Definition Of Heart Failure
Heart failure is not a single pathological diagnosis, but a clinical syndrome consisting of cardinal symptoms that may be accompanied by signs . It is due to a structural and/or functional abnormality of the heart that results in elevated intracardiac pressures and/or inadequate cardiac output at rest and/or during exercise.
Identification of the aetiology of the underlying cardiac dysfunction is mandatory in the diagnosis of HF as the specific pathology can determine subsequent treatment. Most commonly, HF is due to myocardial dysfunction: either systolic, diastolic, or both. However, pathology of the valves, pericardium, and endocardium, and abnormalities of heart rhythm and conduction can also cause or contribute to HF.
Clinical Characteristics Of Patients With Heart Failure With Mildly Reduced Ejection Fraction
There is a substantial overlap of clinical characteristics, risk factors, patterns of cardiac remodelling, and outcomes among the LVEF categories in HF. Patients with HFmrEF have, on average, features that are more similar to HFrEF than HFpEF, in that they are more commonly men, younger, and are more likely to have CAD ,,, and less likely to have AF and non-cardiac comorbidities . However, ambulatory patients with HFmrEF have a lower mortality than those with HFrEF, more akin to those with HFpEF.
Patients with HFmrEF may include patients whose LVEF has improved from 40% or declined from 50%.
Evidence Review And Evidence Review Committees
In developing recommendations, the writing committee uses evidence-based methodologies that are based on all available data . Literature searches focus on randomized controlled trials but also include registries, nonrandomized comparative and descriptive studies, case series, cohort studies, systematic reviews, and expert opinion. Only key references are cited.
An independent evidence review committee is commissioned when there are 1 questions deemed of utmost clinical importance and merit formal systematic review to determine which patients are most likely to benefit from a drug, device, or treatment strategy, and to what degree. Criteria for commissioning an evidence review committee and formal systematic review include absence of a current authoritative systematic review, feasibility of defining the benefit and risk in a time frame consistent with the writing of a guideline, relevance to a substantial number of patients, and likelihood that the findings can be translated into actionable recommendations. Evidence review committee members may include methodologists, epidemiologists, clinicians, and biostatisticians. Recommendations developed by the writing committee on the basis of the systematic review are marked SR.
You May Like: What Is Maximum Heart Rate
Diagnostic Algorithm For Classification Of Hf According To Lvef
Structural and functional alterations of the heart as the underlying cause for the clinical presentation support the diagnosis of HFmrEF and HFpEF . The criteria for diagnosis of HFmrEF and HFpEF require evidence of increased LV filling pressures at rest, exercise, or other provocations. The criteria can be fulfilled with findings of elevated levels of natriuretic peptides, echocardiographic diastolic parameters such as an E/e 15 or other evidence of elevated filling pressures, or invasive hemodynamic measurement at rest or exercise. Evidence of structural heart disease may be used to further support the diagnosis of HFpEF. Key structural alterations are an increase in left atrial size and volume and/or an increase in LV mass .
Figure 4
Diagnostic Algorithm for HF and EF-Based Classification
The algorithm for a diagnosis of HF and EF-based classification is shown. BNP indicates B-type natriuretic peptide ECG, electrocardiogram EF, ejection fraction HF, heart failure HFmrEF, heart failure with mildly reduced ejection fraction HFpEF, heart failure with preserved ejection fraction HFrEF, heart failure with reduced ejection fraction LVEF, left ventricular ejection fraction LV, left ventricular and NT-proBNP, N-terminal pro-B type natriuretic peptide.
Pharmacologic Therapies For Hfref
The sequential initiation of medication with prognostic benefit has historically underpinned the treatment for patients with a diagnosis of HF with reduced ejection fraction . Such medications are typically considered before other therapies, including devices, with the goal of reducing the risk of death, hospitalisation for HF and improving symptoms. Until recently, there were three main groupings of drugs used:
These drugs antagonise maladaptive neurohumoral activation, thought to be central to the pathophysiology of HF. As such, they are considered disease-modifying drugs. Large-scale trials over the last 30+ years have confirmed efficacy at reducing mortality and HF hospitalisations, often accompanied by improving symptoms .316 There is a fundamental need to appreciate this, since in clinical practice it is common to see these drugs stopped or down-titrated due to the misconception that their primary use is to lower blood pressure or for diuretic effect. Such misunderstanding can lead to the inappropriate cessation of life prolonging therapy.
Table 1. Randomised trials studying the group of patients with a left ventricular ejection fraction 40% . The table shows A: trials with earlier disease-modifying drugs and B: those with more recent drug classes incorporated into the 2021 ESC guidelines
Read Also: Signs For Heart Attack In Woman
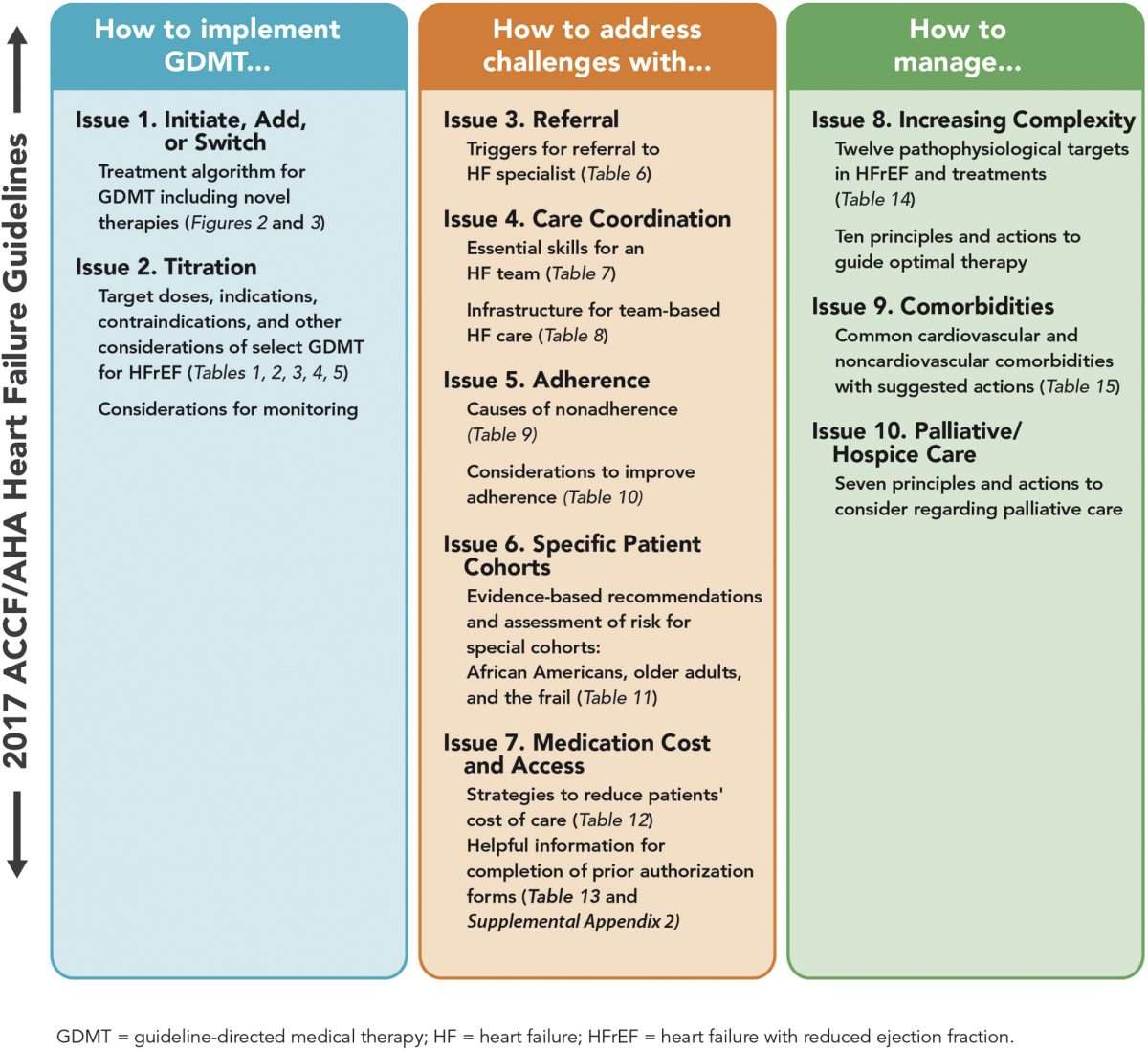
How To Achieve Optimal Therapy Given Multiple Drugs For Hf Including Augmented Clinical Assessment That May Trigger Additional Changes In Gdmt
5.2.1 Target Doses
To achieve the maximal benefits of GDMT in patients with chronic HFrEF, therapies must be initiated and titrated to maximally tolerated doses . Doses of GDMT higher than those studied in randomized clinical trials, even if tolerated, are not known to provide incremental benefits, and are generally not recommended.
Strategies for titration are detailed in and . Achieving target or maximally tolerated doses of GDMT is the goal of titration. Beta-blocker doses should be adjusted every 2 weeks in a patient with no evidence of decompensated HF and no contraindications to higher doses. Longer time periods may be needed for frail patients or those with marginal hemodynamics, whereas more rapid titration may be reasonable in clinically stable patients without hypotension. Following adjustment, patients should be cautioned that there may be a transient worsening of HF symptoms such as dyspnea, fatigue, erectile dysfunction, or dizziness.
For several reasons, HYD/ISDN-indicated therapy for HF is often neglected in eligible patients. However, given the benefits of this combination and the favorable impact on health status , African-American patients should receive these drugs once target or maximally tolerated doses of beta-blocker, ARNI/ACEI/ARB, and aldosterone antagonists are achieved . This combination of drugs is especially important for those patients with NYHA class III to IV symptoms.
5.2.2 Barriers to Medication Titration
5.2.3 Clinical Assessment
Heart Failure Guidelines Are Updated By Esc
The European Society of Cardiology and the Heart Failure Association have updated their guidelines for the diagnosis and treatment of acute and chronic heart failure.
The guidelines are an update to the ESCs 2016 recommendations and now include distinct recommendations for each phenotype of heart failure.
Among the new recommendations are:
- Treatment with a focus on mortality and morbidity for heart failure with mildly reduced ejection fraction
- New classification for acute heart failure, including 4 major clinical presentations
- New medication regimens and treatments for diabetes, obesity, and other noncardiovascular comorbidities
- New considerations such as genetic testing and treatments for cardiomyopathies
- New key quality indicators to measure the use of these guidelines by health care professionals
The aim of this ESC Guideline is to help health professionals manage people with heart failure according to the best available evidence, the authors concluded. Fortunately, we now have a wealth of clinical trials to help us select the best management to improve the outcomes for people with HF for many, it is now both preventable and treatable. This guideline provides practical, evidence-based recommendations.
You May Like: Who Invented Open Heart Surgery
Esc Guidelines For Acute And Chronic Heart Failure: Key Points
Aug 29, 2021 | Supriya Shore, MD
- McDonagh TA, Metra M, Adamo M, et al.
- Citation:
- 2021 ESC Guidelines for the Diagnosis and Treatment of Acute and Chronic Heart Failure: Developed by the Task Force for the Diagnosis and Treatment of Acute and Chronic Heart Failure of the European Society of Cardiology With the Special Contribution of the Heart Failure Association of the ESC. Eur Heart J 2021 Aug 27:.
The following are key points to remember from the 2021 European Society of Cardiology Guidelines for the Diagnosis and Treatment of Acute and Chronic Heart Failure :
New Hf Definition Stage Updates Outlined In 2022 Acc/aha/hfsa Guidelines
The new guidelines also call for better incorporation and addressing of social determinants of health.
During a panel at the American College of Cardiologys 70th Scientific Session, experts highlighted updates to the 2022 American Heart Association /ACC/Heart Failure Society of America guidelines for the management of heart failure and offered a new definition of the condition.
The syndrome of HF is defined as a complex clinical syndrome with symptoms and signs that result from structural or functional impairment, said Biykem Bozkurt, MD, PhD, guideline writing committee vice-chair and professor of Medicine-Cardiology at Baylor College of Medicine.
With regard to terminologies for HF trajectory, the guidelines emphasized the use of persistent HF as opposed to stable HF, as the term stable creates inertia, while persistent HF requires optimization, Bozkurt added. The phrase HF in remission is also preferred over HF in recovery as the majority of patients who withdraw from therapy will relapse.
Among the updates included are a redefinition of HF stages to emphasize prevention and the addition of sodiumglucose co-transporter 2 inhibitors for the treatment of symptomatic HF.
This latter inclusion comes off the heels of an FDA approval for empagliflozin, for a broader range of patients with HF, including those with preserved ejection fraction a condition with a poor prognosis and very limited treatment options.
Recommended Reading: What Age Can You Have A Heart Attack
Don’t Miss: How Long Can A Heart Attack Last Before Death
Scope Of The Guideline
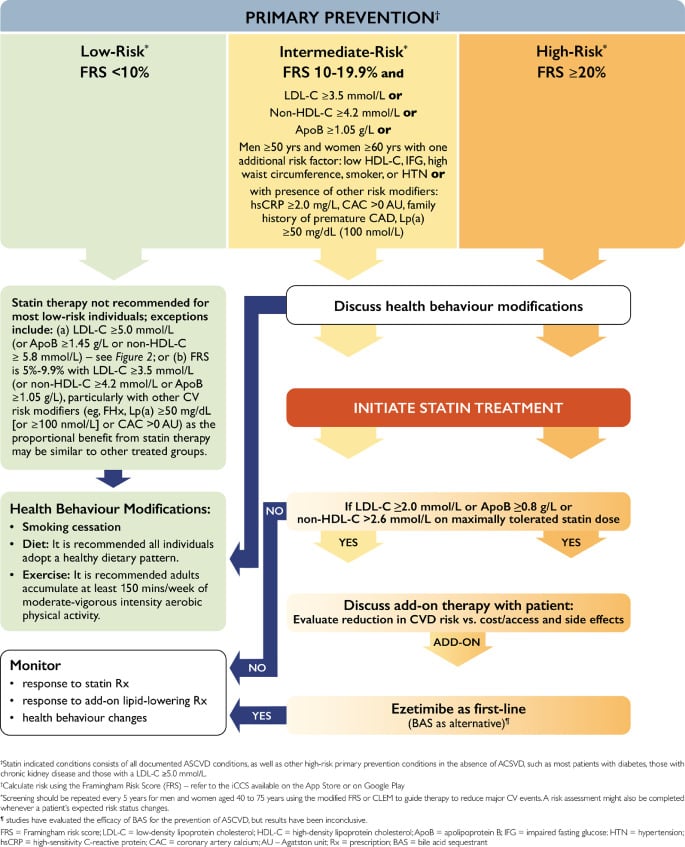
The purpose of the 2022 AHA/ACC/HFSA Guideline for the Management of Heart Failure is to provide an update and to consolidate the 2013 ACCF/AHA Guideline for the Management of Heart Failure for adults and the 2017 ACC/AHA/HFSA Focused Update of the 2013 ACCF/AHA Guideline for the Management of Heart Failure into a new document. Related ACC/AHA guidelines include recommendations relevant to HF and, in such cases, the HF guideline refers to these documents. For example, the 2019 primary prevention of cardiovascular disease guideline includes recommendations that will be useful in preventing HF, and the 2021 valvular heart disease guideline provides recommendations for mitral valve clipping in mitral regurgitation .
Iron Deficiency And Anaemia
Iron deficiency is common in patients with HF and independently predicts adverse outcome. Correction of iron deficiency with intravenous iron has been shown in the short term to improve quality of life and exercise capacity as compared with placebo. A meta-analysis recently showed potential impact on reduction in risk of HF hospitalisation.26
One of the trials in this meta-analysis, AFFIRM-AHF , evaluated whether giving IV iron influenced CV mortality and hospitalisations for heart failure.27 The trial included patients with LVEF 50% during hospitalisation for acute HF and who were iron deficient. Patients were followed up for a year, but no IV iron was given beyond the first 24 weeks. Whilst the primary end point just failed to meet significance, patients who were given IV ferric carboxymaltose after stabilisation but prior to discharge had significantly fewer subsequent hospitalisations with HF. There did not, however, appear to be an effect on mortality.
Several longer-term studies, including the UK-based IRONMAN trial, will provide further data on long-term efficacy, safety and effect on CV death.28
On the basis of the trials above, the 2021 ESC HF guidelines recommend the following:
Also Check: When Is Heart Rate Too High
Diagnosis And Treatment Of Heart Failure With Mildly Reduced Ejection Fraction And Heart Failure With Preserved Ejection Fraction
Carolyn Lam, Professor of Duke-NUS Cardiovascular Academic Clinical Programme, Singapore, presented a session on the diagnosis and treatment of HF with mildly reduced ejection fraction , and HF with preserved ejection fraction . Lam began by defining HF as a clinical syndrome consisting of cardinal symptoms that may be accompanied by signs. The speaker then went on to explain the diagnostic algorithm of HF, which begins with the clinical assessment of these signs through ECG to determine underlying cardiac abnormalities. The left ventricular ejection fraction is then assessed for HF classification an LVEF of 40% indicates HFrEF, 4149% HFmrEF, and 50% HFpEF.
One of the most notable changes from the 2016 guidelines in this area of HF is the modification of the term HF with mid-range ejection fraction to HF with mildly reduced ejection fraction. This change was implemented following evidence demonstrating that patients with HFmrEF could benefit from similar therapies to those recommended for individuals with HFrEF. A table of recommendations for HFmrEF treatment has also been added to the guidelines, an area which was previously merged with HFpEF treatments.
Palliative And Supportive Care Shared Decision
Recommendations for Palliative and Supportive Care, Shared Decision-Making, and End-of-Life
Referenced studies that support the recommendations are summarized in the .
| COR | |
|---|---|
| C-LD | |
| 1. |
For all patients with HF, palliative and supportive careincluding high-quality communication, conveyance of prognosis, clarifying goals of care, shared decision-making, symptom management, and caregiver supportshould be provided to improve QOL and relieve suffering . |
1C-LD
| 2. |
For patients with HF being considered for, or treated with, life-extending therapies, the option for discontinuation should be anticipated and discussed through the continuum of care, including at the time of initiation, and reassessed with changing medical conditions and shifting goals of care . |
2aB-R
| 3. |
For patients with HFparticularly stage D HF patients being evaluated for advanced therapies, patients requiring inotropic support or temporary mechanical support, patients experiencing uncontrolled symptoms, major medical decisions, or multimorbidity, frailty, and cognitive impairmentspecialist palliative care consultation can be useful to improve QOL and relieve suffering . |
2aC-LD
| 4. |
For patients with HF, execution of advance care directives can be useful to improve documentation of treatment preferences, delivery of patient-centered care, and dying in preferred place . |
2aC-LD
| 5. |
In patients with advanced HF with expected survival < 6 months, timely referral to hospice can be useful to improve QOL . |
Synopsis
Also Check: What Is Congestive Heart Failure
American College Of Cardiology/american Heart Association/heart Failure Society Of America Recommendations For Genetic Evaluation And Testing
Genetic screening and counseling are recommended for first-degree relatives of selected individuals with genetic or inherited cardiomyopathies to detect cardiac disease and to encourage review of therapies for lowering HF progression and sudden death.
It is reasonable to refer select patients with nonischemic cardiomyopathy for genetic counseling and testing to identify conditions that could guide treatments for patients and family member.
Strategic Phenotypic Overview Of The Management Of Heart Failure With Reduced Ejection Fraction
In addition to the general therapies considered in section 5, other therapies are appropriate to consider in selected patients. These are covered in detail in later sections. Some of the main ones are depicted in Figure . The effect of some interventions on symptoms/QOL are outlined in Supplementary Table 9.
Also Check: Congestive Heart Failure Exercise
European Society Of Cardiology Guidelines For Genetic Counseling And Testing
Arrhythmogenic cardiomyopathy
Offer genetic counseling and testing all patients with suspected ACM and all first-degree adult relatives of patients with ACM and a disease-causing mutation, regardless of their phenotype to preclinically identify genetically affected individuals.
Genetic family screening may also be used for arrhythmic risk stratification.
First-degree relatives with the same definite disease-causing mutation as the patient should undergo clinical evaluation, electrocardiography , echocardiography, and possibly cardiac magnetic resonance imaging . In the setting of no definite identified genetic mutation in the patient or no genetic testing is undertaken, consider clinical evaluation in first-degree adult relatives with ECG and echocardiography, and repeat every 2-5 years or less if nondiagnostic abnormalities are present.
Dilated cardiomyopathy or hypokinetic nondilated cardiomyopathy
All patients with suspected DCM or HNDC and all first-degree adult relatives of such patients and a definite disease-causing mutation, regardless of their phenotype, should undergo genetic counseling and testing to preclinically identify genetically affected individuals. Repeat the evaluation every 5 years or less in first-degree adult relatives when aged younger than 50 years or in the presence of nondiagnostic abnormalities.
All first-degree relatives of patients should undergo clinical evaluation, ECG, echocardiography, and possibly CMRI.
Hypertrophic cardiomyopathy
Relationships With Industry And Other Entities
The ACC and AHA have rigorous policies and methods to ensure that documents are developed without bias or improper influence. The complete policy on relationships with industry and other entities can be found online. of the guideline lists writing committee members relevant RWI for the purposes of full transparency, their comprehensive disclosure information is available in a . Comprehensive disclosure information for the Joint Committee is also available online.
Read Also: When Did Bob Harper Have His Heart Attack
The Background To Heart Failure With Preserved Ejection Fraction
This guideline acknowledges the historical changes in nomenclature and the lack of consensus on the optimal LVEF cut-off to define the group of patients with HF without overtly reduced EF. The term preserved was originally proposed in the Candesartan in Heart failure: Assessment of Reduction in Mortality and morbidity Programme to refer to patients with an EF that was not clearly reduced or completely normal. While the current guidelines have designated patients with an LVEF 4149% as HFmrEF, we recognize that there will be debate about what constitutes mildly reduced EF, what these EF cut-offs should be, and whether they should be different for men and women., The EACVI defines systolic dysfunction as being < 52% for males and < 54% for females.
