Stage C Treatment Options
Treatment at this stage focuses on managing your symptoms, optimizing your heart function, and preventing worsening of your condition.
Medications to treat stage C heart failure include:
- Diuretics to reduce fluid retention
- Beta blockers to help make your heart work less hard
- SGLT2 inhibitors to reduce the risk of cardiovascular death and hospitalization for heart failure
- Angiotensin-converting enzyme inhibitors
- Angiotensin II receptor blockers
- Entresto , which reduces the risk of death and hospitalization among patients with chronic heart failure
- Aldosterone antagonists
- Digoxin to help the heart beat stronger and more regularly
- Possible cardiac resynchronization therapy
- Possible implantable cardiac defibrillator therapy
In addition to the lifestyle changes for stages A and B, you may need to make the following changes:
- Reduce your sodium intake
- Restrict fluid intake
- Keep track of your weight daily
Remember that even if the treatment causes your symptoms to get better or stop, you still need to continue treatment to slow the progression of your condition to stage D.
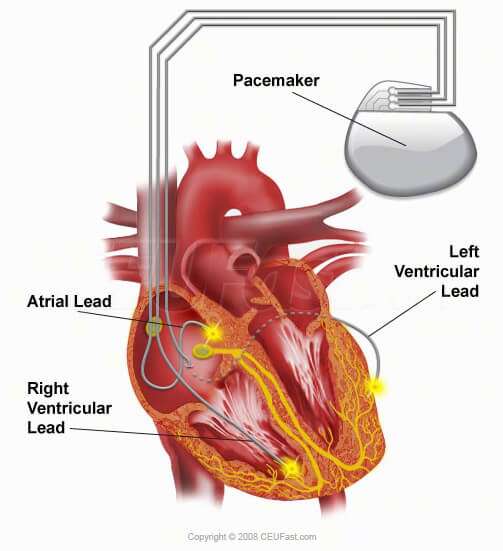
How Are Pacemakers Implanted
Pacemakers are implanted two ways:
- Endocardial approach. This is the most common technique used.
- This procedure is done in a pacemaker or electrophysiology lab.
- A local anesthetic is given to numb the area. A cut is made in the chest where the leads and pacemaker are inserted.
- The lead is inserted through the incision and into a vein, then guided to the heart with the aid of a fluoroscopy machine.
- The lead tip attaches to the heart muscle, while the other end of the lead is placed in a pocket created under the skin in the upper chest.
The doctor will determine which pacemaker implant method is best for you.
Where Does It Go And How Is It Put In Place
A pacemaker is usually implanted under local anaesthetic, just below your collarbone with leads coming from it that are positioned in your heart. The procedure usually takes 30-60 minutes.
The electrode lead is inserted into a vein at the shoulder or the base of the neck. The cardiologist guides the lead into the correct chamber of the heart, checking its position on an X-ray screen and securing it in position with a stitch at your shoulder. The lead is then connected to the pacemaker and the pacemaker is fitted into a small pocket, or space, between the skin and the chest muscle. The amount of electrical energy needed to stimulate the heart to contract is then tested and the pacemaker is adjusted.
Don’t Miss: What Should Resting Heart Rate Be
Prognosis By Ejection Fraction
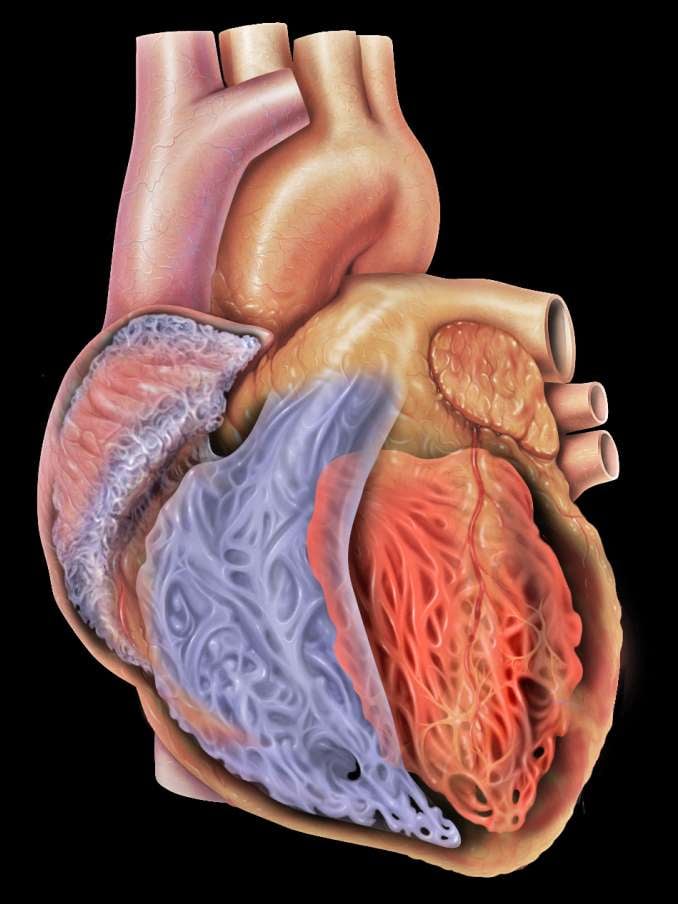
Ejection fraction is a measure of how much blood is pumped out of your heart each time it contracts. A healthy heart has an EF of between about 55 percent to 75 percent.
Some people with CHF have a reduced EF. This means their heart is pumping less blood out to the rest of their body than a healthy heart. Studies have shown that people who have CHF and a reduced EF have a more challenging outlook than people with CHF who do not have a reduced EF.
The exact survival rates varied among studies, but have shown that EF has an impact on prognosis. Your doctor will have the best information about how your ejection fraction can affect your prognosis.
How Does Heart Failure Affect The Quality Of Life And Lifestyle
With the right care and treatment plan, many adults still enjoy life even though heart failure limits their activities. How well you feel depends on:
- How well your heart muscle is working.
- Your symptoms.
- How well you respond to your treatment plan.
- How well you follow your treatment plan.
This includes caring for yourself by:
- Taking your medications.
- Tracking and reporting new or worsening symptoms to your provider.
- Keeping regular follow-up appointments with your healthcare provider.
Because heart failure is a chronic, long-term illness, talk to your doctor and your family about your preferences for medical care. You can complete an advance directive or living will to let everyone involved in your care know what you want. A living will details the treatments you do or dont want to prolong your life. Its a good idea to prepare a living will while you are well in case you arent able to make these decisions at a later time.
A note from Cleveland Clinic
If you have heart failure, you can take steps to improve your heart health. Take your medications as instructed, follow a low-sodium diet, stay active or become physically active, take notice of sudden changes in your weight, live a healthy lifestyle, keep your follow-up appointments and track your symptoms. Talk to your healthcare provider about questions or concerns you have about your medications, lifestyle changes or any other part of your treatment plan.
References
You May Like: Can You Be Awake During Heart Surgery
Stage B Treatment Options
While stage A CHF is managed with lifestyle changes, the treatment plan for stage B typically includes taking medications regularly. People at this stage should still make the same lifestyle changes as those appropriate for stage A. However, your doctor may also prescribe additional treatments such as:
- Angiotensin-converting enzyme inhibitors or angiotensin II receptor blockers, if you arent taking any as part of your stage A treatment plan
- Beta blockers if youve had a heart attack and your EF is 40% or lower, if you arent taking any as part of your stage A treatment plan
- Possible surgery or intervention as a treatment for coronary artery blockage, heart attack, valve disease, or congenital heart disease
Incidence Of Heart Failure After Pacemaker Implantation
- European Heart Journal
You’ve saved your first item
You can find your saved items on your dashboard, in the “saved” tab.
You’ve recommended your first item
Your recommendations help us improve our content suggestions for you and other PracticeUpdate members.
You’ve subscribed to your first topic alert
What does that mean?
You May Like: Do Oxygen Levels Drop During Heart Attack
How Is The Pacemaker Placed
The pacemaker is placed inside the chest by performing very minor surgery. This is not open-heart surgery, so minor anesthesia would suffice to perform the surgery.
The surgery to place the pacemaker in the body can take up to 2-3 hours of time. The pacemaker has batteries that need to be changed after a few years and that again requires a minor surgical performance. The pacemaker can be physically examined at it is placed not much beneath the skin surface.
Key Points To Remember
- A pacemaker for heart failure, also called cardiac resynchronization therapy or CRT, can help you feel better so you can do your daily activities.
- A pacemaker can slow down the progression of heart failure. It may help keep you out of the hospital and help you live longer.
- If you get a pacemaker, you still need to take medicines for heart failure. You’ll also need to follow a healthy lifestyle to help treat heart failure. This includes eating healthy foods that are low in salt, and not smoking.
- Heart experts have guidelines about who might benefit from a pacemaker. Talk to your doctor about the reasons that you might want one. For example, a pacemaker may help you if your heart’s ventricles don’t pump at the same time.
- A pacemaker sends electrical pulses to your heart to help it work better. You can’t feel the pulses.
- There can be problems from having a pacemaker placed in your chest. The wires that connect the pacemaker to your heart can move from the spot where they were placed. You could get an infection where the pacemaker was placed. Or the pacemaker or leads might not work.
How does the pacemaker work?
When you have heart failure, the lower chambers of your heart aren’t able to pump as much blood as your body needs. Sometimes, the ventricles also don’t pump at the same time.
How is the pacemaker placed?
It can take about 2 to 3 hours to place the pacemaker.
You may be able to see a little bump under the skin where the pacemaker is placed.
Problems include:
Recommended Reading: What Does Heart Rate Measure
What Does It Do
A pacemaker monitors your heart rate and sends small and painless electrical impulses to the right ventricle of your heart to start each heartbeat only when needed. You may need a pacemaker if your heart beats too slowly and it cannot be controlled by medication.
Pacemakers today are small metal devices, about the size of a small pocket watch, containing a computer and battery and up to three flexible electrode leads . They are generally not visible, and apart from an insertion scar, which heals in time, they will usually become unnoticeable with time.
How Is Heart Failure Treated
Your treatment will depend on the type of heart failure you have and, in part, what caused it. Medications and lifestyle behaviors are part of every treatment plan. Your healthcare provider will talk to you about the best treatment plan for you. Treatment is the same, regardless of gender.
As heart failure gets worse, your heart muscle pumps less blood to your organs, and you move toward the next stage of heart failure. Since you cant move backward through the heart failure stages, the goal of treatment is to keep you from moving forward through the stages or to slow down the progression of your heart failure.
Stage A treatment
The usual treatment plan for people with Stage A heart failure includes:
- Regular exercise, being active, walking every day.
- Stopping the use of tobacco products.
- Treatment for high blood pressure .
- Treatment for high cholesterol.
- Not drinking alcohol or using recreational drugs.
- Angiotensin-converting enzyme inhibitor or an angiotensin II receptor blocker if you have coronary artery disease, diabetes, high blood pressure, or other vascular or cardiac conditions.
- Beta-blocker if you have high blood pressure.
Stage B treatment
The usual treatment plan for people with Stage B heart failure includes:
Stage C treatment
The usual treatment plan for people with Stage C HF-rEF includes:
If the treatment causes your symptoms to get better or stop, you still need to continue treatment to slow the progression to Stage D.
Stage D treatment
Recommended Reading: What Is A Normal Resting Heart Rate For A 50 Year Old Woman
Pacemakers Restore Proper Heart Rhythm
If the heart doesnt beat at the proper rate typically 60 to 100 beats per minute blood is not pumped properly throughout the body.
A pacemaker is a small, battery-operated device that is implanted under the skin near the heart to help regulate the heartbeat.
About half the size of a deck of cards, a pacemaker mimics the hearts natural pacemaker, which sends electrical impulses through the cardiac muscle to the heart chambers. These electrical signals make the chambers contract normally and pump blood effectively to the body.
UT Southwestern is recognized as one of the nations leading heart disease treatment centers, with faculty in accredited, advanced cardiothoracic surgery and clinical cardiac electrophysiology training programs.
UT Southwestern is also home to a dedicated Cardiac Rehabilitation Program. Cardiac rehabilitation is a critical component of recovery and can prevent future heart disease.
Central Venous Catheter Placement In Icd Patients
Pacemaker or implantable cardioverter-defibrillator leads placed in the venous system often have surrounding thrombosis, with 20% of patients having complete occlusion at 2 years. If a metal guidewire contacts the lead system during central line placement, there may be enough noisy artifact to trigger an inappropriate shock.
Consideration should be given to either avoid a metal guidewire or deactivate the ICD during central line placement. Although the contralateral subclavian or internal jugular vein can be cannulated with care, femoral vein access is a much safer option.
Don’t Miss: How Long Can You Have Angina Before A Heart Attack
Congestive Heart Failure Drugs
There are several medications that can be used to treat CHF, including ACE inhibitors, beta-blockers, and more.
ACE inhibitors
Angiotensin-converting enzyme inhibitors open up narrowed blood vessels to improve blood flow. Vasodilators are another option if you cant tolerate ACE inhibitors.
You may be prescribed one of the following:
voluntary recall of 5 lots of the drug Accupril due to the presence of nitrosamine. Nitrosamine, a known carcinogen with the potential to cause cancer, was found to exist in the drug at levels greater than the Acceptable Daily Intake as determined by the FDA. This recall is specific only to a handful of lot numbers and does not affect all Accupril tablets made by Pfizer. If you take Accupril tablets, talk with your pharmacist or doctor and they will help you determine if your medication has been impacted by the recall.
ACE inhibitors shouldnt be taken with the following medications without consulting a doctor, because they may cause an adverse reaction:
- Potassium-sparing diuretics and potassium supplements. These diuretics can cause potassium buildup in the blood, which may lead to abnormal heart rhythms. Examples include: riamterene , eplerenone , and spironolactone .
- Nonsteroidal anti-inflammatory drugs .NSAIDs such as ibuprofen, aspirin, and naproxen, can cause sodium and water retention. This may reduce the ACE inhibitors effect on your blood pressure.
Beta-blockers
This may be achieved with:
Diuretics
Your doctor may recommend:
Study: Pacemakers Can Cause Heart Failure
People with the most common pacemaker types are more likely than similar people without pacemakers to die from or be hospitalized for gradual heart failure , sometimes within six months, according to a large study confirming doctors’ belief the life-saving devices actually harm some patients.
Experts say the tens of thousands of patients with pacemakers should not panic. They should have the pacemaker checked every several months, contact the doctor if heart failure symptoms such as shortness of breath and fatigue develop, and possibly have the pacemaker’s timing adjusted.
For some patients, replacing the pacemaker with a new type designed to prevent damaging strain on the heart’s key pumping chamber could prevent heart failure, said Dr. Michael Sweeney, director of heart devices implantation at Brigham and Women’s Hospital in Boston.
“The way we’ve practiced cardiac pacing for the last three decades must be abandoned,” said Sweeney, who was not involved in the study.
About 175,000 pacemakers are implanted in this country each year.
Sweeney said about 90 percent stimulate one or two of the heart’s right chambers to contract when beating slows down, but don’t allow the four chambers to beat in the same order as a healthy heart. That out-of-sync beating puts extra stress on the heart’s main pumping chamber, the left ventricle, and in some patients causes congestive heart failure, in which the heart gradually stops pumping effectively.
Don’t Miss: Which Blood Vessels Carry Blood Away From The Heart
Factors Associated With Heart Failure Among Patients With Pacemaker
Factors associated with risk of HF among PM patients are presented in Figure . With increasing age, the risk of HF increased among patients with PM. Furthermore, increased risk of HF was observed among men , patients with CKD , and prior history of MI .
Forest plot showing the factors associated with risk of heart failure among patients with right ventricular pacing.
‘bionic’ Pacemaker Reverses Heart Failure
- Date:
- University of Auckland
- Summary:
- A revolutionary pacemaker that re-establishes the heart’s naturally irregular beat is set to be trialled in New Zealand heart patients this year.
A revolutionary pacemaker that re-establishes the heart’s naturally irregular beat is set to be trialled in New Zealand heart patients this year, following successful animal trials. “Currently, all pacemakers pace the heart metronomically, which means a very steady, even pace. But when you record heart rate in a healthy individual, you see it is constantly on the move,” says Professor Julian Paton, a lead researcher and director of Manaaki Manawa, the Centre for Heart Research at the University of Auckland.
Manaaki Manawa has led the research and the results have just been published in leading journal Basic Research in Cardiology.
“If you analyse the frequencies within your heart rate, you find the heart rate is coupled to your breathing. It goes up on inspiration, and it goes down on expiration, and that is a natural phenomenon in all animals and humans. And we’re talking about very ancient animals that were on the planet 430 million years ago.”
Twelve years ago, Paton was a member of a group of scientists who decided to investigate the function of this variability. They made a mathematical model that predicted it saved energy. That made them question why a metronomic heartbeat was used in heart-failure patients who lacked energy. They asked, “Why aren’t we pacing them with this variability?”
Don’t Miss: How To Figure Out Resting Heart Rate
What To Expect After Pacemaker Surgery
You will be admitted to the hospital overnight for the pacemaker implantation. The nurses will monitor your heart rate and rhythm. The morning after your implant, you will have a chest X-ray to ensure the leads and pacemaker are in the proper position.
You will be shown how to care for your wound. Keep your wound clean and dry. After 5 days, you may take a shower. Look at your wound every day to make sure it is healing. Your pacemaker settings will be checked before you leave the hospital.
You will receive a temporary ID card that tells you:
- The type of pacemaker and leads you have
- The date of the pacemaker implant
- The name of the doctor who implanted the pacemaker
Within 3 months, you will receive a permanent card from the pacemaker company. CARRY THIS CARD WITH YOU AT ALL TIMES in case you need medical attention at another hospital.
Restrictions after pacemaker surgery
- Do not lift objects that weigh more than 10 pounds.
- Do not hold your arms above shoulder level for 3 weeks.
- Avoid activities that require pushing or pulling heavy objects, such as shoveling the snow or mowing the lawn.
- Stop any activity before you become overtired.
- For 6 weeks after the procedure, avoid golfing, tennis, and swimming.
- Try to walk as much as possible for exercise.
- Ask your doctor when you can resume more strenuous activities.
- Your doctor will tell you when you can go back to work, usually within a week after you go home. If you can, ease back to your regular work schedule.
