Understanding Your Heart Rate By The Numbers
If youre curious about your heart rate, you can measure it yourself. First, find your pulse by holding a finger to the radial artery on the inside of your wrist. Then, count the number of beats per minute while youre resting.
Other places your heart rate can be measured include:
- on your neck, alongside your windpipe
- inside your elbow
- on the inside of your groin/upper thigh
- on the top of your foot
When youre determining your heart rate, here are some numbers to keep in mind:
- A resting adult heart rate is normally between
Chest Pain That Isnt Caused By A Heart Attack
You feel a pain in your chest and left arm. You immediately start worrying that you’re having a heart attack. At what point do chest pains equal a heart attack? Emergency room physician Dr. Troy Madsen shares what chest pains can mean. He also discusses the symptoms and feelings of a heart attack versus “regular” chest pain.
Interviewer:
Announcer:
What Are The Harmless Causes Of Low Heart Rate
It is normal for our heart rate to fluctuate throughout the day. It naturally changes in response to what our body needs and what we are doing. Some harmless causes of bradycardia include:
-
Sleep: Our heart rate is generally lower when we are asleep or in a relaxed state. This is also known as our resting heart rate. When we are lying down and resting, our heart doesn’t have to work as hard against gravity to get the blood everywhere it needs to go. When were sleeping, our bodies dont use as much energy, so our nervous system tells the heart to take a little bit of a break.
-
Physical fitness: Cardiovascular activity strengthens our heart muscle. And a stronger heart can pump blood more efficiently. When the heart beats more efficiently in someone who has been physically training over time, their heart rate tends to be lower.
-
Certain medications: Some medications lower the heart rate in order to decrease the amount of work the heart has to do. Some examples include blood pressure medications, like beta blockers or calcium channel blockers.
While these causes of bradycardia are expected, there are some concerning conditions that can also cause a low heart rate.
Also Check: What Happens After A Massive Heart Attack
Planning A Low Potassium Diet
High potassium levels in the blood can cause serious heart troubles, especially if you are at high risk of heart failure, but before you severely restrict the potassium in your diet you may want to check in with a healthcare professional to talk about the risks of high potassium and how a low-potassium diet can help.
Cytokine Storm: A Serious Coronavirus Complication
Most serious of all, Gilotra says, is the possibility of the immune system launching an attack on the invading virus that is so severe that it destroys healthy tissues.
When responding to infection with the coronavirus, the body releases a flood of proteins called cytokines that help cells communicate with one another and fight the invaders.
In some people, perhaps due to a genetic difference, this normal defensive event is exaggerated, leaving them vulnerable to a cytokine storm. In a cytokine storm, the immune system response causes inflammation that can overwhelm the body, destroying healthy tissue and damaging organs such as the kidneys, liver and heart.
A cytokine storm and its resulting heart damage can also affect the hearts rhythm. Serious ventricular arrhythmias due to a cytokine storm can be catastrophic, Gilotra says.
A cytokine storm is difficult to survive. Current research is exploring the possible benefit of using immune-suppressing drugs to treat patients with COVID-19 who experience this serious complication.
You May Like: How Do I Know If I M Having Heart Attack
Things That Happen During A Heart Attack
Q: What happens during a heart attack?
A: In a heart attack, those arteries get blocked for one reason or another, usually involving some kind of worsening of their risk factors. For example, someone might have a night where they smoke a pack of cigarettes when they usually only smoke a few cigarettes. They might experience a heart attack because all the chemicals floating around in their blood already increased the likelihood of their existing blockages into rupturing. Heres how an existing blockage ruptures. A buildup of cholesterol, fat, and inflammatory cells accumulates underneath a thin layer of protein. When this thin layer of protein is perturbed in some way, it ruptures and all the stuff beneath it are exposed. There are these factors called clotting factors in the blood that are responsible for causing clots to happen when they see something “foreign” . They perceive those streaks of fat, deposits of cholesterol and inflammatory cells as foreign and create a clot – kind of like the clot you get when you get a papercut air is a foreign material to your blood so your blood will start to clot so you dont bleed out to death. Thats what happens inside of your coronary artery when that cap ruptures and the blood is exposed to all the stuff thats harbored inside.
Other Heart Electrical Issues
If the heart is unable to send electrical signals due to a blockage or heart disease, this can lead to bradycardia.
Complete heart block is when there is a total loss of communication between a persons atria and the ventricles. This occurs when the SA node is unable to pass a signal to the AV node.
Complete heart block results in a persons atria and ventricles activating independently of each other. If a person does not receive treatment for complete heart block quickly, it can be fatal.
Read Also: What Is A Silent Heart Attack
Describe Chest Pain To Your Doctor
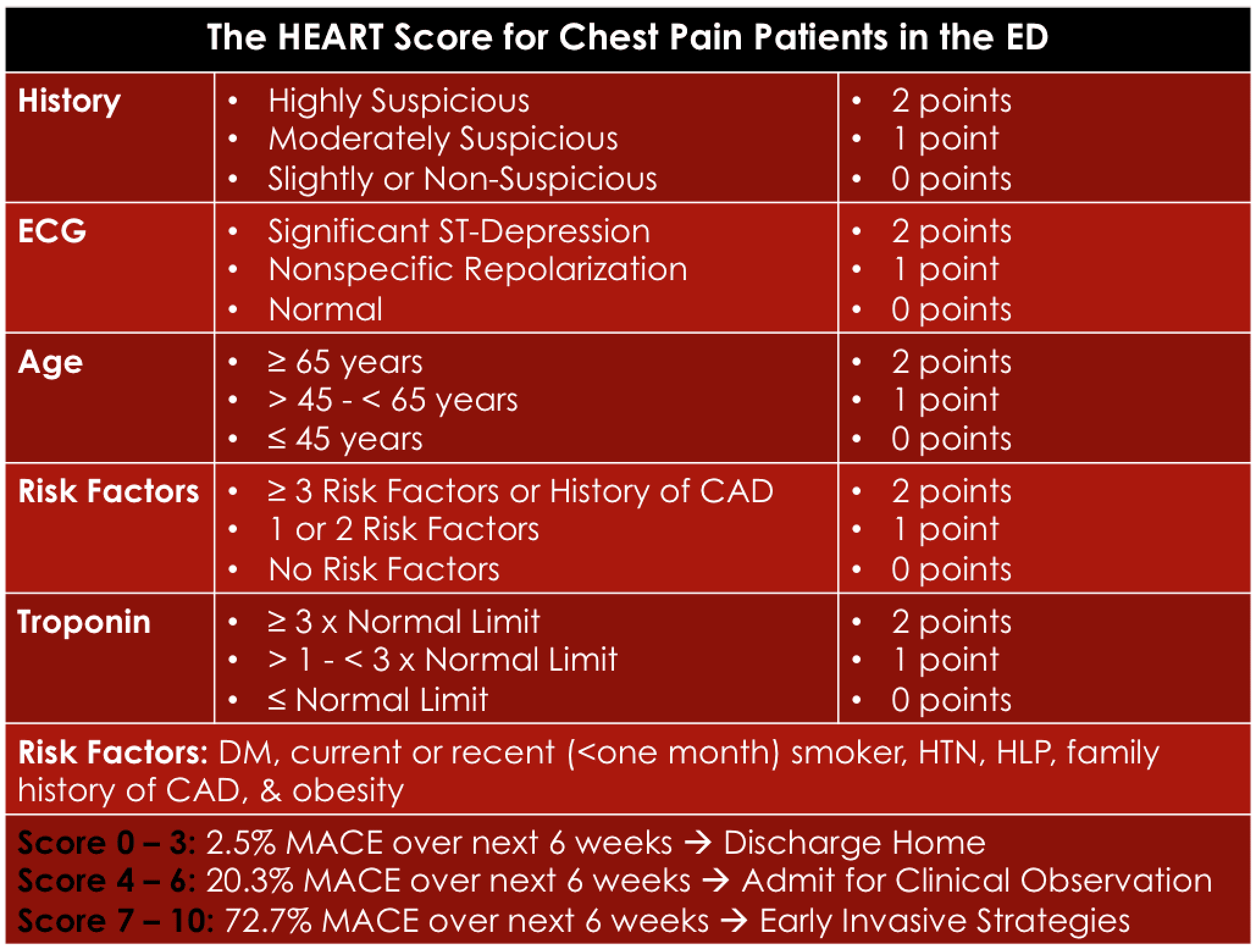
Doctors use several pieces of information to determine who is, and who isn’t, having a heart attack. In addition to the description of your symptoms and your heart risk profile, doctors use the results of an electrocardiogram and a blood test called cardiac troponin. But sometimes these don’t immediately show abnormalities. So, what you describe to the doctor and your medical history are extremely important in determining the initial steps in your treatment.
Here are some things your doctors will want to know about what you are experiencing:
-
What is it that you are feeling ?
-
Where is the discomfort?
-
Has it gotten worse or stayed the same?
-
Is the feeling constant, or does it come and go?
-
Have you felt it before?
-
What were you doing before these feelings started?
Clear answers to these questions go a long way toward nailing down a diagnosis. A few seconds of recurrent stabbing pain is less likely to be a heart attack , while pain centered in the chest that spreads out to the left arm or jaw is more likely to be one.
What Causes A Low Heart Rate
Many things can bring on a slow heart rate.
A heart malfunction
The most common cause for bradycardia is a malfunction in the hearts natural pacemaker, the sinus node. It controls how quickly the top and bottom heart chambers pump blood through the body.
AV Block
Another cause of bradycardia is atrioventricular block , in which the top and bottom chambers dont communicate well and your heart rate drops as a result.
Its like having virtual electrical cables and wires inside the heart, Dr. Baez-Escudero says. These deteriorate as we age. Common medications used in older populations can also often make bradycardia more significant.
Age
Age is the most common risk factor for developing bradycardia. The condition is most common among men and women over age 65.
Having certain illnesses or conditions
Illness or other conditions may also cause bradycardia. These include:
- Heart attacks due to coronary artery disease.
- A bacterial infection in the blood that attacks your heart.
- Inflammation of your heart muscle.
- Low thyroid function.
- Too much potassium in your blood.
- Certain medications, including beta blockers and antiarrhythmics.
Congenital heart defects, diabetes or long-standing high blood pressure all may make bradycardia more likely, says Dr. Baez-Escudero.
Don’t Miss: Why Does My Resting Heart Rate Fluctuate
Does Sleep Deprivation Affect Heart Health
Substantial evidence demonstrates that sleeping problems, including sleep deprivation and fragmented sleep, have negative effects on heart health.
Sleep is an essential time for the body to recuperate. During the non-rapid eye movement sleep stages, heart rate slows, blood pressure drops, and breathing stabilizes. These changes reduce stress on the heart, allowing it to recover from strain that occurs during waking hours.
Without sufficient nightly sleep, a person doesnt spend enough time in the deep stages of NREM sleep that benefit the heart. The same problem can affect people whose sleep is frequently interrupted.
As a result, chronic sleep deprivation has been linked to numerous heart problems including high blood pressure, high cholesterol, heart attack, obesity, diabetes, and stroke.
How Is Bradycardia Treated
The treatment of bradycardia depends on whats causing it. Bradycardia thats mild or occasional may not require treatment.
If a slow heart rate is due to the effect of a medication, its possible that your doctor may adjust your medication dosage. If possible, they could also switch you to a different medication that doesnt have bradycardia as a side effect.
Similarly, if an underlying condition is contributing to your bradycardia, your doctor will work to address that condition. For example, the medication levothyroxine can be used to manage hypothyroidism.
Its also possible that your doctor may recommend a pacemaker. This is an implanted medical device that stimulates heartbeats so that they occur at a regular rate and rhythm. Bradycardia is one of the main conditions for which a pacemaker may be recommended.
Also Check: Is Green Tea Good For Heart Attack Patients
How To Survive This Pandemic
If you experience any of these symptoms, seek medical help. And do everything you can to prevent gettingand spreadingCOVID-19 in the first place: Wear a face mask, get tested if you think you have coronavirus, avoid crowds , practice social distancing, only run essential errands, wash your hands regularly, disinfect frequently touched surfaces, and to get through this pandemic at your healthiest, don’t miss these 35 Places You’re Most Likely to Catch COVID.
Sleep For People With Heart Disease
Because sleep deprivation can harm the heart, its important for people with cardiovascular problems to make getting good sleep a priority. Some evidence even indicates that improving sleep may reduce the likelihood of heart attacks or other cardiovascular problems in people who are otherwise at high risk.
Unfortunately, some heart problems can interfere with sleep. For example, diabetes can cause frequent nighttime urination, and other cardiovascular disorders may create chest discomfort when trying to get to sleep. Worry and anxiety about heart health can also make it hard to wind down and fall asleep normally.
Because numerous factors can influence both sleep and cardiovascular health, its most helpful to talk with your doctor about heart-healthy sleep. A doctor can help develop a specific plan to improve your sleep while also addressing other lifestyle factors, such as diet and exercise, that are important for your heart and overall wellness.
Read Also: What Is A Normal Resting Heart Rate For A 50 Year Old Woman
Palpitations Of The Heart
Palpitations are a sensation or awareness of your heart beating. They may feel like your heart is racing, thumping or skipping beats. Almost everyone has had palpitations at some time in their life. They are usually associated with an abnormal heart rhythm .
Palpitations may have no obvious cause, but can be triggered by:
- physical activity
- nicotine
- illicit substances.
An occasional palpitation that does not affect your general health is not usually something to worry about. However, see your doctor if you have more frequent or consistent palpitations, which may be associated with a serious arrhythmia.
What Tests Will Be Done To Diagnose This Condition
The most likely tests for bradycardia include:
- Physical examination. A physical examination involves a healthcare provider looking at your body for any visible signs of conditions or problems. They may also feel any affected areas, as some problems cause changes that you can feel but not see.
- Electrocardiogram . This test is essential for diagnosing bradycardia because it can track your hearts electrical activity very precisely. This test uses several sensors called electrodes that stick to the skin of your chest. The electrodes can detect the electrical activity in your heart and show it as a wave on either a paper printout or a computer screen.
Lab tests are also possible for bradycardia, most of which can help rule out other problems. These tests include:
- Electrolyte levels: These tests measure the levels of electrolytes in your blood, especially calcium, potassium and magnesium.
- Thyroid hormone levels: Hypothyroidism can cause bradycardia.
- Troponin: Your heart muscles cells contain a specific type of troponin, a protein. Damage to those cells causes troponin to leak into your blood, which can indicate damage to your heart. Troponin is a key indicator that providers use to diagnose heart attacks.
- Toxicology screen. This test looks for toxic substances in your blood. This test can identify drugs that can cause bradycardia, as well as other heart-damaging substances.
Also Check: Can Ibs Cause Heart Palpitations
Is It Any Of The Above Is It At Least Two
Q: How many of the factors above can a patient have and still be considered “safe”?
A: I think if you have any of the above and you have chest pain, then its concerning and with each additional factor that you also have, that increases your pre-test probabilityI am sure there’s literature out there about how much, maybe one of the Framingham heart studies would categorize people better. I dont know the exact number off the top of my head but that would be a place to look because they identified risk factors for coronary risk factors in general. They did a good job at explaining and quantifying how much each additional risk factor adds to people.
Understanding A Slow Heart Rate
It’s common to experience a slow heart rate as you get older, but it’s also something that your doctor needs to monitor. Find out what a slow heart rate means for your health, and when it’s time to seek treatment.
Its common for everyones heart beat rate to slow down at rest, but some people have a chronically slow heart rate that causes symptoms such as fatigue and lightheadedness.
This condition is called bradycardia, and its more common as you age. Mild cases of bradycardia dont have symptoms, but in severe cases it can cause chest pain, shortness of breath, and may even lead to cardiac arrest.
Are you doing everything you can to manage your heart condition? Find out with our interactive checkup.
A normal heart beat rate is between 60 and 100 beats a minute, says Joshua D. Moss, MD, a cardiologist at the Heart Rhythm Center at the University of Chicago Medical Center. Bradycardia is defined as having a heart rate of less than 60 beats a minute. In reality, you can have periods when your heart beat rate goes below 60 and not have bradycardia, Dr. Moss says. It can happen when youre sleeping, or it can occur in highly conditioned athletes when theyre at rest.
How Bradycardia Is Detected
You may be prompted to find out if you have a slow heart rate if you have certain symptoms. However, some people with the condition dont have any symptoms.
What Causes Bradycardia
How Bradycardia Is Treated
Read Also: Does Acid Reflux Cause Heart Palpitations
Arrhythmias As Symptoms Of Serious Disorders
Arrhythmia can be a symptom of more serious underlying disorders, including:
- cardiovascular disease
- heart valve or heart muscle abnormalities
- congenital heart disease
- an overactive thyroid gland
- problems with the electrical circuitry of the heart, such as blocked signals or signals taking an abnormal path through the heart
- significant electrolyte abnormalities
- irritable heart cells sending extra electrical signals.
What To Expect At Your Office Visit
Your provider will examine you and ask questions about your medical history and symptoms.
You may be asked:
- Do you feel skipped or stopped beats?
- Does your heart rate feel slow or fast when you have the palpitations?
- Do you feel a racing, pounding, or fluttering?
- Is there a regular or irregular pattern to the unusual heartbeat sensations?
- Did the palpitations begin or end suddenly?
- When do the palpitations occur? In response to reminders of a traumatic event? When you are lying down and resting? When you change your body position? When you feel emotional?
- Do you have any other symptoms?
An electrocardiogram may be done.
If you go to an emergency room, you will be connected to a heart monitor. However, most people with palpitations do not need to go to an emergency room for treatment.
If your provider finds you have an abnormal heart rhythm, other tests may be done. This may include:
- Holter monitor for 24 hours, or another heart monitor for 2 weeks or longer
Read Also: Elevated Heart Rate When Sick
Risk Factors For Bradycardia
Risk factors that could contribute to bradycardia include:
- Age: Men and women age 65 and older are most likely to develop a slow heart rate that needs treatment.
- Congenital heart defect: Problems with the structure or function of the heart present at birth can cause a slow heart rate.
- Electrolyte imbalance:Any abnormality in the bodys mineral balance including calcium, chloride, magnesium, phosphate, potassium and sodium can lead to a slow or irregular heart rate.
- Infection of the heart: Certain bacteria, viruses and parasites can infect the heart muscle, causing inflammation and damage leading to an irregular heart rate.
- Previous heart attacks: Heart attacks can weaken the heart muscle or cause problems with its electrical system.
- Low thyroid: An abnormally low level of thyroid hormones can cause a slow heart rate.
- Medications for other heart problems: Some medications for treating high blood pressure or other heart conditions like beta blockers, antiarrhythmics and digoxin can cause bradycardia.
