Aha/acc/hfsa Heart Failure Guideline: Key Perspectives
- Heidenreich PA, Bozkurt B, Aguilar D, et al.
- Citation:
- 2022 AHA/ACC/HFSA Guideline for the Management of Heart Failure: A Report of the American College of Cardiology/American Heart Association Joint Committee on Clinical Practice Guidelines. J Am Coll Cardiol 2022 Apr 1:.
The following are key perspectives from the 2022 American Heart Association /American College of Cardiology /Heart Failure Society of America Guideline for the Management of Heart Failure:
Heart Failure With Reduced Ejection Fraction: Guideline
JACC Review Topic Of The Week: Counterpoint
Healing, Papa would tell me,
is not a science
Although side effects of these drugs are reported in clinical trials to be minimal, the modern consumer has ready access to Internet sites, including the FDAs Web site , which present a less sanguine picture: urosepsis and ketoacidosis are listed as important risks these drugs all carry a warning that they should be held for 3 to 4 days before surgery to reduce risk of ketoacidosis. Canagliflozin had a black box warning for lower extremity amputations removed in 2020 due to new data showing reductions in cardio-renal risks that the FDA felt balanced the relatively low amputation risk, but the amputation warnings persist in the drug information insert. Other potential interactions with antihypertensive medications and insulin may cause hypotension and syncope . Sick day dosing changes are pertinent, as discussed in the following.
Sglti Drugs Incorporated Into Guidelines
The findings of the CVOT and guidelines for use of SGLT2is have been reviewed . At least 3 clinical trials using these drugs during hospital admission for acute decompensated heart failure have recently been published . Use of SGLT2is in ADHF, after the patient is stabilized, has been incorporated into the Canadian Cardiovascular Society/Canadian Heart Failure Society guidelines . These guidelines include clinical tips on use of these drugs, and how to adjust dosing during sick days.
Also Check: Prognosis Congestive Heart Failure
Aha/acc/hfsa Guideline For The Management Of Heart Failure
- Guideline-directed medical therapy for heart failure with reduced ejection fraction now includes 4 medication classes which include sodium-glucose cotransporter-2 inhibitors .
- Patients with advanced HF who wish to prolong survival should be referred to a team specialized in HF. A HF specialty team reviews HF management, assesses suitability for advanced HF therapies and uses palliative care including palliative inotropes where consistent with the patients goals of care.
- Recommendations are provided for select patients with heart failure and iron deficiency, anemia, hypertension, sleep disorders, type 2 diabetes, atrial fibrillation, coronary artery disease and malignancy.
Medication Prescription Pattern According To Patients Characteristics
The beta-blocker prescription rate at discharge was 54.8% in all patients and that of RAS inhibitors was 75.0%. With increasing age, the beta-blocker prescription rate decreased , while that of RAS inhibitors remained unchanged .
Subgroup analysis. The HRs of medical therapy compared with no GDMT for all-cause mortality in subgroups were calculated using multivariate Cox regression analysis. The forest plots demonstrate the HRs of GDMT versus no GDMT from the results. There was no significant interaction between the treatment strategy and diverse subgroups, and GDMT was associated with lower morality across subgroups. *The p for interaction indicates whether treatment strategy interacts with the subgrouping variable. It was calculated from multivariable Cox regression analysis that included the variables for treatment strategy, subgrouping variables, interaction term of the treatment strategy-by-subgrouping variable, sex, hypertension, diabetes, atrial fibrillation and prescription of mineralocorticoid receptor antagonists, digitalis and diuretics. CKD, chronic kidney disease COPD, chronic obstructive pulmonary disease HF, heart failure GDMT, guideline-directed medical therapy RAS, reninangiotensin system.
Don’t Miss: Dogs In Heart Failure
Early Clinical Benefits Following Initiation Of Sglt2i Versus Attention To Comorbid Problems
Rao et al claim that not prescribing SGLT2i to an eligible patient at discharge exposes the patient to a statistically and clinically significant excess risk for death and readmission in the first days to weeks postdischarge. This may be statistically true, but practically speaking, in a typical elderly patient with heart failure, comorbidities may matter more: about 70% of 30-day readmission were for nonheart failure causes, and the median time to readmission was 12 days. Reduction of readmission will need to focus on common comorbid conditions related to age and frailty .
Impact Of Usage Of Gdmt
Clinical improvement was reflected as there was statistically significant improvement in EF from 28.12 during first month to 38.59 by the end of twelfth month in patients managed in HF clinic while there was no significant improvement in EF of patients in other general cardiology OPD . Moreover, at the end of 1year, there was significant difference in the number of events of rehospitalisation and mortality . All these might be attributed to the increased usage and adherence to the guideline in the patients treated in HF clinic.
You May Like: Survival Rate Of Heart Attack By Age
Redefining Patients With Hf: Therapeutic Implications
Until now, we categorized HF patients according to left ventricular ejection fraction : reduced , mid-range , and preserved . The rationale was based on the therapeutic benefits available at the time only for LVEF < 40%. In the new ESC guidelines, this definition evolved, highlighting that therapies beneficial in HFrEF can also be effective in patients with LVEF ranging between 40% and 50%. From now on, we should therefore change our perception of HF patients with LVEF from 40% to 50%, replace the term mid-range with mildly reduced LVEF , and offer them HFrEF therapies.
No treatment has convincingly been shown to improve the prognosis of HFpEF because it includes a more heterogeneous group of patients. For instance, HFpEF with supernormal LVEF may often be due to amyloidosis or hypertrophic cardiomyopathy . Hopefully, specifically designed randomized studies will lead, in the future, to successfully characterize and approach untreatable phenotypes of HFpEF.
Gdmt And Risk Of Death With Primary Prevention Icds
- Dhande M, Rangavajla G, Canterbury A, et al.
- Citation:
Quick Takes
- In patients with HFrEF receiving primary prevention ICDs, incremental addition of heart failure guideline-directed medical therapy is independently associated with lower rates of all-cause mortality.
- These findings were consistent when stratifying outcomes by type of device and cause of cardiomyopathy .
- Future studies examining benefit of primary prevention ICDs in the current era of HF GDMT should be considered.
You May Like: Heart Bypass Surgery Recovery
Drug Prices And Major Side Effects Of Gdmt
Rao et al assert that Challenges with implementation exist for both newer and older generic mediations , strongly suggesting that drug prices are not the predominant explanation for widespread medication underuse. However, patients feel the cost when their medical insurance does not cover a medication or places obstacles in the form of request for prior authorization also, when they have not met a deductible, or when they are in the dreaded donut hole and must pay for medications out-of-pocket.
Recently, cost sensitivity to newer medications was illustrated by an e-mail to me from a long-time patient, who informed me that he found himself in the Medicare Part D donut hole and the cost of his 90-day supply of empagliflozin had tripled. The patient further noted that, unless he was prescribed expensive medications by year end, he would not be able to emerge from the donut hole and the cost of his current medications would become prohibitive. MRAs, irrespective of cost, must be used with caution, especially in elderly frail patients with heart failure. After the publication of RALES , rates of hospitalization for hyperkalemia increased .
Data Collection And Analysis
Patient data relevant to the study was obtained from the electronic medical record during three time points, i.e., first month, sixth month, and twelfth month after the first visit, and the collected data were then evaluated between the study groups to assess the usage of GDMT. Attainment of evidence-based target doses of disease-modifying drugs and time to reach target dose were also evaluated. The patients were categorized to four groups based on the percentage of target dose achieved as group 1 , group 2 , group 3 , and group 4 . Data storage and analysis were performed using Microsoft Excel 2010 and SPSS Version 24. For the comparison of continuous variable, we used independent sample t test and paired t test, and the categorical variables were compared using 2-likelihood ratio test. All the p values were two-tailed, and a significance level of 5% was used.
Also Check: All About Heart Attack
Study Variables And Definition
HFrEF was defined as a left ventricular ejection fraction of 40%. The patients were classified into groups according to the medication prescribed at discharge: the GDMT group , beta-blockers only group, RAS inhibitors only group and no GDMT group . Chronic kidney disease was defined as a glomerular filtration rate of < 60mL/min/1.73m2, and chronic obstructive pulmonary disease was defined as a self-reported or physician-confirmed diagnosis of chronic bronchitis, emphysema or both. The primary outcome was 3-year postdischarge all-cause mortality from index admission.
Heart Failure Usually Is A Chronic Long
At AstraZeneca, we are dedicated to elevating patient voices and experiences, advocating for improvements in the management of HF care.
I wish I wouldve known about heart disease beforehand. Its not something people talk about and its the number one killer among women.
Erinpatient living with HF
Read Also: Is Your Pulse And Heart Rate The Same
Prescription Of Gdmt In Elderly Patients
The prescription rate of GDMT was 50% in patients aged 6569 years and 30% in those aged 85 years. The decline can be mainly attributed to a decreasing beta-blocker prescription rate. Hamaguchi et al reported that the prescription rate of beta-blockers was 48% in HFrEF patients aged 80 years and that GDMT was applied only in 38% of these patients. In this study, the beta-blocker prescription rate was 55% in all patients and 46% in patients aged 80 years. Beta-blockers in very elderly patients may be withheld due to the potential side effects and uncertainty with regard to the benefits for this high-risk group. In addition, 13% of patients had COPD, which was associated with a 30% reduced prescription rate of beta-blockers but not of RAS inhibitors. Accordingly, COPD was associated with a 33% reduced prescription rate of GDMT. This finding reflects the possible side effect of beta-blockers, as non-selective beta-blockers may cause bronchoconstriction in patients with COPD. However, given that multiple studies have shown that beta-1 selective beta-blockers can be used safely in patients with asthma and COPD, beta-1 selective drugs should be considered for patients with COPD.
Funding Support And Author Disclosures
The authors have reported that they have no relationships relevant to the contents of this paper to disclose.
-
McDonagh T.A., Metra M., Adamo M., et al.”2021 ESC guidelines for the diagnosis and treatment of acute and chronic heart failure: developed by the Task Force for the diagnosis and treatment of acute and chronic heart failure of the European Society of Cardiology with the special contribution of the Heart Failure Association of the ESC”. Eur Heart J2021 42:3599-3726.
You May Like: Why Is My Heart Palpitating
Gdmt And Outcomes In Elderly Patients With Hf
Large clinical trials have shown the efficacy of GDMT in patients with HFrEF. However, the patients enrolled in such clinical trials were younger and had fewer comorbidities than real-world elderly patients. Moreover, data from clinical trials supporting the use of GDMT in elderly patients are scarce. The Study of the Effects of Nebivolol Intervention on Outcomes and Rehospitalisation in Seniors with Heart Failure study, which included 2128 patients aged 70 years with a history of HF, is considered the representative study conducted in elderly patients with HF. It showed that nebivolol reduced the composite of all-cause mortality and rehospitalisation for HF but did not reduce all-cause mortality.
Study Design And Participants
The study was approved by the Institutional Review Board at a university hospital. The need for informed consent was waived because of the retrospective nature of the study using coded and anonymized data obtained from routine care. The study was conducted in compliance with the ethical standards of the responsible institution on human subjects.
We conducted a retrospective observational study using data from patients with HFrEF managed at our GDMT Optimization Clinic in Cleveland, Ohio, USA. All patients who carried the diagnosis of HFrEF were identified in the study period from January 2017 to December 2019 and were screened for inclusion.
Inclusion criteria were age 18 years and having a diagnosis of heart failure and a left ventricular ejection fraction of 40% by echocardiography performed within 12 months. Patients were excluded if they only had one follow-up visit to the GDMT Optimization Clinic.
Variables were obtained by chart review from electronic medical records. For all patients, we collected the following data: age, gender, height, weight, diabetes mellites, tobacco use, hypertension, atrial fibrillation, chronic kidney disease , coronary artery disease , and depression. Moreover, baseline labs were also obtained: sodium, potassium, chloride, blood urea nitrogen , and creatinine.
Also Check: What Side Of The Heart Pumps Blood To The Lungs
Strengths And Limitations Of This Study
-
This was a large prospective cohort study that included patients with heart failure with reduced ejection fraction who were aged 65 years or older.
-
We obtained all participants mortality data from medical or national death records.
-
The registry could not capture all comorbidities including functional or cognitive impairments, which is an important prognostic factor for elderly patients.
Why Are Earlier Diagnosis And The Quick Adoption Of Guideline
Learn from Erin, who shares her first-hand experience as a patient living with HF, highlighting how an earlier diagnosis may have been helpful to manage her condition.
We also spoke with Helen Yeh, Vice President, Cardiovascular, Renal & Metabolism , BioPharmaceuticals Medical, AstraZeneca, who underlines the importance of implementing guideline-directed medical therapy as soon as possible, given the severity of this chronic disease and the high risk of death, and the key opportunity to proactively use all latest tools available to diagnose HF.
Professor Giuseppe Rosano, Professor of Cardiology and Consultant Cardiologist at St. George’s Hospital NHS Trust University of London, emphasizes how the 2021 European Society of Cardiology guideline updates have changed the diagnosis and treatment paradigm in acute and chronic HF and some of the barriers that may be hindering the implementation of these updates into practice.
Also Check: What To Do In Case Of A Heart Attack
Whats Next The Challenge Of Optimal Treatment
Because of the availability of so many different drugs with a Class I recommendation, not all patients will be exposed to all of them. The consequences of drugs under treatment or withdrawal are unknown, and no specific strategy aiming at introducing in a given patient the full medical armamentarium has been demonstrated to be preferable.
Any new therapy for HF must be compared with the current optimal standard of care. The definition of optimal treatment and adherence will play a central role in defining the quality of future trials.
It is likely that guideline-directed but patient-tailored treatments will become the next step to follow for all of us, aiming at identifying what is optimal in every specific patient at a given point in time. At least we hope.
Icipants And Cohort Recruitment
The Korean Acute Heart Failure registry is a prospective multicentre registry designed to reflect the real-world clinical data of Korean patients admitted for acute HF. The study design and primary results of the registry have been published elsewhere. Patients hospitalised for acute HF from 10 tertiary university hospitals in Korea were consecutively enrolled from March 2011 to February 2014. Briefly, patients with signs or symptoms of HF and either lung congestion or objective findings of left ventricle systolic dysfunction or structural heart disease were eligible for enrolment in this registry. To minimise selection bias, we tried to enrol all hospitalised patients with acute HF at each hospital. Patients baseline characteristics, clinical presentation, underlying diseases, vital signs, laboratory tests, treatments and outcomes were recorded at admission, and discharge, and during follow-up . The mortality data for patients who were lost to follow-up were obtained from the national insurance data or national death records.
In this study, we included patients with HFrEF who were aged 65 years or older. For patient selection, we serially excluded patients if any of the exclusion criteria was met. Written informed consent was waived by the institutional review board. The study complied with the Declaration of Helsinki.
Read Also: Heart Valve Repair Without Surgery
The New Paradigm In The Treatment Of Hfref
In HFrEF, the new sodium-glucose cotransporter 2 inhibitors dapaglifozin and empaglifozin earned a central role. Despite there being no definitive consensus about how these molecules can provide cardiac benefit, both improve HF outcome, regardless of the presence of diabetes. A recent trial suggests these molecules may be effective even in patients with an LVEF > 40%.
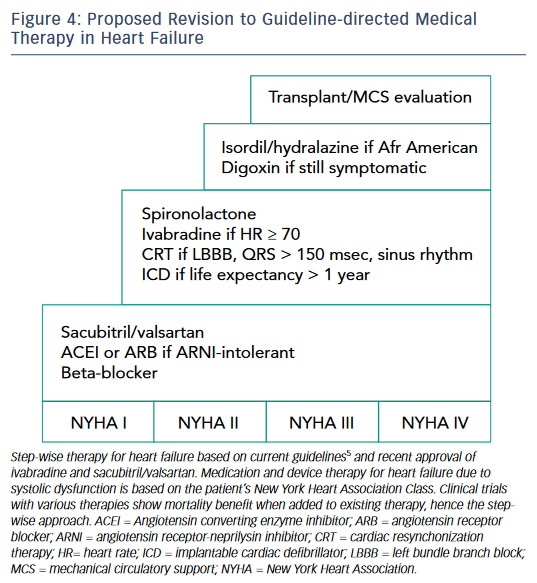
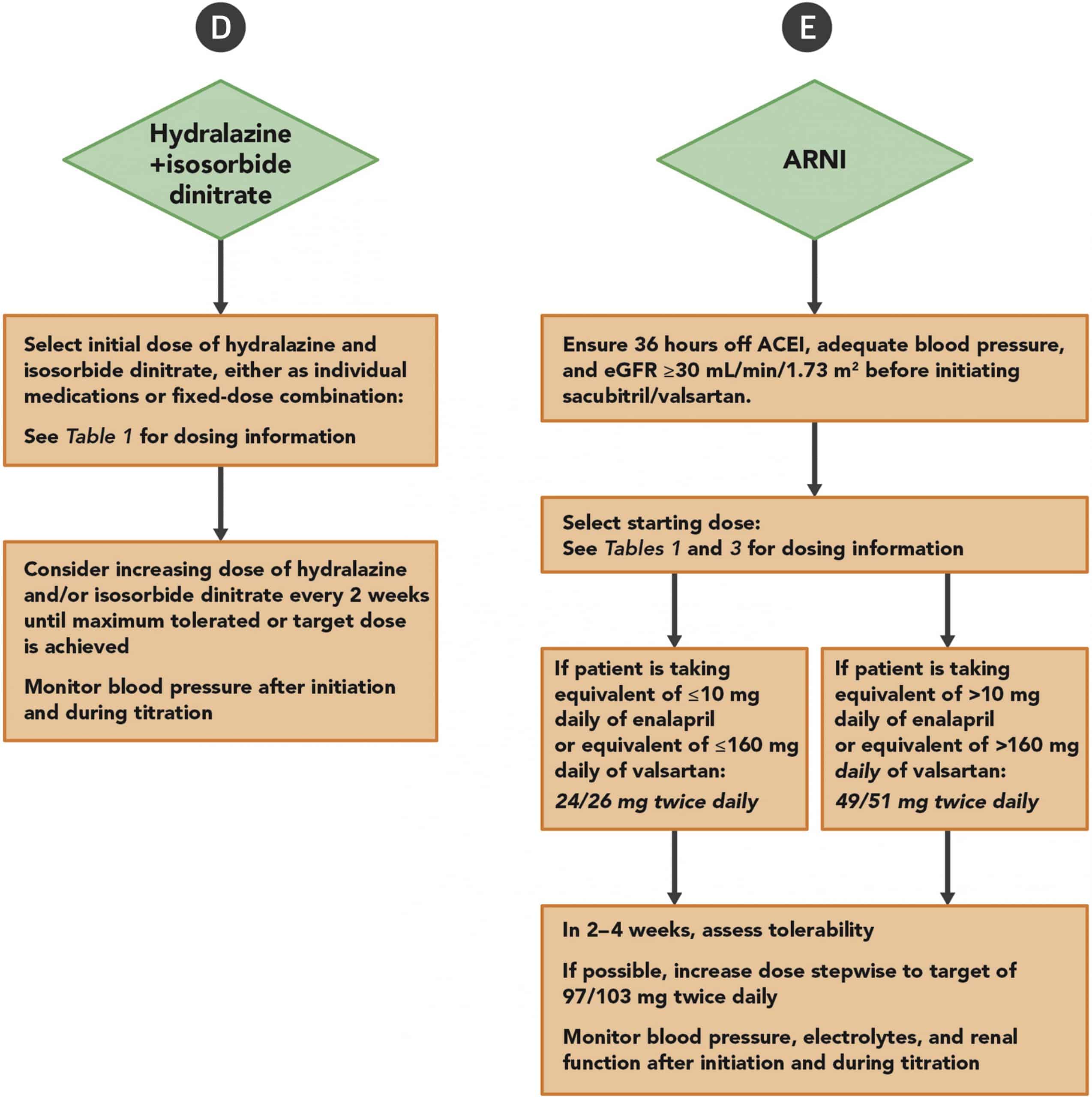
Because we had already 4 different classes of drugs with a Class I recommendation in HFrEF , the issue is now how to manage an increasingly complex armamentarium. The task becomes even more challenging when we need to add on top of disease-modifying drugs symptomatic therapies, such as diuretics. A recent consensus from the American College of Cardiology gives us directions. All patients with a new diagnosis of symptomatic HFrEF should receive a beta-blocker and concomitantly an angiotensin-converting enzyme inhibitor, angiotensin receptor blocker, or angiotensin receptor-neprilysin inhibitor . Each one of these inhibitors can be first-line therapy initiated as soon as possible and should be up-titrated every 2 weeks to the target dose. Patients shifting from ACE inhibitors to ARNIs should receive a starting dose according to the previous ACE inhibitor dose . Notably, in ACE inhibitor-naïve patients, a run-in phase is no longer mandatory, and a direct-to-ARNI approach can be adopted. Choosing this strategy, the most common adverse effects are related to hypotension, while angioedema is infrequent.
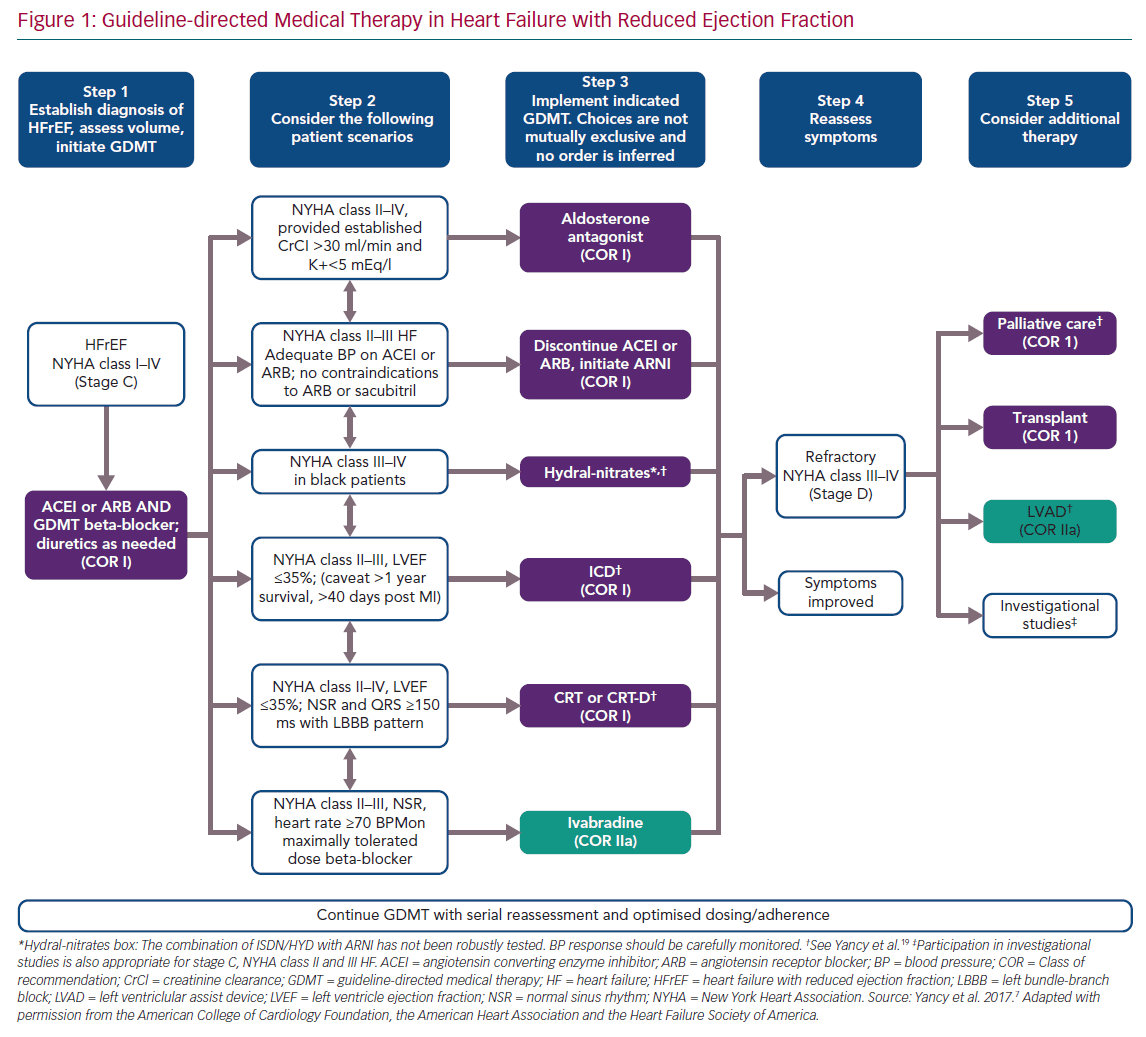
Figure 1
