How Are Blood Tests Performed
Blood tests may be performed in a lab or providers office.1-2 They are a typical part of a routine exam. Sometimes blood tests are done before you eat for the day, after an 8-12 hour fast. Samples of blood are drawn by a needle from a vein in the arm into test tubes which are then analyzed by a lab for the levels of specific components.2
Table Of Cutoff Values
Table 2, below, summarizes the evidence-based cutoff values of BNP and NT-proBNP for ruling in and ruling out the diagnosis of heart failure in the dyspneic patient presenting to the emergency department.
Table 2. Evidence-Based BNP and NT-proBNP Cutoff Values for Diagnosing HF
|
Criterion |
|
|
BNP = B-type natriuretic peptide GRF = glomerular filtration rate HF = heart failure LR = likelihood ratio NPV = negative predictive value NT-pro-BNP = N-terminal proBNP PPV = positive predictive value = not specifically defined. * Derived from Breathing Not Properly data . Derived from PRIDE data . Derived from subset of Breathing Not Properly data . |
BNP and NT-proBNP levels are higher in older patients, women, and patients with renal dysfunction or sepsis. Atrial fibrillation has also been associated with increased BNP levels in the absence of acute heart failure. However, BNP levels may be disproportionately lower in patients who are obese due to fat metabolism or who have hypothyroidism or advanced end-stage heart failure . NT-proBNP plasma levels are also lower in obese heart failure patients relative to nonobese patients with heart failure, regardless of whether the etiology is ischemic or nonischaemic.
Physical Exam For Heart Failure
First, your doctor will want to know if you:
- Have other conditions such as diabetes, kidney disease, angina, high blood pressure, or other heart problems
- Drink alcohol, and how much
- Take medications, and which ones
Your doctor will also do a physical exam. They’ll look for signs of heart failure as well as other illnesses that may have weakened your heart.
During your visit, your doctor will:
- Listen to your heart
- Check your blood pressure
Theyâll also look at your appearance while you sit, do mild activity, and lie flat. People with mild or moderate heart failure may appear comfortable at rest, but when active, they often become short of breath. Those with heart failure may be uncomfortable if they lie flat for a few minutes.
Your doctor may check for fluid in your lungs with a stethoscope. People with heart failure may also have neck veins that are larger than normal, swelling of the legs or abdomen, or an enlarged liver.
Don’t Miss: Does High Potassium Cause Heart Attacks
A Blood Test Threshold For Diagnosing Heart Failure In General Practice Is Reviewed
This is a plain English summary of an original research article
The cut-off level for the blood test NTproBNP appears to provide the best balance of detecting true cases while excluding false positives when lowered to 125 pg/ml.
The trial supported by the NIHR included a sample of people presenting to their GP with suspected heart failure. It aimed to see which method was best for identifying those who needed referral: the blood test alone clinical decision rules based on clinical symptoms or the combination of both.
The blood test alone at the 125 pg/ml cut-off correctly identified 94% of people with heart failure but led to 50% of people who did not have heart failure being referred for further investigation. This threshold is lower than the level currently recommended by NICE , which could miss up to one in five people.
Clinical decision rules used alone or in combination with the blood test did not improve detection rates.
However, the lower cut-off would also mean that one in two people without heart failure would be referred for unnecessary expensive tests. A cost-effectiveness analysis is being prepared, which will enable decision-makers to balance the effectiveness of the different approaches.
Liver Size And Hepatojugular Reflux
The key component of the abdominal examination is the evaluation of liver size. Hepatomegaly may occur because of right-sided heart failure and venous congestion.
The hepatojugular reflux can be a useful test in patients with right-sided heart failure. This test should be performed while the patient is lying down with the upper body at a 45-degree angle from the horizontal plane. The patient keeps the mouth open and breathes normally to prevent Valsalva’s maneuver, which can give a false-positive test. Moderate pressure is then applied over the middle of the abdomen for 30 to 60 seconds. Hepatojugular reflux occurs if the height of the neck veins increases by at least 3 cm and the increase is maintained throughout the compression period.18
You May Like: Fitbit Heart Rate Too High
How To Diagnose Heart Failure
This article was medically reviewed by Jonas DeMuro, MD. Dr. DeMuro is a board certified Pediatric Critical Care Surgeon in New York. He received his MD from Stony Brook University School of Medicine in 1996. He completed his fellowship in Surgical Critical Care at North Shore-Long Island Jewish Health System and was a previous American College of Surgeons Fellow.There are 11 references cited in this article, which can be found at the bottom of the page.wikiHow marks an article as reader-approved once it receives enough positive feedback. In this case, 93% of readers who voted found the article helpful, earning it our reader-approved status. This article has been viewed 17,394 times.
Heart failure, or congestive heart failure, is a condition where your heart stops pumping blood like it should. Early detection of heart failure and proper treatment can help you live longer and have an active life. Learn how to diagnose heart failure so you can get the proper treatment and maintain a better quality of life.
What Did This Study Do
The REFER study included 304 adults aged over 55 years who were recruited to the study when they presented with suspected heart failure at 28 UK GP practices. The final number of participants was lower than planned, but is still larger than previous, similar studies.
Clinical assessment, blood tests, electrocardiograph and echocardiograms were carried out within seven days. Three heart specialists independently assessed each case. They were given patient data in three instalments: clinical assessment, ECG and echocardiogram results addition of clinical decision rule data and finally blood levels of NTproBNP .
The accuracy of heart failure diagnosis using the decision rule, NTproBNP level , or combination of the two was compared against a reference standard. In this case, the standard was a diagnosis confirmed by consensus of three experts using agreed standard definitions.
Recommended Reading: How Much Does Open Heart Surgery Cost With Medicare
Risk Factors And Symptoms
Risk factors for cardiomyopathy and heart failure include a family history of coronary artery disease, a previous heart attack, excessive alcohol consumption, drug abuse, and obesity. Certain conditions can also increase risk, including high blood pressure, diabetes, thyroid disorders, a buildup of iron in the heart muscle, and sarcoidosis, which causes inflammation in the bodys organs. Cancer treatments, including radiation and certain types of chemotherapy, may also increase a persons risk.
In its earliest stages, cardiomyopathy and heart failure may not cause noticeable symptoms. However, as the condition progresses, a person may experience fatigue or shortness of breath, especially with physical exertion. They may also have swelling of the legs, feet, and abdomen, which occurs when the body overproduces fluid in response to a reduction in blood pumped from the heart. Other symptoms include heart palpitations or lightheadedness caused by irregular heartbeats, or arrhythmias.
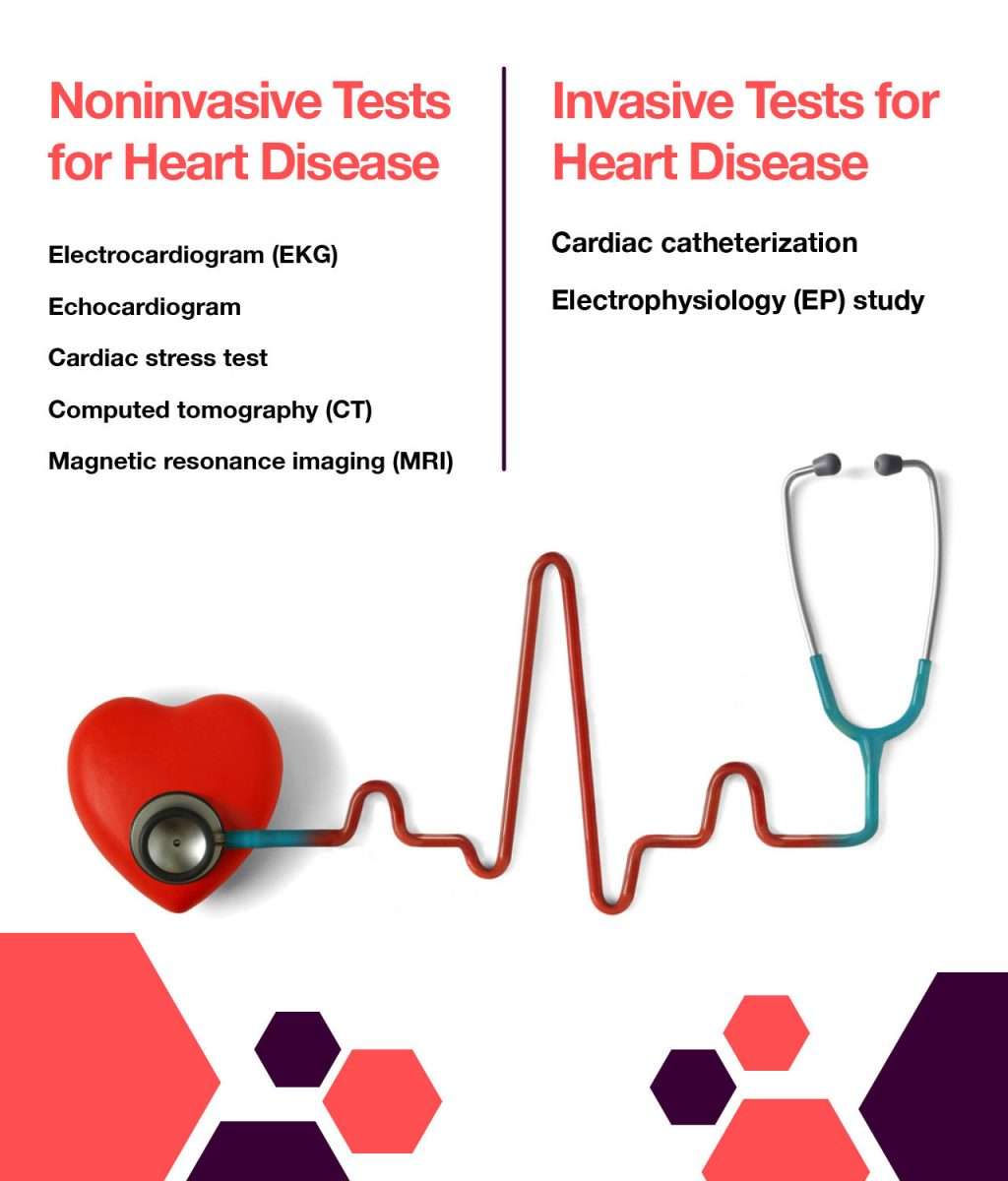
Diagnosing Cardiomyopathy & Heart Failure
NYU Langone specialists are experts at identifying cardiomyopathy and heart failure, a type of heart disease in which the heart fails to pump enough blood to the body. It can be inherited, or it can be caused by another condition, as well as by certain medications or lifestyle habits.
When cardiomyopathy weakens the hearts ability to pump blood, heart failure may occur. Right-sided heart failure happens when the heart cant pump enough blood to the lungs. Left-sided heart failure occurs when the heart cant pump enough blood to the rest of the body. Most of the time, the condition affects both sides of the heart.
Recommended Reading: How To Know If You’re Having A Heart Attack Male
What Is Heart Failure
Heart failure, or congestive heart failure, is a long-term condition that gets worse over time. Although the name sounds like your heart has stopped working, heart failure means your heart isnt able to pump blood as well as it should. When your heart has less pumping power, that can damage your organs and fluid can collect in your lungs.
What Are The Types Of Heart Failure
There are many causes of heart failure, but the condition is generally broken down into these types:
Left-sided heart failure
Heart failure with reduced left ventricular function The lower left chamber of your heart gets bigger and cannot squeeze hard enough to pump the right amount of oxygen-rich blood to the rest of your body.
Heart failure with preserved left ventricular function Your heart contracts and pumps normally, but the bottom chambers of your heart are thicker and stiffer than normal. Because of this, your ventricles can’t relax properly and fill up all the way. Because there’s less blood in your ventricles, your heart pumps out less blood to the rest of your body when it contracts.
Right-sided heart failure
Heart failure can also affect the right side of your heart. Left-sided heart failure is the most common cause of this. Other causes include certain lung problems and issues in other organs.
Recommended Reading: Right Sided Heart Failure Symptoms
Autosomal Dominant Arrhythmogenic Right Ventricular Dysplasia/cardiomyopathy
ARVD/C is characterized by progressive fibrofatty replacement of the myocardium that predisposes to ventricular tachycardia and sudden death in young individuals and athletes. It primarily affects the RV with time, it may also involve the LV. The presentation of disease is highly variable even within families, and affected individuals may not meet the established clinical criteria. The mean age at diagnosis is 31 years .
Genetic testing should be considered in individuals who have a clinical diagnosis of ARVD based on the diagnostic criteria. A case can be made to offer genetic testing to all with a clinical diagnosis of ARVD with a negative family history based on the high rate of reduced penetrance thus far identified with the ARVD genes. Molecular genetic testing is available on a clinical basis for TGFB3, RYR2, TMEM43, DSP, PKP2, DSG2, DSC2, and JUP.
For more information regarding genetic testing and cardiomyopathy, please see HFSA Guideline Approach to Medical Evidence for Genetic Evaluation of Cardiomyopathy, as well as Murphy RT, Starling RC. Genetics and cardiomyopathy: where are we now? Cleve Clin J Med. Jun 2005 72:465-6, 469-70, 472-3 passim.
Identifying The Symptoms Of Heart Failure

Read Also: Can Gas Cause Heart Palpitations
What Causes Heart Failure
Although the risk of heart failure doesnt change as you get older, youre more likely to have heart failure when youre older.
Many medical conditions that damage the heart muscle can cause heart failure. Common conditions include:
- Tobacco and recreational drug use.
- Medications. Some drugs used to fight cancer can lead to heart failure.
What Are The Most Common Symptoms Of Congestive Heart Failure
Swelling is the most common symptom of congestive heart failure. Often, swelling is most apparent in the extremities, especially in the legs and ankles, but it can occur in other parts of the body as well. Fluid collection in and around the lungs can cause shortness of breath , especially during physical activity or when lying down. Other common symptoms of heart failure include fatigue, loss of appetite, and weight gain.
You May Like: Signs Of Heart Attack For Woman
How Is Congestive Heart Failure Treated
Advanced treatment approaches are extending and improving quality-of-life for patients with congestive heart failure. Congestive heart failure is treated and managed through a combination of lifestyle modifications and a wide range of therapies, including medication and interventions, which help the heart to work more effectively and alleviate heart failure symptoms. Pacemakers and ventricular assist devices can make it easier for heart the heart to pump blood and remain in rhythm. For some patients with advanced heart failure, a heart transplant may be an option.
What Do The Left And Right Sides Of The Heart Do
The two sides of your heart work in different ways to pump blood.
- Left side: Receives oxygen-rich blood from your lungs and delivers it to the rest of your body. The oxygen helps organs, muscles and other tissue do their job.
- Right side: Receives oxygen-poor blood from your body and delivers it to your lungs. From there, you release carbon dioxide and take in more oxygen.
Also Check: What Is The Survival Rate Of Open Heart Surgery
The Best Exercises For Heart Failure
Your heart is your bodyâs most important muscle. Like all of the others, it needs exercise. Thatâs true even when you have heart failure.
In most cases, light to moderate exercise isnât going to make your condition worse. In fact, itâs not only safe, itâs the best medicine, says Suzanne Steinbaum, DO, an American Heart Association Go Red for Women volunteer medical expert and cardiologist in New York City.
It slows your heart rate, opens your arteries, and improves the way your heart works, she says. This means less shortness of breath and less time spent in the hospital — and possibly a longer life.
Exercise can help you do the activities you love, Steinbaum adds.
The key is to do it smartly to keep your ticker as strong as it can be. Ask your doctor which activities are safe for you and how much you should do, says Brittany Ferri, MS, OTR/L, an occupational therapist in Rochester, NY.
What Is The Outlook With Heart Failure
With the right care, congestive heart failure wont stop you from doing the things you enjoy. Your prognosis, or outlook for the future, will depend on:
- How well your heart muscle is working.
- How well you respond to your treatment plan.
- How well you follow your treatment plan.
One study says that people with heart failure have a life span 10 years shorter than those who dont have heart failure. Another study showed that the survival rates of people with chronic heart failure were 80% to 90% for one year, but that dropped to 50% to 60% for year five and down to 30% for 10 years.
A different study found that people who had heart failure and were discharged from the hospital had expected life spans ranging from three to 20 years, depending on various factors like age and gender. Its important to look at your specific situation when considering your prognosis.
Read Also: Heart Failure Exacerbation Symptoms
What Are The Symptoms Of Left
Symptoms may be mild at first or you may think it’s a cold or allergy. You might not even notice them. But as heart functioning worsens, you may experience:
- Constant coughing.
- Shortness of breath with walking or bending over.
- Waking up short of breath or unable to lie flat at night.
- Swelling in your ankles, legs or abdomen.
Over time, the heart works harder to do its job. This causes complications that may include:
- Abnormal heart rates and rhythms .
How Does Heart Failure Affect The Quality Of Life And Lifestyle
With the right care and treatment plan, many adults still enjoy life even though heart failure limits their activities. How well you feel depends on:
- How well your heart muscle is working.
- How well you respond to your treatment plan.
- How well you follow your treatment plan.
This includes caring for yourself by:
- Taking your medications.
Read Also: Natural Ways To Reverse Congestive Heart Failure
Systolic Vs Diastolic Dysfunction
As many as 40 percent of patients with clinical heart failure have diastolic dysfunction with normal systolic function.32 In addition, many patients with systolic dysfunction have elements of diastolic dysfunction. With systolic dysfunction, the pumping ability of the ventricle is impaired. With diastolic dysfunction, ventricular filling is defective.
Ventricular diastolic function depends on the pressure-to-volume relationship in the left ventricle. Decreased compliance of the left ventricular wall leads to a higher pressure for a given diastolic volume. The end result is impaired ventricular filling, inappropriately elevated left atrial and pulmonary venous pressure, and decreased ability to increase stoke volume. These dysfunctions lead to the clinical syndrome of heart failure.
Findings suggestive of diastolic dysfunction on the two-dimensional echocardiogram are left ventricular hypertrophy, a dilated left atrium, a normal or nearly normal ejection fraction and reversal of the normal pattern of flow velocity across the mitral valve .
The rightsholder did not grant rights to reproduce this item in electronic media. For the missing item, see the original print version of this publication.
