Conflict Of Interest Statement
Financial arrangements of the authors with companies whose products may be related to the present report are listed below, as declared by the authors: Kris Vijay has served as a consultant, speaker, and/or advisor for Amarin Corporation, Amgen, AstraZeneca, Aventyn, Baxter International, Boehringer Ingelheim/Eli Lilly and Company, Esperion Therapeutics, Legacy Heart Care, Novo Nordisk, and Pfizer. He is a board member of the Cardiorenal Society of America, Life 365, and the National Lipid Association. Brendon L. Neuen has received fees for advisory boards, steering committee roles, scientific presentations, and travel from AstraZeneca, Bayer AG, and Janssen Pharmaceuticals, with all honoraria paid to his employer. Edgar Lerma has no conflicts to declare.
Recommended Reading: Is Congestive Heart Failure Hereditary
What Is The Outlook With Heart Failure
With the right care, congestive heart failure wont stop you from doing the things you enjoy. Your prognosis, or outlook for the future, will depend on:
- How well your heart muscle is working.
- How well you respond to your treatment plan.
- How well you follow your treatment plan.
One study says that people with heart failure have a life span 10 years shorter than those who dont have heart failure. Another study showed that the survival rates of people with chronic heart failure were 80% to 90% for one year, but that dropped to 50% to 60% for year five and down to 30% for 10 years.
A different study found that people who had heart failure and were discharged from the hospital had expected life spans ranging from three to 20 years, depending on various factors like age and gender. Its important to look at your specific situation when considering your prognosis.
Heart Failure With Preserved Ejection Fraction In Patients With Ckd
The diagnosis of HFpEF in patients with CKD may be challenging. The BNP levels may be elevated because of the CKD and may not be diagnostic. The fluid overload may be a result of CKD itself. These patients have similar risk of poor outcomes and suffer frequent hospital admissions because of fluid overload, similar to patients with heart failure with reduced ejection function . Careful use of diuretics is necessary to control the symptoms of volume overload. Nonsteroidal anti-inflammatory drugs should be avoided because they can cause AKI and fluid retention in patients with CKD, and mimic HFpEF. There is no compelling evidence for effective therapy in HFpEF to improve outcomes such as cardiovascular mortality or heart failure hospitalizations. However, large trials are underway, such as FINEARTS-HF , a randomized controlled trial of finerenone in patients with CKD and HFpEF.
Don’t Miss: Can Aspirin Lower Heart Rate
Management Of Hf In Patients With Ckd
The co-existence of CKD and HF has major clinical implications as baseline renal function is a strong determinant of outcome in patients with HF. Moreover, renal function is an important factor in the management of HF as it alters the pharmacokinetics and pharmacodynamics of several cardiovascular medications, necessitating drug dose adjustments. Conversely, certain cardiovascular medications can interfere with renal function and, hence, must be administered with caution in patients with underlying CKD.
Because patients with CKD have been relatively underrepresented in HF clinical trials, evidence based management of patients with concomitant CKD and HF is limited. Therefore, treatment strategies in such patients, including those described in this review, are based mainly on results of observational data from unselected cohorts, or from post-hoc analysis of clinical trials in which patient sub-groups with renal dysfunction were included.
Also Check: What Is Considered A Low Heart Rate
Discussion Of Aki In This Patient
This patient developed AKI while undergoing diuresis. As alluded to earlier and discussed in more detail later, AKI in the setting of decongestion has been associated with improved prognosis in some studies . The exact pathophysiologic cause of AKI in our patient cannot be determined, but possibilities include decreased forward perfusion and diuretic-induced neurohormonal activation. The worsening of kidney function despite diuresis and paracenteses suggests that increased venous pressure was not the primary cause.
We have been traditionally taught that prerenal azotemia is associated with low FeNa and bland urine sediment, while intrinsic renal disease due to acute tubular necrosis is associated with high FeNa and granular casts. These distinctions, however, are likely neither very sensitive nor specific, and there may be overlap, particularly when there is tubular damage with low FeNa. This suggests the ability of nondamaged parts of the nephron to conserve sodium. Overlap may also occur during diuretic therapy, when the FeNa may be high in the setting of prerenal pathophysiology. In the latter setting, the FeUrea may be more accurate in distinguishing ATN from prerenal azotemia . Given the bland urine sediment and the clinical presentation, the cause of AKI was consistent with CRS, although one cannot rule out some component of ATN because the FeUrea was equivocalit was above the threshold of 35% used to define prerenal azotemia.
You May Like: How To Measure Heart Rate Variability
What Does Moving To Hospice Care Involve
If you and your family have made the decision to pursue hospice care while receiving inpatient care, a case manager or social worker can help facilitate the process. If you are at home and would like to transition to hospice care, hospice agencies can help make the arrangements. Hospice agencies will review your needs and have a doctor order the appropriate medications for you. These medications will focus not on treating your condition, but on managing your symptoms and comfort as much as possible.
Heart Disease And Chronic Kidney Disease
Having chronic kidney disease means you are more likely to get heart disease. CKD can cause heart disease, and heart disease can cause CKD. In fact, heart disease is the most common cause of death among people on dialysis.
The best way to prevent heart disease is to prevent or treat the problems that can cause it, such as diabetes, high blood pressure and anemia.
Recommended Reading: Symptoms.of Heart Attack Woman
Echocardiographic Findings In Relation To Cause Of Chronic Kidney Disease
To explore any differences between different causes of ESKD, we compared patients with an aetiology of hypertension, diabetes, glomerulonephritis and polycystic kidney disease . Left atrial volume was significantly larger in patients with hypertensive nephropathy compared to the other groups. We found no difference in the number of patients with LVEF< 50%, LVEF40%, or valve disease between groups.
Table 3 Echocardiographic findings by cause of kidney disease
Hospice And Congestive Heart Failure
When a heart failure patient has been diagnosed with six months or less to live, the added support of hospice care helps them remain in their home until end of life.
Crossroads Hospice & Palliative Care provides a team of nurses, aides, social workers, volunteers, and chaplains to support the patient and their family through the final stages of congestive heart failure symptoms. To learn more about referring your patient to hospice, please call Crossroads at 1-888-564-3405.
Also Check: What Should My Heart Rate Be For Cardio
Stage C Treatment Options
Treatment at this stage focuses on managing your symptoms, optimizing your heart function, and preventing worsening of your condition.
Medications to treat stage C heart failure include:
- Diuretics to reduce fluid retention
- Beta blockers to help make your heart work less hard
- SGLT2 inhibitors to reduce the risk of cardiovascular death and hospitalization for heart failure
- Angiotensin-converting enzyme inhibitors
- Angiotensin II receptor blockers
- Entresto , which reduces the risk of death and hospitalization among patients with chronic heart failure
- Aldosterone antagonists
- Digoxin to help the heart beat stronger and more regularly
- Possible cardiac resynchronization therapy
- Possible implantable cardiac defibrillator therapy
In addition to the lifestyle changes for stages A and B, you may need to make the following changes:
- Reduce your sodium intake
- Restrict fluid intake
- Keep track of your weight daily
Remember that even if the treatment causes your symptoms to get better or stop, you still need to continue treatment to slow the progression of your condition to stage D.
Moderate Stage Of Chf
At Stage C, as the heart continues to fail, the person develops weakness and significant fatigue, shortness of breath or palpitations with the slightest physical exertion. She begins to limit activity because of these symptoms as she is only comfortable when resting. A doctor’s evaluation and testing shows moderate signs of heart dysfunction,
Other possible symptoms might include more visible edema of the lower extremities and the hands might also swell as the fluid congestion in body tissues increases. Shoes and rings might be tighter. The pulse might become weaker because of the struggling heart.
Recommended Reading: Which Of These Will Increase The Heart Rate
Epidemiology Of Chronic Heart Failure And Chronic Kidney Disease
Chronic heart failure affects approximately 12% of the adult population in developed countries, with increasing prevalence in patients over the age of 70 years. It includes both those with preserved and those with reduced ejection fraction, but here we will only consider the management of the latter.
Renal dysfunction is common in patients with CHF. One study found that 33% of CHF patients with New York Heart Association class III and IV symptoms had severely impaired renal function .
Baseline renal function is just as important a prognostic marker as ejection fraction or NYHA class. For each 1 ml/min decrease in creatinine clearance there is a 1% increase in mortality. This is important as some CHF interventions reduce creatinine clearance by > 10 ml/min.
Aki In Patients With Heart Failure And Ckd
The incidence of AKI is high in patients with heart failure. Incidence of AKI among acute heart failure admissions at St Georges Hospital was 17% in 1094 patients admitted with acute decompensated heart failure, and inpatient mortality was 21% with stage 1, 36% with stage 2, and 48% with stage 3 AKI . In a meta-analysis of 28 trials with 49,890 patients, the incidence of AKI or worsening of kidney function was 23%, and the mortality was higher over 488±569 days . In a unique situation in cardiology, when the kidney insult is known and preventive measures are used , the incidence was 7.1% in 985,737 US patients undergoing percutaneous coronary interventions, and was higher with the presence of CKD and heart failure . The other causes of AKI in patients with heart failure are infection, sepsis, volume depletion, drug toxicity, and obstruction of the urinary tract in older men with enlarged prostate.
Read Also: How Much Does Heart Surgery Cost
What Is The Life Expectancy For An Elderly Person With Congestive Heart Failure
Although there have been recent improvements in congestive heart failure treatment, researchers say the prognosis for people with the disease is still bleak, with about 50% having an average life expectancy of less than five years. For those with advanced forms of heart failure, nearly 90% die within one year.
Angiotensin Receptor And Neprilysin Inhibitor Therapy In Patients With Heart Failure With Reduced Ejection Fraction And Ckd
A large randomized controlled trial of dual angiotensin receptor and neprilysin inhibitor therapy excluded patients with eGFR< 30 ml/min per 1.73 m2 , but included patients with only mild CKD . A randomized controlled trial of angiotensin receptor neprilysin inhibitors, including patients with eGFR as low as 20 ml/min per 1.73 m2, demonstrated safety and efficacy similar to irbesartan . More recently, angiotensin receptor and neprilysin inhibitor therapy has been shown to slow the progression of CKD in patients with heart failure with preserved ejection fraction more effectively than valsartan . The recommended starting dosage for patients with eGFR< 60 ml/min per 1.73 m2 is 24 mg sacubitril and 26 mg valsartan, administered twice per day, at least 36 hours after stopping ACEis or ARBs the dose is then increased, with careful monitoring of creatinine, potassium, and BP.
Recommended Reading: Exacerbation Of Congestive Heart Failure
Request A Hospice Evaluation
The primary physician may recommend hospice when the time is right. But as anyone who has faced a serious illness knows, patients and family members often must act as their own advocates to receive the care they need and deserve.
You, your loved one or your trusted physician may request an evaluation to see if hospice is an appropriate option for care.
What Are The Overall Benefits Of Hospice Care
If you or a loved one is facing a life-limiting illness, such as congestive heart failure, hospice can provide specialized medical care for patients and support services for loved ones. Here are some other lesser-known benefits of hospice.
2Miller SC, Gozalo P, Mor V. Hospice enrollment and hospitalization of dying nursing home patients. American Journal of Medicine 2001 111:38-44
Recommended Reading: Resting Heart Rate Chart By Age
Days Before Death Symptoms
In the days before death, a series of physiological changes will occur. Their pulmonary system will start to degrade and the will become congested, leading to a tell-tale death rattle. Their breathing will also exhibit fluctuations, as they may begin to respirate up to 50 times per minute or as little as six. When exhaling, they may puff their lips. They may also begin to cough more frequently, but in general, the congestion itself is painless.
During their last days, your loved one may begin to experience hallucinations in which they talk to people who arent there or who have also died. It is important to maintain a close eye on your loved one if they begin exhibiting these symptoms. There is no guarantee for how long they may have left, and some people pass through this process faster than others.
Some common symptoms those a few days from death experience include:
- A drop in blood pressure
- The body temperature changes frequently
- Skin changing color or becoming blotchy
- Erratic sleeping patterns
How Is Heart Failure Treated
Your treatment will depend on the type of heart failure you have and, in part, what caused it. Medications and lifestyle behaviors are part of every treatment plan. Your healthcare provider will talk to you about the best treatment plan for you. Treatment is the same, regardless of gender.
As heart failure gets worse, your heart muscle pumps less blood to your organs, and you move toward the next stage of heart failure. Since you cant move backward through the heart failure stages, the goal of treatment is to keep you from moving forward through the stages or to slow down the progression of your heart failure.
Stage A treatment
The usual treatment plan for people with Stage A heart failure includes:
- Regular exercise, being active, walking every day.
- Stopping the use of tobacco products.
- Treatment for high blood pressure .
- Treatment for high cholesterol.
- Not drinking alcohol or using recreational drugs.
- Angiotensin-converting enzyme inhibitor or an angiotensin II receptor blocker if you have coronary artery disease, diabetes, high blood pressure, or other vascular or cardiac conditions.
- Beta-blocker if you have high blood pressure.
Stage B treatment
The usual treatment plan for people with Stage B heart failure includes:
Stage C treatment
The usual treatment plan for people with Stage C HF-rEF includes:
If the treatment causes your symptoms to get better or stop, you still need to continue treatment to slow the progression to Stage D.
Stage D treatment
Don’t Miss: Does Covid Cause Heart Attacks
What Causes Congestive Heart Failure
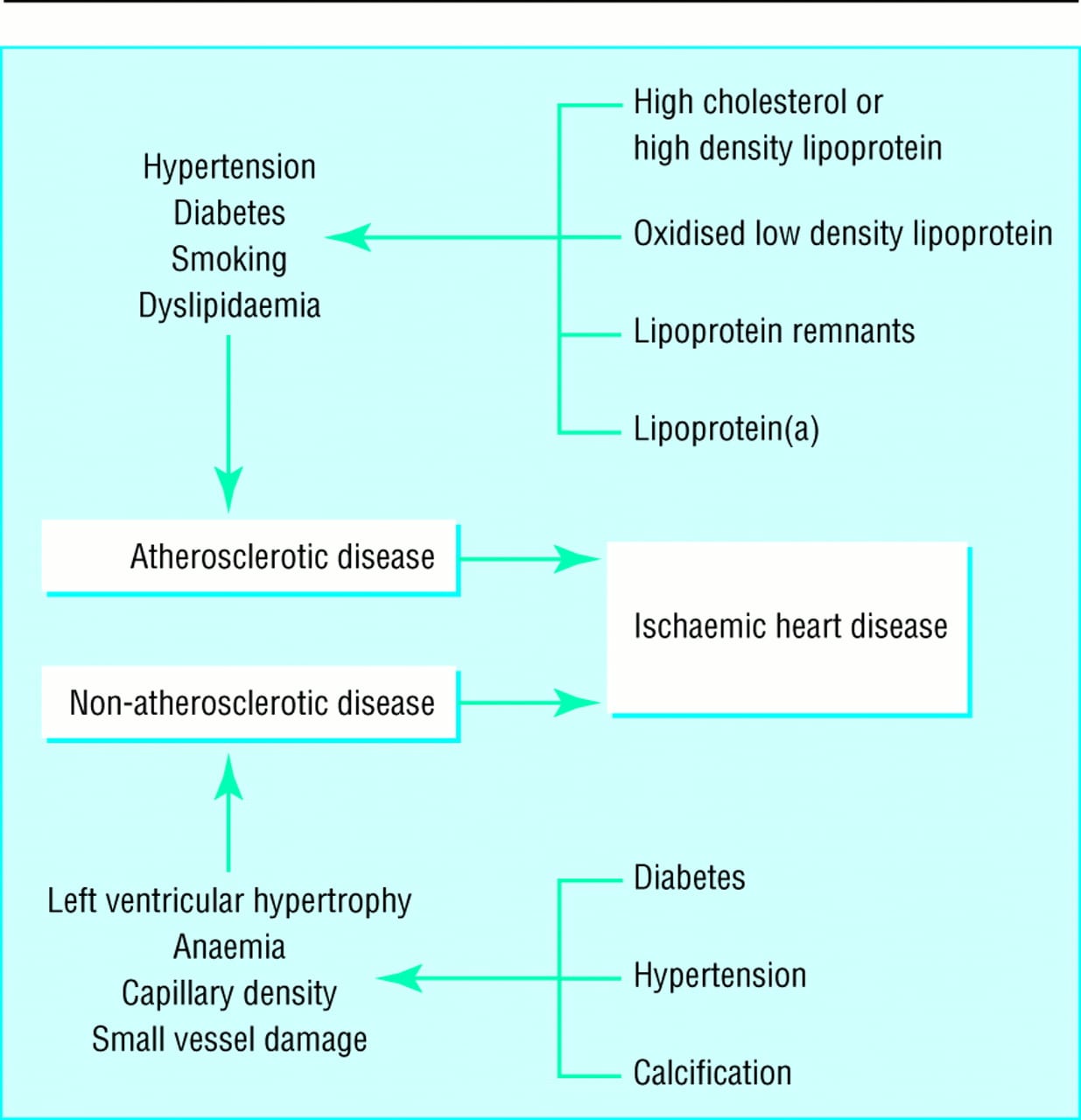
There are several conditions that can impair the pumping efficiency of the heart. Below are a few common and rare conditions that can cause congestive heart failure:
- Coronary artery disease : This is the most common cause of congestive heart failure, as the arteries become blocked or severely narrowed, which decreases blood flow to the heart.
Read Also: Can Sinus Infection Cause Increased Heart Rate
The Depth Of The Problem
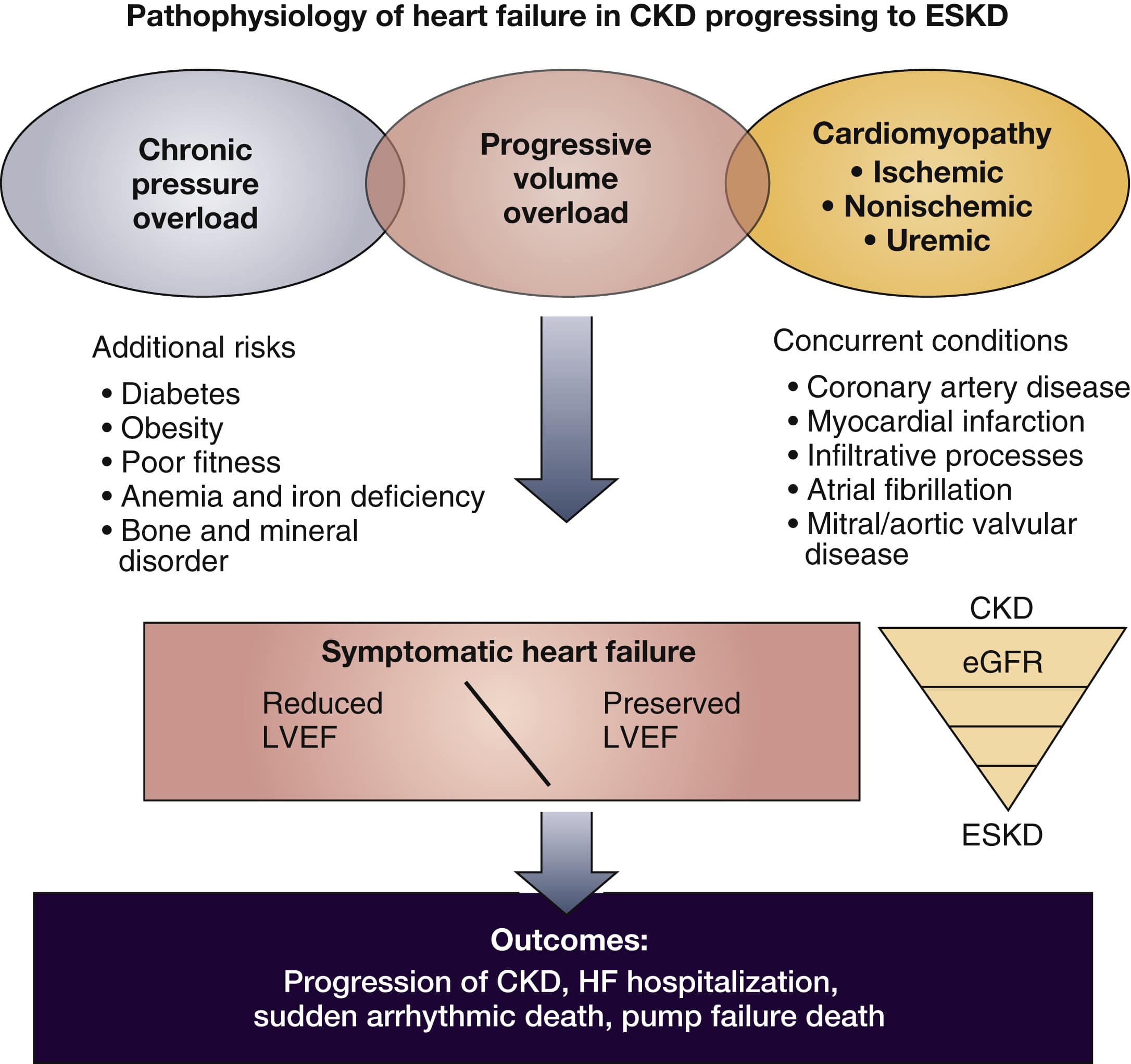
The cardiovascular system maintains a direct communication with other organ systems however, the cardiorenal interaction appears to be the most substantial. This is supported by the position statement from the National Kidney Foundation Task Force on cardiovascular outcomes in CKD: patients with CKD be considered in the highest risk group for subsequent cardiovascular events and that treatment recommendations based on cardiovascular risk stratification should take into account the highest-risk status of these patients .
Also Check: Living With Heart Failure
End Stages Of Heart Failure: What To Expect
Congestive heart failure is one of the most common reasons for hospital admissions for senior citizens. In fact, over 5 million adults in the United States experience heart failure.
Heart failure occurs when the heart muscle becomes damaged and can no longer pump blood effectively. Although symptoms can be managed, this is a chronic condition with no cure. In time, patients will reach the final stages of congestive heart failure.
Patients in the end stages of heart failure want to know what to expect. The symptoms of end-stage congestive heart failure include dyspnea, chronic cough or wheezing, edema, nausea or lack of appetite, a high heart rate, and confusion or impaired thinking.
Heart Failure Therapy In Patients With Ckd
Management of chronic heart failure in the general population has changed over the past 3 decades. Novel agents such as ivabradine, angiotensin receptor neprilysin inhibitors, mineralocorticoid receptor inhibitors, and cardiac resynchronization therapy have improved survival. Many trials have included patients with mild-to-moderate CKD, and evidence has emerged for newer agents in the treatment of patients with heart failure and CKD, which is discussed below, and summarized in and .
Heart failure studies in general population with clinical characteristics including creatinine- or eGFR-based inclusion criterion
Don’t Miss: Can Statins Cause Heart Palpitations
What Is Chronic Kidney Disease
Chronic kidney disease is the disease in which the gradual loss of kidney functions found to get occur. Our kidneys play very important jobs in the body and protect the other organs from damage. It helps in the excretion of waste and toxins from the body which can be much dangerous for our overall health. At the time of kidney disease, all the functions performed by the kidneys found to get affected and cause the waste build up inside the body. Here are the causes of chronic kidney disease, every individual need to be aware of:
- Diabetes and frequent hypertension
- Urine backs up inside the kidneys
- Kidney infection
