How Common Are Heart Attacks
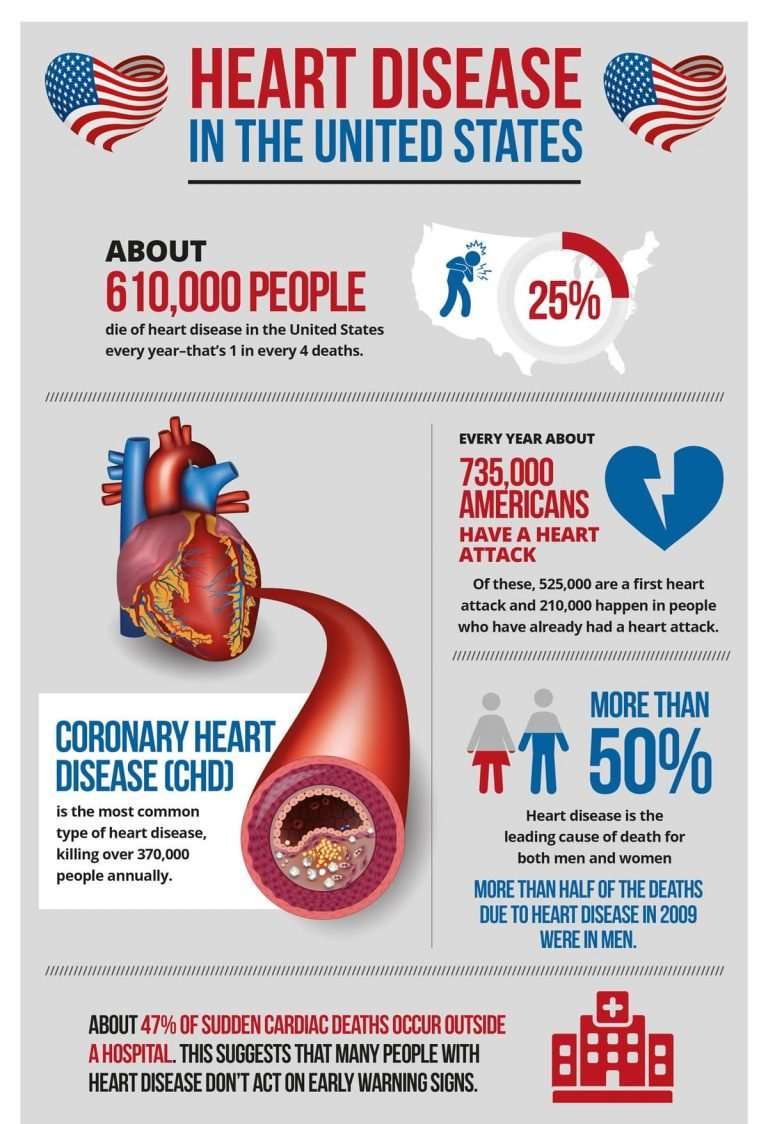
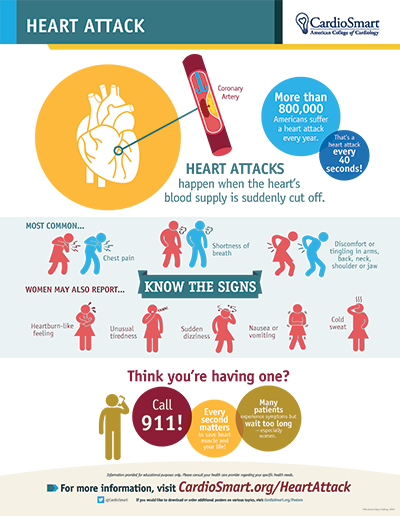
A heart attack;strikes someone about every 43 seconds. It occurs when the blood flow that brings oxygen to the heart muscle is severely reduced or cut off completely. This happens because the arteries that supply the heart with blood can slowly narrow from a buildup of fat, cholesterol;and other substances .
How Do I Recover From A Heart Attack
To recover, it’s important to partake in cardiac rehabilitation, an outpatient program that uses medically supervised exercise usually an average of three times per week for three months. It also includes nutrition counseling and risk management to help you maintain a healthy weight or quit smoking.
One study found that cardiac rehab helped reduce chances of a repeat heart attack by 47 percent. Another found patients who participated in cardiac rehab were 42 percent less likely to die within an average of eight years.
Research has found that any physical activity after a heart attack can be helpful, but the goal should be regular physical activity. A healthy diet that limits sugar, saturated fat and sodium also is important, Goldberg said.
The Mediterranean diet;emphasizes fruits and vegetables and little red meat. The DASH diet, which stands for Dietary Approaches to Stop Hypertension, also incorporates a variety of fruits and vegetables, whole grains, skinless poultry and fish, nuts and legumes, low-fat dairy products and non-tropical oils.
Another important element of recovery is finding a support system, Goldberg said. Isolation can be a marker for a recurrent heart attack and death.
Rely on family, friends or your house of worship for emotional support. Reach out to support networks or seek professional help. One study found returning to work also can help combat post-heart attack depression.
How Slow Is Too Slow
Doctors consider a;heart rate below 60 beats per minute as low, Dr. Baez-Escudero says.
If you have bradycardia, youll have a sustained heart rate below 60 even when youre awake and active. A normal range is from 60 to 100 beats-per-minute while awake. The heart rate can also slow down normally while we are asleep to 40 to 60 beats a minute.
Read Also: Why Does Your Heart Rate Go Up When You Exercise
What To Expect At The Doctors
Your doctor may use a variety of diagnostic tools to help diagnose your condition, including:
- Electrocardiogram. Also referred to as an ECG or EKG, this diagnostic tool uses small electrodes to record the electrical activity of your heart. Your doctor can use the information collected to determine if heart abnormalities are contributing to your condition.
- Imaging tests. Imaging can be used to assess if there are any structural abnormalities in your heart that may be contributing to your condition. Possible imaging tests can include echocardiogram, CT scan, and MRI scan.
- Laboratory tests. Your doctor may order blood tests to determine if your condition is caused by something such as an electrolyte imbalance or thyroid disease.
Once a diagnosis is made, your doctor will work with you to develop a plan to treat and manage your condition.
Depending on the findings from the diagnostic tests, your doctor may refer you to a cardiologist. A cardiologist specializes in treating and preventing diseases of the heart and circulatory system.
How To Check Your Heart Rate
Bernard Kim, M.D. contributes to topics such as Cardiology.
George Batsides, M.D. contributes to topics such as Cardiothoracic Surgery.
Like the check-engine light on your car, your vital signs can alert you when somethings wrong so you can get your vehicle to a mechanicor rather, your body to a doctorbefore it breaks down.
Knowledge is power, says George Batsides, M.D., chief of cardiac surgery at Hackensack University Medical Center. The more data you have about your body, the better off youre going to be.
One of the most important vital signs to monitor on a regular basis is your heart rate, or pulse. Although its not a perfect indicator, measuring it both at rest and during exercise can give you a sense of your overall physical fitness and maybe even your risk for a heart attack.
Follow these tips to calculate it and keep track of it:
There are two different heart rates:
- Resting heart rate, which is your pulse when youre inactive and sedentary
- Maximum predicted heart rate, which is your pulse when youre exercising at maximum effort
Before you measure either, its important to know whats normal:
Once you know whats normal for someone of your age, you can take your pulse and compare it. You can measure your heart rate manually or electronically.
Recommended Reading: How To Stop Heart Palpitations Due To Anxiety
What Is An Irregular Pulse
An irregular pulse is when the heart doesn’t beat in a regular, steady rhythm. This is also called an irregular heart rate or an arrhythmia.
If your heart rate is irregular, you may notice that your pulse:
- seems irregular or is ‘jumping around’
- is racing, even when you’re at rest
- seems unusually slow some or most of the time.
Your Heart Rate Isnt Always Predictable
How this cardiac event affects the heart rate isnt always predictable.
Certain medications may slow your heart rate
For example, if youre on a medication that slows your heart rate, such as a beta-blocker for heart disease, your heart rate may remain slow during a heart attack. Or if you have a type of heart rhythm disturbance called bradycardia, in which your heart rate is perpetually slower than normal, a heart attack may do nothing to increase the rate.
There are certain types of heart attacks that can lead to an abnormal slowing of the heart rate because they affect the electrical tissue cells of the heart.
Tachycardia may speed your heart rate
On the other hand, if you have tachycardia, in which your heart always or frequently beats abnormally fast, then that pattern could continue during a heart attack. Or, certain types of heart attacks can cause the heart rate to increase.
Finally, if you have some other condition thats causing your heart to beat fast, such as sepsis or infection, then it could be causing the stress on your heart rather than being a result of the blockage to blood flow.
Many people live with tachycardia and have no other symptoms or complications. However, if you consistently have a rapid resting heart rate, you should absolutely have your cardiovascular health evaluated.
- lightheadedness
- a vague sense of impending doom
If you think you or a loved one may be having a heart attack, call 911 immediately.
Also Check: What Does Heart Rate Mean
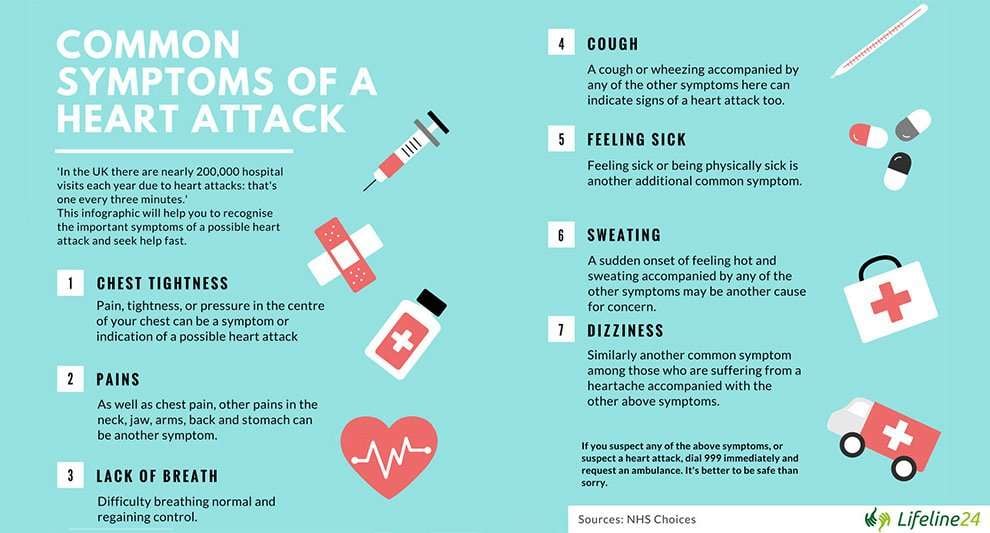
Breaking Out In A Cold Sweat
Another common symptom is finding yourself breaking out in a cold sweat. The reason behind this symptom is that when you have clogged arteries, your heart requires more effort to pump blood, and sweating keeps your bodys temperature down during this extra effort.
For women, this means night sweats may not just be the result of menopause. They might also be a sign of heart problems.
If you experience any of these symptoms, make sure to consult your physician. Dont wait until it becomes urgent.
Shortness Of Breath Nausea And Lightheadedness
Shortness of breath can occur with or without a chest pain during a heart attack. Most people dont realize this can happen before or after a heart attack as wellespecially for women..
Research has found that shortness of breath is the third most reported symptom before a heart attack among women and the top symptom during a heart attack.
Read Also: How To Calculate Resting Heart Rate
When To Contact A Medical Professional
If you have never had heart palpitations before, see your provider.
- Loss of alertness
- Dizziness or lightheadedness
- You often feel extra heartbeats .
- You have risk factors for heart disease, such as high cholesterol, diabetes, or high blood pressure.
- You have new or different heart palpitations.
- Your pulse is more than 100 beats per minute .
- You have related symptoms, such as chest pain, shortness of breath, feeling faint, or loss of consciousness.
What Happens To Your Heart Rate During A Panic Attack
In many cases, a panic attack triggers a fast heart rate, also known as tachycardia. The heart rate may speed up to 200 beats per minute or even faster.
A fast heart rate can make you feel lightheaded and short of breath. Or you might feel fluttering or pounding in the chest. Usually, tachycardia that happens in response to emotional stress and only lasts a few minutes is not harmful. But if it happens regularly, or you have possible symptoms of a heart attack, seek medical care.
Read Also: What Branch Of Medicine Deals With Heart Disease
Shortness Of Breath Or Chest Pain After Covid
Shortness of Breath
You want to consult a doctor if any of your symptoms are severe, especially shortness of breath, Post says. She recommends using a commercially available O2 saturation monitor.
Shortness of breath by itself is not always a sign of a serious problem, but if you have that symptom along with low O2 , that is a reason to be concerned. Sometimes people are short of breath with exertion after COVID-19 because they have been less active for a long time and need to gradually build their fitness level back up.
COVID-19 Chest Pain
What about lingering chest pain, another common post-COVID complaint? Chest pain may be nothing serious, but if you are having severe chest pain, get help, especially if it is persistent or if you are also having nausea, shortness of breath or lightheadedness: These could be symptoms of a heart attack.
If you have chest pain when you inhale, you might have lung inflammation. Sudden, severe chest pain could be a blood clot in the lung , Post says.
Family doctor or cardiologist?
If your symptoms are not severe but you want to be checked out, Post says a cardiologist doesnt need to be your first stop if youve never had heart problems before and are not at risk. For nonemergency post-COVID-19 symptoms, your primary care practitioner can advise you, she says.
Heart Failure and COVID-19
- Shortness of breath, especially with exertion
- Fatigue
- Shortness of breath when lying down
- Leg swelling
- Frequent urination at night
Causes Of A Slow Heart Rate
Its normal for your heart rate to change throughout the day. It speeds up when you exercise, slows down as you recover from exercising, and is usually at its lowest while you sleep.
Sometimes people have a slower heart rate than normal. This is called bradycardia, and it isnt necessarily a problem. Its diagnosed when your heart beats less than 60 beats per minute.
There are several causes of a slow heart rate. The most common are being young or physically fit. The heart is a muscle, and just like the other muscles in your body, it responds positively to exercise. When youre in good shape, your heart doesnt need to beat as often to supply your body with enough oxygen.
But a slow heart rate can also be a sign of a medical problem, such as a heart condition. If your resting heart rate is slow and you have other symptoms of bradycardia such as lightheadedness, call your doctor or go to the ER.
Read Also: What Causes Heart Rate To Spike
Watch For Subtle Signs Of A Heart Attack
A heart attack might seem like it came out of nowhere. But in many cases, chest pain due to heart disease, known as angina, appears in the days or weeks before a cardiac event.
You may feel a twinge or some pain in the shoulder or chest but think its something else, says Dr. Miller. The symptoms go away. Then later, the pain gets worse, or you feel a little off. Then the heart attack hits. These early signs can be hard to identify.
When Heart Rate Or Rhythm Changes Are More Serious
Irregular heartbeats change the amount of blood that flows to the lungs and other parts of the body. The amount of blood that the heart pumps may be decreased when the heart pumps too slow or too fast.
Changes such as atrial fibrillation that start in the upper chambers of the heart can be serious, because they increase your risk of forming blood clots in your heart. This in turn can increase your risk for having a stroke or a blood clot in your lungs . People who have heart disease, heart failure, or a history of heart attack should be more concerned with any changes in their usual heart rhythm or rate.
Fast heart rhythms that begin in the lower chambers of the heart are called ventricular arrhythmias. They include ventricular tachycardia and ventricular fibrillation. These types of heart rhythms make it hard for the heart to pump enough blood to the brain or the rest of the body and can be life-threatening. Ventricular arrhythmias may be caused by heart disease such as heart valve problems, impaired blood flow to the heart muscle , a weakened heart muscle , or heart failure.
Symptoms of ventricular tachycardia include palpitations, feeling dizzy or light-headed, shortness of breath, chest pain or pressure, and fainting or near-fainting. Ventricular fibrillation may cause fainting within seconds and causes death if not treated. Emergency medical treatment may include medicines and electrical shock .
Check your symptoms to decide if and when you should see a doctor.
A New Class Of Drugs To Reduce Heart Rate
A new class of agents selective If inhibitors is now under investigation . The first in its class to be studied is ivabradine, which acts specifically on the sinoatrial node. Administered to rats with heart failure, ivabradine promoted long-term heart rate reduction while improving LV function, increasing stroke volume, and preserving cardiac output despite the heart rate reduction . Part of this improvement may be attributable to ivabradines modifications in the extracellular matrix and/or function of myocytes as a consequence of long-term heart rate reduction.
The INternatIonal TrIAl on the Treatment of angina with IVabradinE vs atenolol study in humans has shown that ivabradine is as effective as atenolol in patients with stable angina. The morBidity-mortality EvAlUaTion of the If inhibitor ivabradine in patients with coronary disease and left ventricULar dys-function study, evaluating ivabradine in patients with coronary disease and LV dysfunction, began in January 2005; 10,947 subjects have completed the study, and results are expected in late 2008. On Top Of BB is a four-month randomized, double-blind, parallel-group multicentre study that is evaluating the antianginal efficacy and safety of oral ivabradine on top of therapy with atenolol in patients with stable angina pectoris that started in 2005 and has just been completed; results are expected to be published in 2008.
Is A Heart Attack More Likely After Covid
That depends: Post says that heart attack has several different forms. A type 1 heart attack, caused by a blood clot blocking one of the hearts arteries, is rare during or after COVID-19 infection.
Type 2 heart attacks are more common with COVID-19, she says. This heart attack can be caused by increased stress on the heart, such as a fast heartbeat, low blood oxygen levels or anemia, because the heart muscle isnt getting enough oxygen delivered in the blood in order do this extra work. We have seen this in people with acute coronavirus disease, but it is less common in those who have survived the illness.
Blood tests have shown that during COVID-19, some people have elevated levels of a substance called troponin in their blood, along with EKG changes and chest pain. Elevated troponin levels are a sign of damaged heart tissue. Sometimes this is from a heart attack. This is less commonly seen after COVID-19.
During acute COVID-19, elevated troponin levels with an abnormal EKG are linked to higher mortality, but not in patients with a normal EKG, Post says.
Myth: If My Heart Rate Is Slow It Means I Have A Weak Heart
Not necessarily. A slow heart rate can be a sign that you’re healthy and fit. An athlete’s heart muscle is in better shape, so it doesn’t have to work as hard to keep up a steady beat.
In general, Patel says, slow rates are only a problem if you also pass out, feel dizzy, are short of breath, or have chest pain. See your doctor if you have any of those symptoms.
Can A Heart Attack Feel Like The Flu
Even though heart disease is the No. 1 killer of women in the United States, women often chalk up the symptoms to less life-threatening conditions like acid reflux, the flu or normal aging.They do this because they are scared and because they put their families first, Goldberg said. There are still many women who are shocked that they could be having a heart attack.
What Is A Heart Attack
A heart attack, also called a myocardial infarction, happens when a part of the heart muscle doesnt get enough blood.
The more time that passes without treatment to restore blood flow, the greater the damage to the heart muscle.
Coronary artery disease ;is the main cause of heart attack. A less common cause is a severe spasm, or sudden contraction, of a coronary artery that can stop blood flow to the heart muscle.
Exercise And Heart Rate
Like any other muscle, your heart needs exercise to keep it fit and healthy. Regular exercise can help reduce your risk of heart disease and other health conditions, such as diabetes.
To keep your heart healthy, you should aim to do 150 minutes of low to moderate intensity exercise a week. If you have a heart condition, talk to your doctor about what exercise and target heart rates are safe for you.
One way to measure the intensity of your exercise is by using your heart rate. To exercise at a low to moderate intensity your heart rate should be at 50 to 70% of your approximate maximum heart rate.
The easiest way to get an approximate maximum heart rate is to calculate 220 your age. You then need to calculate 50 to 70% of your MHR.
For example, if you’re 40-years-old:
- your approximate maximum heart rate is: 220 40 = 180 beats per minute
- 50% of your MHR is 180 X 0.5 = 90 bpm
- 70% of your MHF is 180 X 0.7 = 126 bpm.
Alternatively, you can use our heart rate chart below to get a rough idea.
Remember if you’re on medications to slow your heart rate down, you may not be able to meet these upper heart rates and the aim should be to exercise at a rate that makes you lightly puff.
