About The Heart Failure E
The Heart Failure e-Guidelines are based on the 2017 Heart Failure Guidelines Update as published in the CJC and are a comprehensive set of recommendations that integrates and updates the last decade of CCS Heart Failure Guidelines. The CCS gratefully acknowledges the generous volunteer contributions of the many primary and secondary panel members, organizations and individuals involved in the Heart Failure Guidelines Program. Please see for a complete list of authors.
Heart Failure Guidelines Go
Developed for healthcare professionals who care for heart failure patients in the post-acute setting, our new Heart Failure Guidelines Go-To-Guide provides information about the latest, evidence-based heart failure treatment guidelines. The guide also includes resources that can help healthcare professionals in the post-acute setting apply the latest guidelines.
Canadian Cardiovascular Society Consensus Conference Recommendations On Heart Failure Update 200: Prevention Management During Intercurrent Illness Or Acute Decompensation And Use Of Biomarkers
Heart failure is common, yet it is difficult to treat. It presents in many different guises and circumstances in which therapy needs to be individualized. The Canadian Cardiovascular Society published a comprehensive set of recommendations in January 2006 on the diagnosis and management of heart failure, and the present update builds on those core recommendations.
Based on feedback obtained through a national program of heart failure workshops during 2006, several topics were identified as priorities because of the challenges they pose to health care professionals. New evidence-based recommendations were developed using the structured approach for the review and assessment of evidence adopted and previously described by the Society. Specific recommendations and practical tips were written for the prevention of heart failure, the management of heart failure during intercurrent illness, the treatment of acute heart failure, and the current and future roles of biomarkers in heart failure care.
You May Like: Congestive Heart Failure End Of Life
Facts About Heart Failure In The United States
- About 6.2 million adults in the United States have heart failure.1
- In 2018, heart failure was mentioned on 379,800 death certificates .1
- Heart failure costs the nation an estimated $30.7 billion in 2012.2 This total includes the cost of health care services, medicines to treat heart failure, and missed days of work.
Treatments For Patients With Heart Failure With Mildly Reduced Ejection Fraction
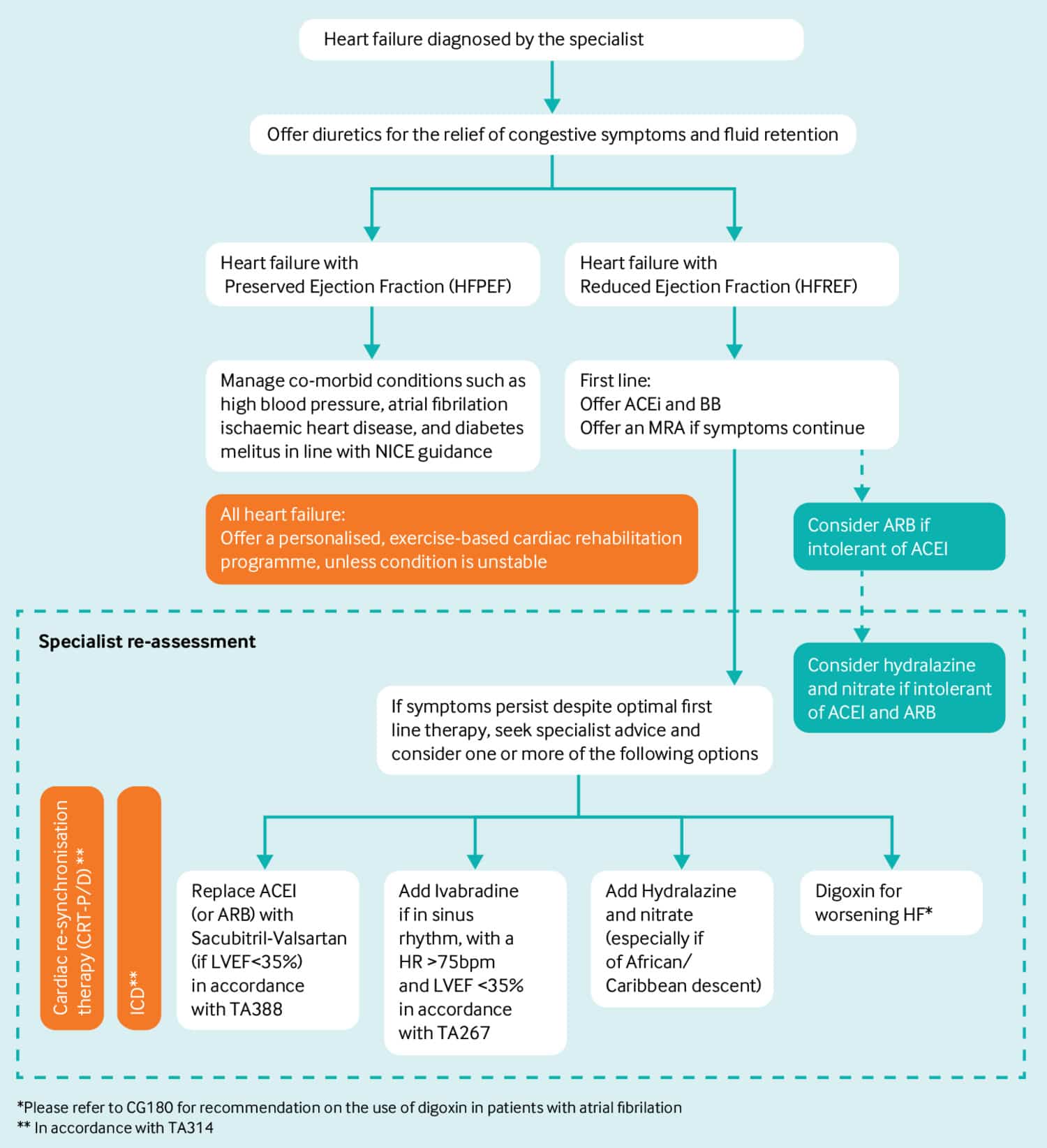
As in other forms of HF, diuretics should be used to control congestion. No substantial prospective RCT has been performed exclusively in patients with HFmrEF . Some data can be gleaned from subgroup analysis of trials in HFpEF, none of which have met their primary endpoint. Although strong recommendations cannot be made about specific therapies at this point in time, we have included a Table of Recommendations to help guide the management of patients in this category.
Pharmacological treatments to be considered in patients with heart failure with mildly reduced ejection fraction
ACE-I=angiotensin-converting enzyme inhibitor ARB=angiotensin-receptor blocker HF=heart failure HFmrEF=heart failure with mildly reduced ejection fraction MRA=mineralocorticoid receptor antagonist NYHA=New York Heart Association.
7.3.1 Angiotensin-converting enzyme inhibitors
There are no specific trials of ACE-I in patients with HFmrEF. Although, the PEP-CHF trial was conducted in patients with HFpEF and included patients with an LVEF > 40%, it did not report outcomes according to LVEF.
However, in patients with HFmrEF, many will also have CAD, hypertension, or post-MI LV systolic dysfunction and will, therefore, already be treated with ACE-I.
Therefore, ACE-I use may be considered in patients with HFmrEF.
7.3.2 Angiotensin receptor II type 1 receptor blockers
7.3.3 Beta-blockers
7.3.4 Mineralocorticoid receptor antagonists
7.3.6 Other drugs
7.3.7 Devices
Also Check: Why Has My Resting Heart Rate Gone Up
Investigations To Determine The Underlying Aetiology Of Chronic Heart Failure
Recommended tests to determine the underlying aetiology of CHF are summarized in Table .
Exercise or pharmacological stress echocardiography may be used for the assessment of inducible ischaemia in those who are considered suitable for coronary revascularization. In patients with HFpEF, valve disease, or unexplained dyspnoea, stress echocardiography might help clarify the diagnosis.
Cardiac magnetic resonance imaging with late gadolinium enhancement , T1 mapping and extracellular volume will identify myocardial fibrosis/scar, which are typically subendocardial for patients with ischaemic heart disease in contrast to the mid-wall scar typical of dilated cardiomyopathy . In addition, CMR allows myocardial characterization in, e.g. myocarditis, amyloidosis, sarcoidosis, Chagas disease, Fabry disease, LV non-compaction CMP, haemochromatosis, and arrhythmogenic cardiomyopathy .,
Computed tomography coronary angiography may be considered in patients with a low to intermediate pre-test probability of CAD, or those with equivocal non-invasive stress tests in order to exclude the diagnosis of CAD.
Single-photon emission CT can also be used to assess myocardial ischaemia and viability, myocardial inflammation or infiltration. Scintigraphy with technetium -labelled bisphosphonate has shown high sensitivity and specificity for imaging cardiac transthyretin amyloid.
Take A Proactive Role
The guidelines are designed to apply to most people in most cases. They give healthcare providers a range of treatment choices. The ultimate decisions rest with the healthcare provider and with you. Remember that you are the most important member of your healthcare team. Asking questions about your treatment is smart and responsible. Its your right to know your healthcare teams goals for you and how clinical guidelines compare with your care plan. It’s important that you understand the approach to your care plan and that you arrive at it together with your healthcare provider.
Online Medical Reviewer:Online Medical Reviewer:Date Last Reviewed:
You May Like: How To Stop A Heart Attack Before It Happens
I Am Presenting In An Oral Live Abstract Or Clinical Case Session
Your presentation should remain short and should focus on the key results of your research. Your presentation timing must not exceed the presentation time indicated on your agreement form.Your presentation slides must be prepared on 16/9 format and we highly recommend the use of the .
Presentation format to be available on-demand on the event platform:
You need to prepare a 5 Slides PowerPoint Presentation and to have ready the corresponding 6 minutes commentary. This timing should be strictly respected.At the time of the upload of your slides, you will record your commentary with an automated assistance service. You will have the option to use your webcam.
Presentation format for the online Abstract session:
To increase the visibility of your research and give you the opportunity to interact with an expert in your topic you are invited to attend an online Abstract or Clinical Case Session during the Live Event . Youll use the same supporting slides than the ones available on demand. You will have 3 minutes to present and a 3 Q& A will follow with the assigned moderators and the audience. Detailed information related to the Online Session will be sent directly to the presenter upon submission of his/her Agreement form.
New Section: The Hospitalized Patient
The 2009 update includes a new section on the evaluation and treatment of heart failure in patients who are hospitalized. Patients may require hospitalization if they develop acute or progressive symptoms of heart failure. Generally there are three clinical profiles for these patients: those who have volume overload those with profound depression of cardiac output and those with signs and symptoms of fluid overload and shock. Patients with heart failure and preserved LVEF are just as likely to be admitted to the hospital as those with heart failure and low LVEF.
Patients are usually admitted to the hospital following a concomitant cardiovascular or cerebrovascular event, and admission often is related to medical or dietary noncompliance. Other common factors that precipitate hospitalization for heart failure include acute myocardial ischemia uncorrected high blood pressure atrial fibrillation and other arrhythmias recent addition of negative inotropic medications pulmonary embolus use of nonsteroidal anti-inflammatory drugs excessive alcohol or illicit drug use endocrine abnormalities and concurrent infections .
Recommended Reading: Nerve Pain After Open-heart Surgery
Secondhand Smoke And Vaping Are Now Official Risk Factors
Quitting smoking has always been an important way to cut your risk of cardiovascular disease, but now the guidelines explicitly include the dangers of secondhand smoke and vaping.
According to the AHA, about a third of U.S. children ages 3-11 are exposed to secondhand smoke or vaping, and both are linked to an increased risk of heart disease and certain kinds of cancer.
In modern America, weve been led to believe that vaping is better than smoking, and thats actually not true, Cho said. Vaping can cause lung problems and cancer, and delivers nicotine, which is highly addictive, she said.
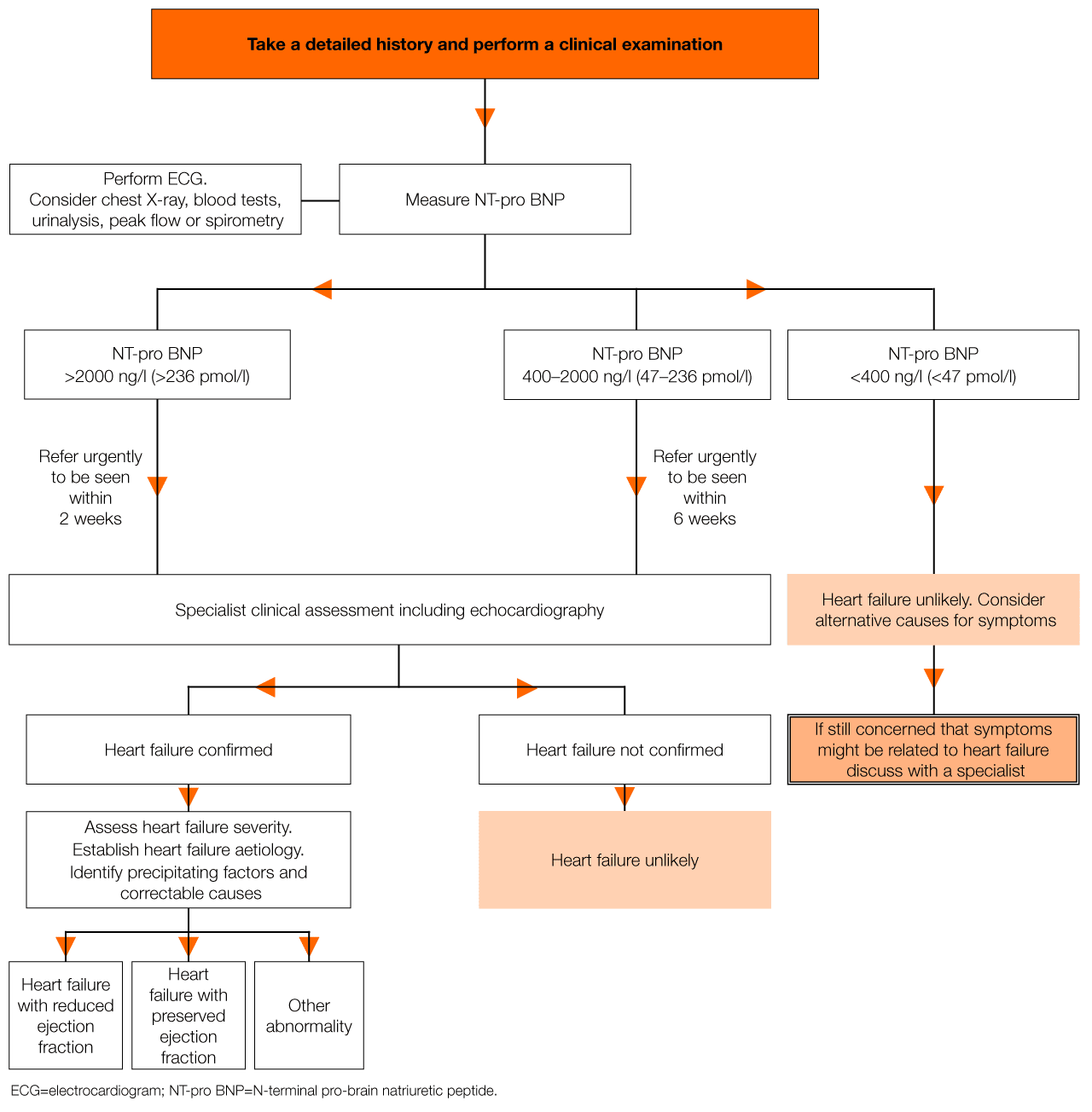
Inpatient Evaluation And Diagnosis
The diagnosis of heart failure in hospitalized patients should be based primarily on signs and symptoms, including volume status, the adequacy of circulatory support or perfusion, and consideration of precipitating factors or comorbidities. Many of the evaluation steps are identical to those used in the initial evaluation of heart failure. For an uncertain diagnosis of heart failure, plasma BNP or NT-proBNP concentrations should be considered in patients being evaluated for dyspnea who have signs and symptoms compatible with heart failure. In patients who have already been diagnosed with heart failure, it is important to understand what has caused the clinical symptoms to worsen.
Acute MI is an important cause of worsening or new-onset heart failure, and criteria for an acute coronary event that might indicate the need for further intervention may be present in up to 20 percent of patients hospitalized for heart failure. However, several other patients may have low levels of detectable troponins that do not meet criteria for an acute ischemic event, but that are typical of chronic heart failure with an acute exacerbation. For patients with newly discovered heart failure, physicians should keep in mind the causative role of coronary artery disease in heart failure and be certain that coronary structure and function are well delineated. Therefore, coronary visualization may be an important step in the evaluation of patients hospitalized with heart failure.
Also Check: How Long Can Heart Attack Symptoms Go On
The Guidelines Also Underscore The Importance Of Other Healthy Lifestyle Habits
Beyond quitting smoking and getting good sleep, the guidelines include things that are proven to help maintain and or improve heart health: exercise, eating well, keeping cardiovascular risk factors in check and more.
It may feel pretty daunting to commit to all of these goals, but you can do so little by little until you create a new routine. Try going for a 21-minute walk a few times a week, for example. Once youre ready, you can up your frequency to every day, which Harvard Health says can cut your risk of heart disease by 30%.
Other ways to start your heart health journey? Make an appointment to check in on your cholesterol and blood pressure or swap in salads for lunch a few days a week.
The American Heart Association encourages everyone to follow these guidelines in addition to those mentioned above:
Honestly, this is not bad news, this is great news … you can do something, youre in control of your heart health, Cho said.
For more help on your journey to better heart health, Cho stressed that youre not alone you can talk to your physician about your goals and find resources via the American Heart Association, the American College of Cardiology or Cleveland Clinic.
The Background To Heart Failure With Preserved Ejection Fraction
This guideline acknowledges the historical changes in nomenclature and the lack of consensus on the optimal LVEF cut-off to define the group of patients with HF without overtly reduced EF. The term preserved was originally proposed in the Candesartan in Heart failure: Assessment of Reduction in Mortality and morbidity Programme to refer to patients with an EF that was not clearly reduced or completely normal. While the current guidelines have designated patients with an LVEF 4149% as HFmrEF, we recognize that there will be debate about what constitutes mildly reduced EF, what these EF cut-offs should be, and whether they should be different for men and women., The EACVI defines systolic dysfunction as being < 52% for males and < 54% for females.
You May Like: What Part Of The Brain Controls Heart Rate
Do You Find It Hard To Follow Your Treatment Plan For Hfref
Often, even the best medical advice for managing heart failure is hard to maintain for many reasons. Medicines may have side effects, like fatigue. The cost and logistics of taking several medicines at different times may be challenging. Not surprisingly, as many as half of people following a treatment plan for HFrEF arent able to take medicines consistently as prescribed so if youre finding it hard, youre not alone.
Unfortunately, not taking medicine as often as needed or at the dose needed can affect your health. So, talk to your doctor to see if there are ways to address the challenges that make it hard to follow your plan.
Options might include
- getting larger quantities of each prescription to minimize trips to the pharmacy
- simplifying the regimen
- using pill boxes and reminders
- choosing generic medicines to lower cost, or getting assistance with copays.
Living well with heart failure depends not only on the available therapies, but on ongoing, open communication with your medical team about how you are feeling, what your goals are, and what challenges youre facing, so that together you can determine the right path forward for you.
About the Author
Amy Leigh Miller, MD, PhD, Contributor
Ccs/chfs Heart Failure Guidelines: Clinical Trial Update On Functional Mitral Regurgitation Sglt2 Inhibitors Arni In Hfpef And Tafamidis In Amyloidosis
In this update, we focus on selected topics of high clinical relevance for health care providers who treat patients with heart failure , on the basis of clinical trials published after 2017. Our objective was to review the evidence, and provide recommendations and practical tips regarding the management of candidates for the following HF therapies: transcatheter mitral valve repair in HF with reduced ejection fraction a novel treatment for transthyretin amyloidosis or transthyretin cardiac amyloidosis angiotensin receptor-neprilysin inhibition in patients with HF and preserved ejection fraction and sodium glucose cotransport inhibitors for the prevention and treatment of HF in patients with and without type 2 diabetes. We emphasize the roles of optimal guideline-directed medical therapy and of multidisciplinary teams when considering transcatheter mitral valve repair, to ensure excellent evaluation and care of those patients.
Also Check: Do Heart Attack Symptoms Come And Go Over Weeks
The 2013 Canadian Cardiovascular Society Heart Failure Management Guidelines Update: Focus On Rehabilitation And Exercise And Surgical Coronary Revascularization
The 2013 Canadian Cardiovascular Society Heart Failure Management Guidelines Update provides focused discussions on the management recommendations on 2 topics: exercise and rehabilitation and surgical coronary revascularization in patients with heart failure. First, all patients with stable New York Heart Association class I-III symptoms should be considered for enrollment in a tailored exercise training program, to improve exercise tolerance and quality of life. Second, selected patients with suitable coronary anatomy should be considered for bypass graft surgery. As in previous updates, the topics were chosen in response to stakeholder feedback. The 2013 Update also includes recommendations, values and preferences, and practical tips to assist the clinicians and health care workers manage their patients with heart failure.
The 2012 Canadian Cardiovascular Society Heart Failure Management Guidelines Update: Focus On Acute And Chronic Heart Failure
The 2012 Canadian Cardiovascular Society Heart Failure Guidelines Update provides management recommendations for acute and chronic HF. In 2006, the Canadian Cardiovascular Society HF Guidelines committee first published an overview of HF management. Since then, significant additions to and changes in many of these recommendations have become apparent. With this in mind and in response to stakeholder feedback, the Guidelines Committee in 2012 has updated the overview of both acute and chronic heart failure diagnosis and management. The 2012 Update also includes recommendations, values and preferences, and practical tips to assist the medical practitioner manage their patients with HF.
Don’t Miss: Can Antihistamines Cause Heart Palpitations
What Is Heart Failure
Heart failure happens when a persons heart is weak and cannot pump blood and oxygen to the rest of the body as well as it should.
According to the Centers for Disease Control and Prevention , heart failure affects 6.2 million American adults.
While there is not a cure for heart failure, it can be managed through medication, lifestyle changes, and other treatments .
The 2011 Canadian Cardiovascular Society Heart Failure Management Guidelines Update: Focus On Sleep Apnea Renal Dysfunction Mechanical Circulatory Support And Palliative Care
The 2011 Canadian Cardiovascular Society Heart Failure Guidelines Focused Update reviews the recently published clinical trials that will potentially impact on management. Also reviewed is the less studied but clinically important area of sleep apnea. Finally, patients with advanced HF represent a group of patients who pose major difficulties to clinicians. Advanced HF therefore is examined from the perspectives of HF complicated by renal failure, the role of palliative care, and the role of mechanical circulatory support . All of these topics are reviewed from a perspective of practical applications. Important new studies have demonstrated in less symptomatic HF patients that cardiac resynchronization therapy will be of benefit. As well, aldosterone receptor antagonists can be used with benefit in less symptomatic HF patients. The important role of palliative care and the need to address end-of-life issues in advanced HF are emphasized. Physicians need to be aware of the possibility of sleep apnea complicating the course of HF and the role of a sleep study for the proper assessment and management of the conditon. Patients with either acute severe or chronic advanced HF with otherwise good life expectancy should be referred to a cardiac centre capable of providing MCS. Furthermore, patients awaiting heart transplantation who deteriorate or are otherwise not likely to survive until a donor organ is found should be referred for MCS.
Also Check: How Do You Calculate Your Resting Heart Rate
