Risk Factors For Heart Failure
Health conditions that left unrecognized or untreated will increase the lifetime risk of developing heart failure. Some of these diseases include:
- Coronary heart disease and heart attacks
- High blood pressure
- Diabetes
- Obesity
Unhealthy behaviors can also increase your risk for heart failure, especially for people who have one of the diseases listed above. Unhealthy behaviors include:
- Smoking or using tobacco
- Use of illegal drugs, like methamphetamines or even excessive alcohol intake
- Eating foods high in fat, cholesterol, and sodium
- Not getting enough physical activity
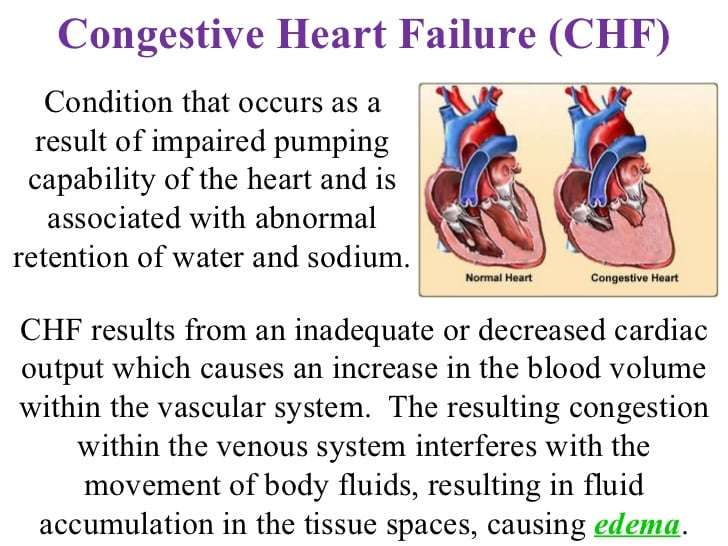
Congestive Heart Failure Causes
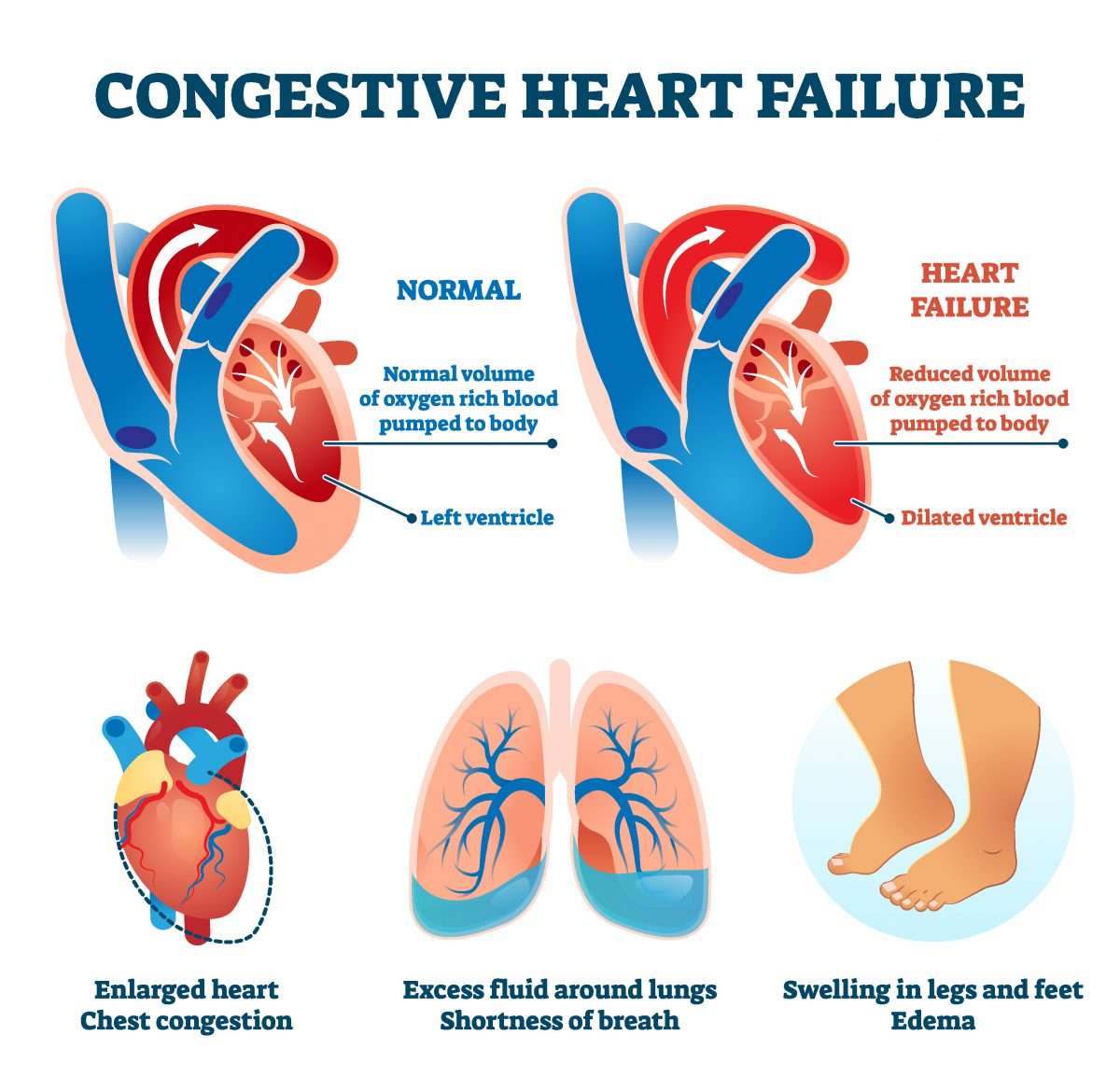
Congestive heart failure stages of dying frequently develop right after other conditions have damaged or weakened your heart. However, the heart doesnt need to become weakened to cause CHF. It can also happen if the heart becomes way too stiff.
When it comes to a result of CHF, the main pumping chambers of your heart may become stiff and not fill properly between beats. In many cases of heart failure, your heart muscle tissue may become damaged and weakened, and the ventricles stretch to the point that the heart cant push blood effectively throughout your body.
Severe lung disease When the lungs dont work properly, the heart needs to work harder to get available oxygen to the entire body.
How Long Can You Live With End
Heart failure is a chronic, progressive condition that worsens with each flare-up. Your outlook and prognosis are better if you are healthy overall, you have been following your treatment plan, and you are responding well to your treatments. Being willing to pursue invasive treatments like a heart transplant will also increase your life expectancy.
Recommended Reading: Is Angioplasty Considered Heart Surgery
Support Them To Make Decisions About Treatments
As well as having an advance care plan, patients should be given the chance to discuss the following issues:
- Whether to deactivate an implantable cardioverter defibrillator , if they have one. This can prevent the ICD activating at the end of life, which can be distressing.
- What the patient would want to happen if they had a cardiac arrest. They may decide they do not want to have cardiopulmonary resuscitation .
- When to stop medication that no longer reduces symptoms or improves their quality of life. This can be a difficult conversation and it’s best carried out sooner rather than later. Make sure the patient and the people important to them understand what changes are being made to their medication and why.
What Are The Risk Factors Of Congestive Heart Failure
Congestive heart failure primarily originates from problems with cardiovascular system of the body. Thus, it gets extremely important to go for regular routine checkups to ensure proper functioning of the heart and its valves. The risk factors include-
Hypertension: Increased blood pressure may lead to congestive heart failure. Hypertension is one of the chief causes of increased blood pressure.
Artery Blockage: Blockages in the arteries can lead to congestive heart failure. These blockages occur due to accumulation of fat and cholesterol in the blood vessels. Thus increased cholesterol content in the blood is a risk factor. Such blockages inhibit proper blood from the blood vessels thereby damaging them.
Heart Valve Conditions: This brings to the next risk factor which is the heart valve condition. Heart valves are extremely important as they carry blood to and fro from the heart to the organs in the body. In case these valves are damaged due to leak or blockage, the circulation gets affected. In turn the human heart pumps the blood harder which can lead to heart infection.
Also Read:
Don’t Miss: How High Can Your Heart Rate Go
What Determines Life Expectancy
Some things that affect your life expectancy with heart failure are out of your control, such as your age. Others, such as a healthy lifestyle, are not.
Things that may affect life expectancy include:
Ejection fraction. To get a better picture of your heart health, your doctor will check how well an area of your heart called the left ventricle pumps out blood. An echocardiogram is one test thatâs often used. It scans the heart and takes measurements to find out what percentage of your blood is being pumped out with each heartbeat. For instance, an ejection fraction of 55% means that 55% of your blood is being pushed out with each thump. A normal result usually falls between 50% and 70%, according to the American Heart Association.
People with a reduced ejection fraction have one type of the condition. Itâs called heart failure with reduced left ventricular function. With the other type, heart failure with preserved left ventricular function, the percentage isnât below normal. But there are other changes, such as the heart becoming stiffer. âAfter the heart squeezes and pumps blood forward, it has to relax to fill with blood,â Lampert says. âWhen the heart muscle is stiff or unable to relax as blood is trying to rush in and fill it, itâs not very compliant, and so you can get that same results of fluid backing up into the lungs and other parts of the body.â
Staging. There are four stages of heart failure, which indicate how serious your condition may be.
How Does Heart Failure Impact People At End Of Life
Heart failure can have a serious psychological impact on people, leading to feelings like worry, sadness or anger. Patients may experience a mix of good and bad days, and the lack of control over their limitations can be very frustrating. As the disease advances, symptoms can fluctuate dramatically, which makes evaluating how long the patient is expected to live more challenging.
Also Check: What Are The Symptoms Of A Heart Attack Or Stroke
Acute Or Chronic Heart Failure
Heart failure can be acute or chronic.
Acute heart failure happens when either:
- symptoms come on suddenly
- it’s the first time the patient has had heart failure
- symptoms suddenly become worse during chronic heart failure.
Chronic heart failure is when someone’s heart failure develops gradually over time and is a long-term condition.
What You Can Do
Some risk factors of heart failure, like age, cant be modified. Still, people with CHF can take steps to improve the long-term prognosis. The first thing to do is to be familiar with any family history of heart disease. You’ll also want to learn about all the possible symptoms. Don’t ignore any symptom that you think is cause for concern. Tell your healthcare provider about them right away.
Regular exercise, along with managing any other health issues you may have, can also help to keep CHF under control.
You May Like: How To Get Your Heart Rate
Lasting Power Of Attorney
A lasting power of attorney is a legal document where you appoint one or more people to help you make decisions or to make decisions on your behalf. This gives you more control over what happens to you if you are unwell and unable to make your own decisions.
-
Find out more about making a lasting power of attorney.
When To Seek Hospice Care
Even physicians have difficulty determining life expectancy for people with end-stage heart-failure. The condition can be unpredictable, and symptoms can change. However, certain signs can indicate that hospice care would be beneficial, including:
- frequent chest pain
- significant fatigue or shortness of breath
- substantial decline in ability to do daily activities, such as self-care
- The patient has already received the best possible treatment, which are no longer working well, and the patient is not a candidate for other interventions.
- The patient has received the best possible treatment and has decided to decline further specialized interventions.
People can be reluctant to start hospice, as they may worry it means theyre giving up or that it will hasten death. But such concerns are unfounded. In fact, patients and families often wish they had started hospice sooner, because it makes such a positive difference in their lives. And research shows that early admission to hospice results in greater satisfaction with care among patients and family caregivers.
Also Check: What Is Heart Palpitations Symptoms
Prognosis At Different Ages
In general, younger people diagnosed with CHF tend to have a better outlook than older people.
A report averaging several smaller studies found that people under age 65 generally had a 5-year survival rate of 78.8 percent following CHF diagnosis. The same report found that people over age 75 had an average 5-year survival rate of 49.5 percent following diagnosis.
Older people diagnosed with CHF may already have other chronic health conditions. This can make it difficult to manage CHF and create a more challenging outlook for them.
for congestive heart failure. The treatment thats best for you will depend on:
- your overall health
- any other health conditions you have
- how you respond to any medications
- what stage of CHF you have
Common options include:
There are lifestyle changes a person with CHF can make that have been shown to help slow the conditions progression. Talk with your doctor before making changes to your diet or starting an exercise routine.
What Are The Symptoms Of End
Heart Failure: Quick Facts
1. More than 6 million U.S. adults have heart failure.
2. About half of people who develop heart failure die within 5 years of diagnosis.
3. Most people with end-stage heart failure have a life expectancy of less than 1 year.
4. The leading causes of heart failure are diseases that damage the heart, such as heart disease, high blood pressure, and diabetes.
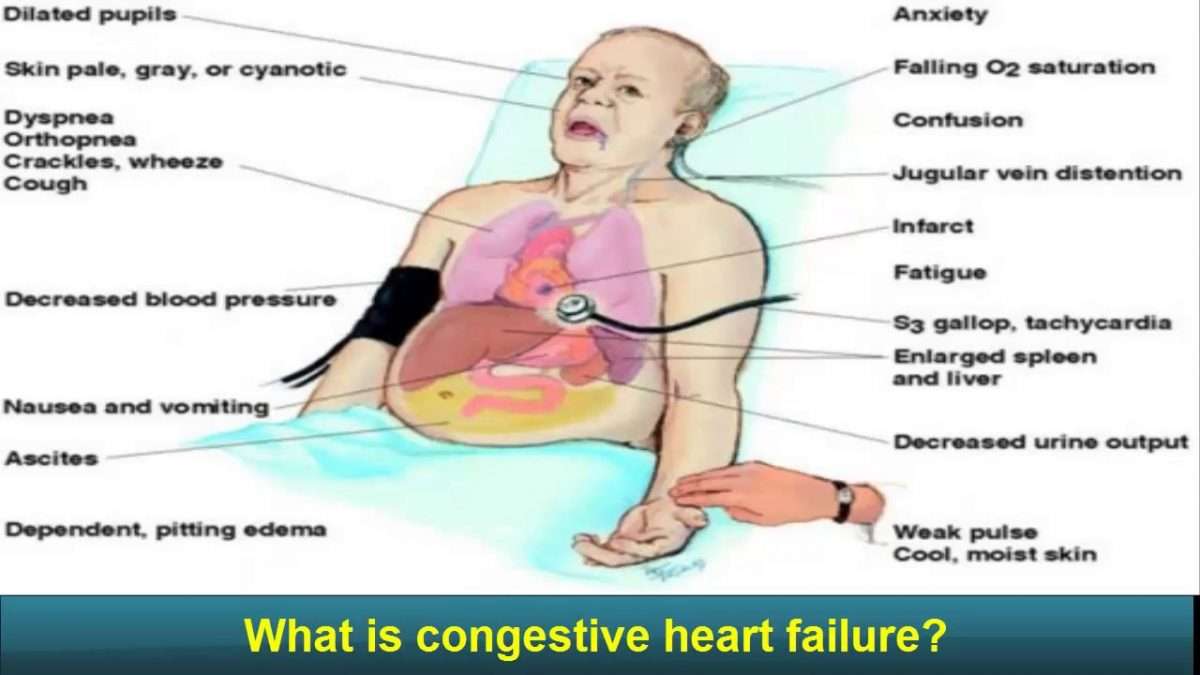
Heart failure worsens over time, so symptoms are most severe during the final stages. It causes fluid to build up in the body, which produces many of these symptoms:
- Shortness of breath . In the final stages of heart failure, people feel breathless both during activity and at rest.
- Persistent coughing or wheezing. This may produce white or pink mucus. The cough may be worse at night or when lying down.
- Weight gain or swelling of the feet, ankles, legs, abdomen, or neck veins.
- Tiredness, weakness.
In addition, people in the final stages of heart failure may suffer from:
- depression, fear, insomnia, and isolation
- anxiety about their future
- trouble navigating the health care system
Read Also: Why Does Anxiety Cause Heart Palpitations
What Can Hospice Do For A Patient With Congestive Heart Failure Or Heart Disease
Your hospice team evaluates the patients status and updates the plan of care as CHF or heart disease symptoms and conditions change, even on a day-to-day basis. The goal of hospice is to manage symptoms and relieve physical/emotional distress so patients can live as fully as possible, retain their dignity and remain comfortable at home.
The hospice plan of care treats a wide range of heart disease symptoms, including:
- Shortness of breath
- Functional decline
- Hypertension
When you turn to hospice, you are not alone in your journey your hospice care team is educated and experienced in advanced cardiac care, such as:
- Monitoring and managing your symptoms
- Communicating with your cardiologists office to intervene early and stabilize worsening conditions
- Providing medication, oxygen and other medical equipment related to your heart disease
- Providing services to reduce acute symptoms and avoid re-hospitalization
- Providing an average of 5 home visits per week and proactive phone calls
Hospice offers comprehensive services for patients with heart disease, such as:
How Can Hospice Help Heart Disease And Heart Failure Patients
Many patients will have lived with congestive heart failure for a long time before reaching the point where hospice is considered. It is important to understand that even though treatment can no longer be given to lengthen a persons life significantly, there are still ways that their quality of life and comfort can be increased, and that is where hospice can prove valuable.
Hospice care is given to patients who are expected to live for six months or less. Although it may be difficult to determine just how long patients with this condition will live, worsening symptoms and deliberately turning down the opportunity to get life-extending treatment are both signs it is time to give hospice serious consideration.
It is important not to wait too long to contact hospice most families report that they wish they had started it sooner after seeing how much it helps. If you suspect your loved one is ready for hospice, talk to your doctor and request a hospice evaluation.
You May Like: Does Stress Increase Heart Rate
Prognosis By Ejection Fraction
Ejection fraction is a measure of how much blood is pumped out of your heart each time it contracts. A healthy heart has an EF of between about 55 percent to 75 percent.
Some people with CHF have a reduced EF. This means their heart is pumping less blood out to the rest of their body than a healthy heart. Studies have shown that people who have CHF and a reduced EF have a more challenging outlook than people with CHF who do not have a reduced EF.
The exact survival rates varied among studies, but have shown that EF has an impact on prognosis. Your doctor will have the best information about how your ejection fraction can affect your prognosis.
Prognosis At Each Stage
The outlook for CHF varies greatly between people, as there are many contributing factors for every individuals situation. However, generally speaking, if CHF is discovered in its earlier stages and properly managed, you can expect a far better outlook than if its discovered much later.
Some people whose CHF is discovered early and treated promptly and effectively can hope to have a nearly standard life expectancy.
Read Also: What Is The Medical Term Of Heart Attack
What Is The Outlook With Heart Failure
With the right care, congestive heart failure wont stop you from doing the things you enjoy. Your prognosis, or outlook for the future, will depend on:
- How well your heart muscle is working.
- Your symptoms.
- How well you respond to your treatment plan.
- How well you follow your treatment plan.
One study says that people with heart failure have a life span 10 years shorter than those who dont have heart failure. Another study showed that the survival rates of people with chronic heart failure were 80% to 90% for one year, but that dropped to 50% to 60% for year five and down to 30% for 10 years.
A different study found that people who had heart failure and were discharged from the hospital had expected life spans ranging from three to 20 years, depending on various factors like age and gender. Its important to look at your specific situation when considering your prognosis.
I Decline In Clinical Status Guidelines
These changes in clinical variables are listed in order of their likelihood to predict poor survival, the most predictive first and the least predictive last. No specific number of variables must be met, but fewer of those listed first and more of those listed last would be expected to predict longevity of six months or less.
You May Like: Do Veins Carry Blood Away From The Heart
How Palliative And Hospice Care Can Help With End
Both palliative and hospice care focus on the whole person, including their physical, emotional, social, and spiritual needs. The main difference is that palliative care can be given at any time during a serious illness, and hospice care is given near the end of life typically when a persons prognosis is six months or less.
Palliative and hospice care can also provide help with making difficult treatment decisions, such as whether to be resuscitated if the persons heart stops, or whether to have a tube placed in their throat to help them breathe.
Similarly, people with end-stage heart failure may need to decide when to disable certain medical devices implanted in their body:
- Implantable cardioverter defibrillator . Patients can have the shock function turned off, or not replace the battery when the current one runs out. Electrical shocks from ICDs can cause unnecessary distress for patients and loved ones at the end of life.
- Left ventricular assist device . Typically, the patient decides when this heart pump will be shut off before it is implanted. The decision can be discussed again as the end of life nears.
Signs Of A Dog Dying Of Heart Failure
If your dog has just been diagnosed with congestive heart failure, you likely have many questions about what this means for their future.
CHF is a serious condition that cannot be cured, but can be managed over time with proper care. So how do you know if your dog is beginning to suffer in their condition?
In this article we will discuss the details of CHF in dogs, and help you understand the signs of a dog dying of heart failure.
You May Like: How To Treat Heart Palpitations
What Are The Symptoms
Some are easy to confuse with normal aging or other diseases. The more advanced your heart failure, the more likely you are to have many symptoms, or the changes that youâve noticed in yourself will worsen.
These are common ways that heart failure can affect you:
Shortness of breath. Heart failure can make it hard to breathe when you walk up a flight of stairs. With advanced heart failure, you may get winded in a shorter period of time, or you may have trouble even when youâre sitting still.
Sleep problems. Heart failure can make it hard to breathe or catch your breath when you lie in bed. You may have trouble nodding off to sleep, or you might wake up in the middle of the night gasping for air. Try sleeping while propped up on two or more pillows instead of lying flat. Advanced heart failure makes it even more likely youâll have trouble breathing when youâre at rest. That means your bedtime problems will probably get worse, too.
Coughing. You may already have a dry cough that acts up when youâre lying in bed. You might cough often during the day, and your phlegm could have a slight pink tint to it. That means thereâs a bit of blood in the gunk youâre coughing up. Advanced heart failure can make that cough worse, especially when youâre lying down.
Fatigue. Heart failure can make you feel worn out. Things that wouldnât have tired you out in the past suddenly do. Youâre more likely to feel tired all of the time with advanced heart failure.
Show Sources
