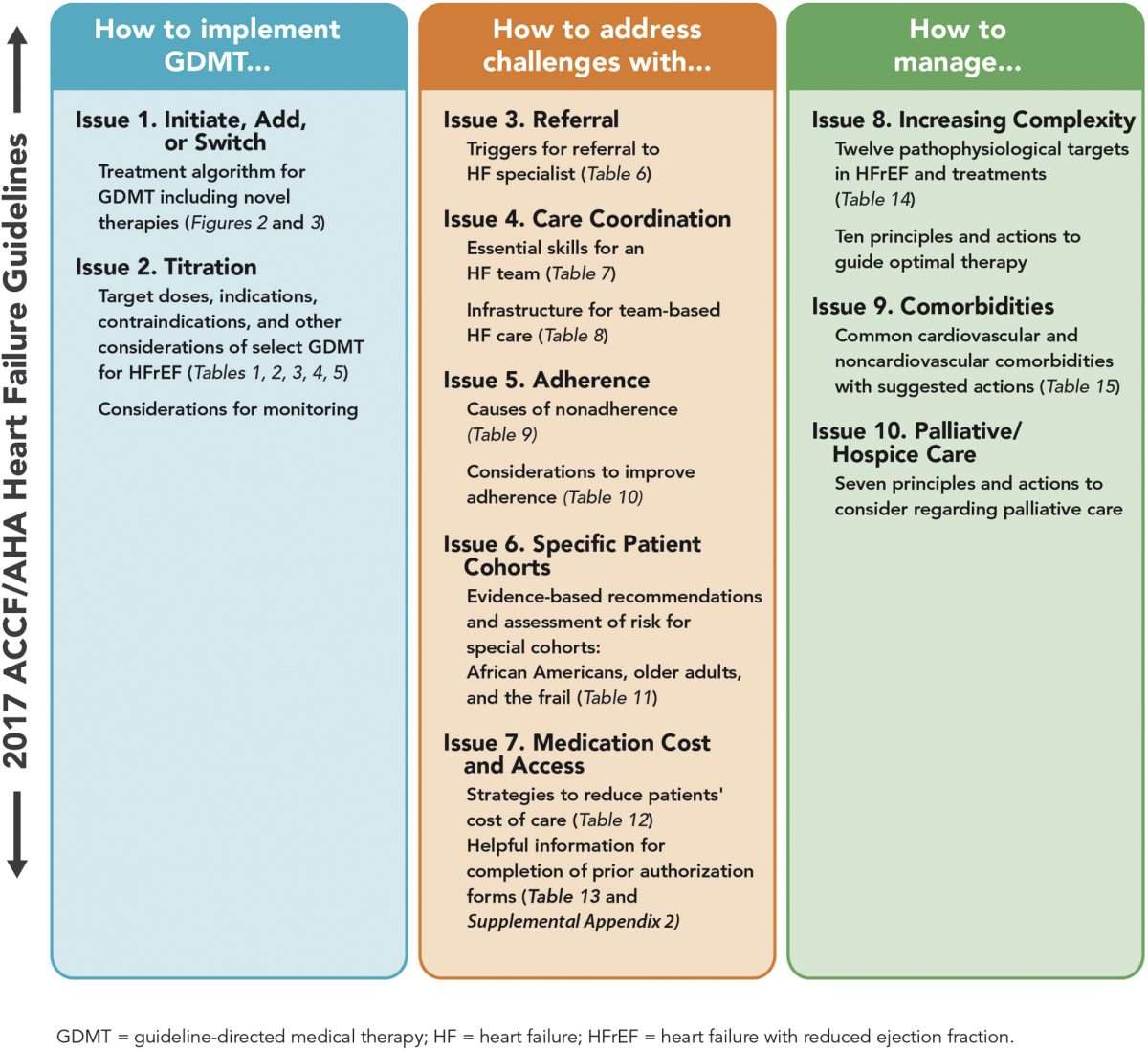
The following are key points to remember from the 2021 Update to the 2017 ACC Expert Consensus Decision Pathway for Optimization of Heart Failure Treatment:
Assessment Of Functional Capacity
The ACCF/AHA indicates the 6-minute walk test may be indicated in patients with heart failure whose adequacy of rate control is in question the HFSA indicates it is a good indicator of functional status and prognosis in patients with heart failure.
The ACCF/AHA and HFSA do not recommend routine maximal exercise stress testing. HFSA guidelines indicate it may be useful in situations such as the following with measurement of gas exchange :
- To assess the disparity between symptomatic limitation and objective indicators of disease severity
- To distinguish non HF-related causes of functional limitation, specifically cardiac versus pulmonary
- To consider whether patients are candidates for cardiac transplantation or mechanical circulatory support
- To determine the prescription for cardiac rehabilitation
ACCF/AHA and ESC guidelines note that values of peak oxygen consumption of less than 50% of predicted or less than 14 mL/kg/min reflect poor cardiac performance and a likelihood of 1-year survival less than 50%, facilitating referral for cardiac transplantation or mechanical circulatory device placement.
You May Like: Under Resting Conditions, Heart Rate Is Primarily Under The Control Of What Control System
How To Achieve Optimal Therapy Given Multiple Drugs For Hf Including Augmented Clinical Assessment That May Trigger Additional Changes In Gdmt
5.2.1 Target Doses
To achieve the maximal benefits of GDMT in patients with chronic HFrEF, therapies must be initiated and titrated to maximally tolerated doses . Doses of GDMT higher than those studied in randomized clinical trials, even if tolerated, are not known to provide incremental benefits, and are generally not recommended.
Strategies for titration are detailed in and . Achieving target or maximally tolerated doses of GDMT is the goal of titration. Beta-blocker doses should be adjusted every 2 weeks in a patient with no evidence of decompensated HF and no contraindications to higher doses. Longer time periods may be needed for frail patients or those with marginal hemodynamics, whereas more rapid titration may be reasonable in clinically stable patients without hypotension. Following adjustment, patients should be cautioned that there may be a transient worsening of HF symptoms such as dyspnea, fatigue, erectile dysfunction, or dizziness.
For several reasons, HYD/ISDN-indicated therapy for HF is often neglected in eligible patients. However, given the benefits of this combination and the favorable impact on health status , African-American patients should receive these drugs once target or maximally tolerated doses of beta-blocker, ARNI/ACEI/ARB, and aldosterone antagonists are achieved . This combination of drugs is especially important for those patients with NYHA class III to IV symptoms.
5.2.2 Barriers to Medication Titration
5.2.3 Clinical Assessment
Figure 4
Scope Of The Guideline
The purpose of the 2022 AHA/ACC/HFSA Guideline for the Management of Heart Failure is to provide an update and to consolidate the 2013 ACCF/AHA Guideline for the Management of Heart Failure for adults and the 2017 ACC/AHA/HFSA Focused Update of the 2013 ACCF/AHA Guideline for the Management of Heart Failure into a new document. Related ACC/AHA guidelines include recommendations relevant to HF and, in such cases, the HF guideline refers to these documents. For example, the 2019 primary prevention of cardiovascular disease guideline includes recommendations that will be useful in preventing HF, and the 2021 valvular heart disease guideline provides recommendations for mitral valve clipping in mitral regurgitation .
Read Also: Congestive Heart Failure Legs
The Aha/acc/hfsa Guidelines Are The First Full Update Since 2013 Informed By Recent Groundbreaking Clinical Trials
New heart failure guidelines released in the United States today stress a four-drug-class approach in patients with reduced ejection fraction, define a new category of mildly reduced heart failure, and celebrate new options for patients who have heart failure with preserved ejection fraction or amyloidosis, along with a number of other key updates.
The document was simultaneously published in the journals and on the websites of the three societies behind todays update: the American College of Cardiology , the American Heart Association , and the Heart Failure Society of America . The 2022 guideline is intended to provide patient-centric recommendations for clinicians to prevent, diagnose, and manage patients with heart failure, the authors state.
The last full set of HF guidelines published by these societies dates back to 2013, with a focused update released in 2017. Of note, the European Society of Cardiology released its newest heart failure guidelines last fall during the ESC Congress. There are many areas of overlap between the two documents.
But as Biykem Bozkurt, MD, PhD , writing committee vice chair for the US guidelines, pointed out to TCTMD, EMPEROR-Preserved came out just 1 hour after the release of the ESC guidelineslong past the cutoff for the writing committee to consider the data. As such, a crucial difference between the European and American recommendations is the newer advice for HFpEF patients.
Key Recommendations
A Heart Failure Top 10
American College Of Cardiology/american Heart Association/heart Failure Society Of America Recommendations For Genetic Evaluation And Testing
Genetic screening and counseling are recommended for first-degree relatives of selected individuals with genetic or inherited cardiomyopathies to detect cardiac disease and to encourage review of therapies for lowering HF progression and sudden death.
It is reasonable to refer select patients with nonischemic cardiomyopathy for genetic counseling and testing to identify conditions that could guide treatments for patients and family member.
You May Like: Can Dehydration Cause Increased Heart Rate
How To Improve Adherence
5.5.1 Medication Nonadherence
Patient adherence is fundamental to the therapeutic effectiveness of GDMT. Medication adherence is defined as the extent to which medications are taken as prescribed, such that nonadherence is not dichotomous, but rather a spectrum of types and degrees of discordance with medication prescription . Estimates of significant nonadherence in patients with HFrEF vary from 20% to 50% , with some difference by drug . Such nonadherence is associated with worse outcomes in HF . In addition to nonadherence, a large proportion of patients with HFrEF do not receive target doses of medical therapies , even in the absence of documented intolerance.
Reasons for nonadherence are complex , as outlined in . Unintentional nonadherence is thought to be more common than intentional nonadherence . As shows, the ability of patients to follow treatment plans in an optimal manner is frequently compromised by more than 1 barrier .
Table 9 Reasons for Nonadherence
| Patient |
|
Difficulty navigating patient assistance programs |
HF = heart failure.
5.5.2 General Approaches to Improving Adherence
Regularly assessing adherence helps guide individual approaches and tailor the intensity and type of adherence interventions. Notably, however, clinicians tend to overestimate actual adherence, and no perfect measure of adherence exists.
Table 10 Ten Considerations to Improve Adherence
| 1. Capitalize on opportunities when patients are most predisposed to adherence |
| Patient Criteria |
|---|
Ology And Evidence Review
The recommendations listed in this guideline are, whenever possible, evidence based. An initial extensive evidence review, which included literature derived from research involving human subjects, published in English, and indexed in MEDLINE , EMBASE, the Cochrane Collaboration, the Agency for Healthcare Research and Quality, and other selected databases relevant to this guideline, was conducted from May 2020 to December 2020. Key search words included but were not limited to the following: heart failure heart failure with reduced ejection fraction heart failure with preserved ejection fraction heart failure with mildly reduced ejection fraction systolic heart failure heart failure rehabilitation cardiac failure chronic heart failure acute decompensated heart failure cardiogenic shock beta blockers mineralocorticoid receptor antagonists ACE-inhibitors, angiotensin and neprilysin receptor antagonist sacubitril valsartan angiotensin receptor antagonist Sodium glucose co-transporter 2 or SGLT2 inhibitors cardiac amyloidosis atrial fibrillation congestive heart failure guideline-directed medical therapy HFrEF diabetes mellitus cardiomyopathy cardiac amyloidosis valvular heart disease mitral regurgitation cardiomyopathy in pregnancy reduced ejection fraction right heart pressure palliative care.
Read Also: What Are Heart Attack Symptoms In Women
Evidence Review And Evidence Review Committees
In developing recommendations, the writing committee uses evidence-based methodologies that are based on all available data . Literature searches focus on randomized controlled trials but also include registries, nonrandomized comparative and descriptive studies, case series, cohort studies, systematic reviews, and expert opinion. Only key references are cited.
An independent evidence review committee is commissioned when there are 1 questions deemed of utmost clinical importance and merit formal systematic review to determine which patients are most likely to benefit from a drug, device, or treatment strategy, and to what degree. Criteria for commissioning an evidence review committee and formal systematic review include absence of a current authoritative systematic review, feasibility of defining the benefit and risk in a time frame consistent with the writing of a guideline, relevance to a substantial number of patients, and likelihood that the findings can be translated into actionable recommendations. Evidence review committee members may include methodologists, epidemiologists, clinicians, and biostatisticians. Recommendations developed by the writing committee on the basis of the systematic review are marked SR.
Heart Rhythm Society And The European Heart Rhythm Association Select Recommendations For Genetic Testing For Channelopathies And Cardiomyopathies
Long QT syndrome
Comprehensive or LQT1-3 targeted LQTS genetic testing is recommended for the following:
- Individuals with a strong clinical index of suspicion for LQTS based on the patient’s clinical history, family history, and expressed electrocardiographic phenotype
- Asymptomatic individuals with idiopathic QT prolongation on serial 12-lead ECGs defined as QTc over 480 ms or longer than 500 ms may also be considered in asymptomatic individuals with idiopathic QT prolongation on serial 12-lead ECGs for QTc values over 460 ms or longer than 480 ms
Mutation-specific genetic testing is recommended for family members following identification of the LQTS mutation in an index case.
Catecholaminergic polymorphic ventricular tachycardia
- Comprehensive or CPVT1 and CVPT2 targeted CPVT genetic testing is recommended for any individual with a clinical index of suspicion for CPVT based on the patient’s clinical history, family history, and expressed ECG phenotype during provocative stress testing with cycle, treadmill, or catecholamine infusion.
- Mutation-specific genetic testing is recommended for family members following identification of the CPVT mutation in an index case.
Brugada syndrome
Cardiac conduction disease
Short QT syndrome
ACM / arrhythmogenic right ventricular cardiomyopathy
Left ventricular noncompaction
Restrictive cardiomyopathy
Also Check: What Is Maximum Heart Rate By Age
Evidence Gaps And Future Research Directions
Significant gaps exist despite evolving evidence and treatment strategies in patients with HF. Table 33 provides selected, common issues that should be addressed in future clinical research.
Table 33 Evidence Gaps and Future Research Directions
AF indicates atrial fibrillation ARNi, angiotensin receptor-neprilysin inhibitor ATTR, transthyretin amyloidosis BP, blood pressure CKD, chronic kidney disease COVID-19, coronavirus disease 2019 eGFR, estimated glomerular filtration rate GDMT, guideline-directed medical therapy HF, heart failure HFimpEF, heart failure with improved ejection fraction HFmrEF, heart failure with mildly reduced ejection fraction HFpEF, heart failure with preserved ejection fraction HFrEF, heart failure with reduced ejection fraction LV, left ventricular MCS, mechanical circulatory support MRA, mineralocorticoid receptor antagonist PUFA, polyunsaturated fatty acid QOL, quality of life RV, right ventricular SGLT1i, sodium-glucose cotransporter-1 inhibitors SGLT2i, sodium-glucose cotransporter-2 inhibitors TAVI, transcatheter aortic valve implantation and VHD, valvular heart disease.
Palliative And Supportive Care Shared Decision
Recommendations for Palliative and Supportive Care, Shared Decision-Making, and End-of-Life
Referenced studies that support the recommendations are summarized in the Online Data Supplements.
| COR | |
|---|---|
| C-LD | |
| 1. |
For all patients with HF, palliative and supportive careincluding high-quality communication, conveyance of prognosis, clarifying goals of care, shared decision-making, symptom management, and caregiver supportshould be provided to improve QOL and relieve suffering . |
1C-LD
| 2. |
For patients with HF being considered for, or treated with, life-extending therapies, the option for discontinuation should be anticipated and discussed through the continuum of care, including at the time of initiation, and reassessed with changing medical conditions and shifting goals of care . |
2aB-R
| 3. |
For patients with HFparticularly stage D HF patients being evaluated for advanced therapies, patients requiring inotropic support or temporary mechanical support, patients experiencing uncontrolled symptoms, major medical decisions, or multimorbidity, frailty, and cognitive impairmentspecialist palliative care consultation can be useful to improve QOL and relieve suffering . |
2aC-LD
| 4. |
For patients with HF, execution of advance care directives can be useful to improve documentation of treatment preferences, delivery of patient-centered care, and dying in preferred place . |
2aC-LD
Synopsis
You May Like: Does Heart Rate Increase During Heart Attack
