Patient Characteristics According To Heart Failure With Preserved Ejection Fraction Descriptive Models
Approximately one quarter of the patients fulfilled at least one of our four descriptive models of HFpEF: 1st descriptive model, 107 patients 2nd, 82 3rd, 61 and 4th, 69 .1). Thus, the same patients could be part of several descriptive models. The remaining 292 patients did not fulfil the FCHF but could have single FC. The baseline variables, according to the presence or absence of the four descriptive models, are shown in Table1.1. Patients in descriptive model 0 were younger and had lower NYHA class, NTproBNP, LAVI, and E/e´ compared with patients with FCHF . Minnesota Living with Heart Failure Questionnaire showed better quality of life in descriptive model 0 compared with descriptive model 1, median 26 and 32, respectively, P < 0.001, Table11.
Do Patients With Acute Heart Failure And Preserved Ejection Fraction Have Heart Failure At Follow
- CAMILLA HAGECorrespondenceReprint requests: Camilla Hage, RN, PhD, Heart and Vascular Theme, Heart failure and GUCH, Karolinska University Hospital, SE-171 76 Stockholm, Sweden. Tel: +46 8 517 792 82 Fax: +46 8 34 49 64.Karolinska Institutet, Department of Medicine, Cardiology unit, Stockholm, SwedenKarolinska University Hospital, Heart and Vascular Theme, Stockholm, Sweden
- Karolinska Institutet, Department of Medicine, Cardiology unit, Stockholm, SwedenSt Görans Hospital, Department of Cardiology, Stockholm, Sweden
- Karolinska Institutet, Department of Medicine, Cardiology unit, Stockholm, SwedenKarolinska University Hospital, Heart and Vascular Theme, Stockholm, Sweden
Congestive Heart Failure: The Framingham Criteria
Until the 1960s, there were no standardized criteria for adjudicating CHF inclinical studies. McKee and colleagues recognized the need for such criteria tofacilitate efforts to document the risk factors and natural history of CHF. As theywrote, if preventive and prophylactic programs are to be developed, theidentification of factors that predispose and influence the course of the diseasebecome important.1
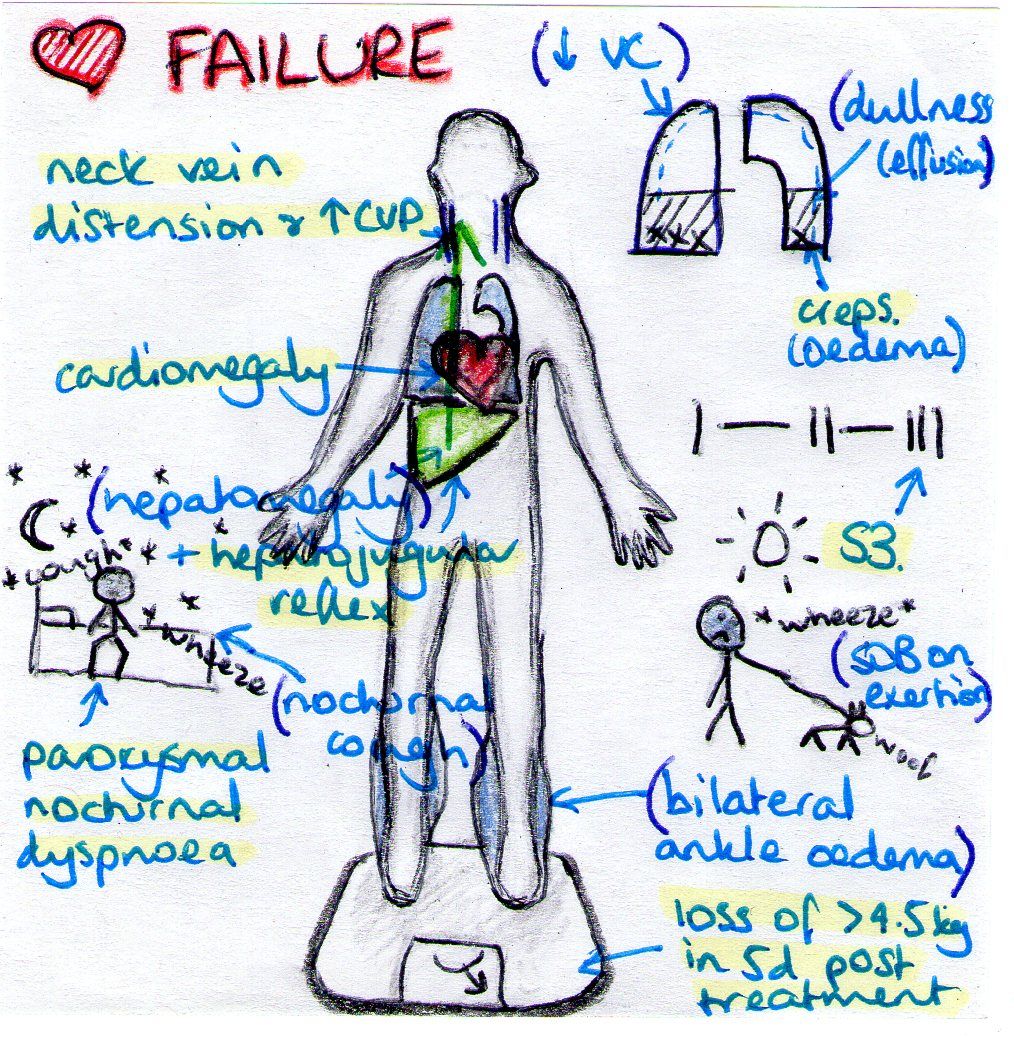
The criteria they proposed are shown in Table1. Included in the list were physician-assessment of neck-veindistension, rales, S3 gallop, venous pressure > 16cm of water, hepatojugularreflux, and weight loss of 4.5 kg in 5 days due to diuretic therapy . Minor criteria were ankle edema, night cough, dyspnea on exertion,hepatomegaly, tachycardia and weight loss. Definite CHF wasdefined as having at least two major criteria, or one major criterion and two minorcriteria, as long as the minor criteria could not be attributed to any othercondition.
Recommended Reading: Is Heart Rate The Same As Blood Pressure
Systolic And Diastolic Failure
Systolic and diastolic heart failure each result in a decrease in stroke volume. This leads to activation of peripheral and central baroreflexes and chemoreflexes that are capable of eliciting marked increases in sympathetic nerve traffic.
Although there are commonalities in the neurohormonal responses to decreased stroke volume, the neurohormone-mediated events that follow have been most clearly elucidated for individuals with systolic heart failure. The ensuing elevation in plasma norepinephrine directly correlates with the degree of cardiac dysfunction and has significant prognostic implications. Norepinephrine, while directly toxic to cardiac myocytes, is also responsible for a variety of signal-transduction abnormalities, such as downregulation of beta1-adrenergic receptors, uncoupling of beta2-adrenergic receptors, and increased activity of inhibitory G-protein. Changes in beta1-adrenergic receptors result in overexpression and promote myocardial hypertrophy.
Precipitating Causes Of Heart Failure
A previously stable, compensated patient may develop heart failure that is clinically apparent for the first time when the intrinsic process has advanced to a critical point, such as with further narrowing of a stenotic aortic valve or mitral valve. Alternatively, decompensation may occur as a result of the failure or exhaustion of the compensatory mechanisms but without any change in the load on the heart in patients with persistent, severe pressure or volume overload. In particular, consider whether the patient has underlying coronary artery disease or valvular heart disease.
The most common cause of decompensation in a previously compensated patient with heart failure is inappropriate reduction in the intensity of treatment, such as dietary sodium restriction, physical activity reduction, or drug regimen reduction. Uncontrolled hypertension is the second most common cause of decompensation, followed closely by cardiac arrhythmias . Arrhythmias, particularly ventricular arrhythmias, can be life threatening. Also, patients with one form of underlying heart disease that may be well compensated can develop heart failure when a second form of heart disease ensues. For example, a patient with chronic hypertension and asymptomatic LV hypertrophy may be asymptomatic until an MI develops and precipitates heart failure.
- Profound anemia
- Nutritional deficiencies
You May Like: Congestive Heart Failure End Of Life
Relevance To Lower And Middle Income Countries
Over the past decades, global socioeconomic development has resulted in anepidemiological transition, with shifts in the leading causes anddeath. As of 2008, 4 out of every 5 deaths globally from cardiovascular diseaseoccurred in developing nations.14A paucity of data exists on the global prevalence of heart failure, although someestimate that more than 23 million people worldwide are living with thecondition.15 A limitationof the original Framingham cohort is that the volunteers were almost entirelyCaucasian, although the new Omni cohorts of the Framingham study reflect a morediverse US population.
Nevertheless, multiple observations from the study of McKee and colleaguesare relevant to the global problem of heart failure. As in the U.S., hypertensionhas been identified as a key risk factor for heart failure in the other countries for instance, it accounts for an estimated 45% of all acute heart failurecases in sub-Saharan Africa.16Similarly, the powerful association between age and heart failure risk has importantimplications in the developing world, where life expectancy has risen from 52 to 57years in lower income nations, and from 63 to 68 years in middle income nations,between 1990 and 2009.17 In India,it is estimated that the number of individuals over the age of 60 years will haverisen to 113 million by 2016, nearly twice the number in this age group in1996.18
Further Risk Score Profiles Based On The Framingham Heart Study
Not only coronary heart disease events but also further risks can be predicted. Risk prediction models for cardiovascular disease outcomes other than CHD events have also been developed by the Framingham Heart Study researchers. Amongst others, a risk score for 10-year risk for atrial fibrillation has been developed.
Also Check: How To Calculate Your Maximum Heart Rate
Framingham Risk Score For Women
Age: 2034 years: Minus 7 points. 3539 years: Minus 3 points. 4044 years: 0 points. 4549 years: 3 points. 5054 years: 6 points. 5559 years: 8 points. 6064 years: 10 points. 6569 years: 12 points. 7074 years: 14 points. 7579 years: 16 points.
Total cholesterol, mg/dL:
- Age 2039 years: Under 160: 0 points. 160-199: 4 points. 200-239: 8 points. 240-279: 11 points. 280 or higher: 13 points.
- Age 4049 years: Under 160: 0 points. 160-199: 3 points. 200-239: 6 points. 240-279: 8 points. 280 or higher: 10 points.
- Age 5059 years: Under 160: 0 points. 160-199: 2 points. 200-239: 4 points. 240-279: 5 points. 280 or higher: 7 points.
- Age 6069 years: Under 160: 0 points. 160-199: 1 point. 200-239: 2 points. 240-279: 3 points. 280 or higher: 4 points.
- Age 7079 years: Under 160: 0 points. 160-199: 1 point. 200-239: 1 point. 240-279: 2 points. 280 or higher: 2 points.
If cigarette smoker: Age 2039 years: 9 points. Age 4049 years: 7 points. Age 5059 years: 4 points. Age 6069 years: 2 points. Age 7079 years: 1 point.
All non smokers: 0 points.
HDL cholesterol, mg/dL: 60 or higher: Minus 1 point. 50-59: 0 points. 40-49: 1 point. Under 40: 2 points.
Systolic blood pressure, mm Hg: Untreated: Under 120: 0 points. 120-129: 1 point. 130-139: 2 points. 140-159: 3 points. 160 or higher: 4 points. Treated: Under 120: 0 points. 120-129: 3 points. 130-139: 4 points. 140-159: 5 points. 160 or higher: 6 points.
Heart Failure With Preserved Ejection Fraction
In diastolic heart failure , the same pathophysiologic processes occur that lead to decreased cardiac output in systolic heart failure, but they do so in response to a different set of hemodynamic and circulatory environmental factors that depress cardiac output.
In HFpEF, altered relaxation and increased stiffness of the ventricle occur in response to an increase in ventricular afterload . The impaired relaxation of the ventricle then leads to impaired diastolic filling of the left ventricle .
Morris et al found that right venticular subendocardial systolic dysfunction and diastolic dysfunction, as detected by echocardiographic strain rate imaging, are common in patients with HFpEF. This dysfunction is potentially associated with the same fibrotic processes that affect the subendocardial layer of the LV and, to a lesser extent, with RV pressure overload. It may play a role in the symptomatology of patients with HFpEF.
You May Like: Panic Attack Heart Palpitations
Descriptive Models Of Heart Failure With Preserved Ejection Fraction
The four descriptive models of HFpEF were used for which the FCHF was required for all . In addition, in descriptive models 24, HFpEF criteria from the ESC guidelines and the PARAGON trial6 were added. The descriptive models were FCHF only FCHF + NPs in sinus rhythm > 300/100 and in atrial fibrillation > 900/400 ng/L for NTproBNP or BNP, respectively FCHF + NPs + ESC echocardiography HFpEF criteria1: relevant structural heart disease and/or diastolic dysfunction, reduced é , or increased E/é ratio and FCHF + NPs + echocardiographic HFpEF criteria from the ongoing PARAGON study6 that requires structural changes with 1 of the following: LAVI > 28 mL/m2 and/or left atrial diameter > 38 mm, or left ventricular hypertrophy, interventricular septal thickness > 10 mm and/or posterior wall thickness in diastole > 10 mm). Patients could fulfil more than one of the descriptive models 14. The patients not fulfilling the FCHF at the baseline outpatient visit were grouped as descriptive model 0 .
Framingham Risk Score For Men
Age: 2034 years: Minus 9 points. 3539 years: Minus 4 points. 4044 years: 0 points. 4549 years: 3 points. 5054 years: 6 points. 5559 years: 8 points. 6064 years: 10 points. 6569 years: 11 points. 7074 years: 12 points. 7579 years: 13 points.
Total cholesterol, mg/dL:
- Age 2039 years: Under 160: 0 points. 160-199: 4 points. 200-239: 7 points. 240-279: 9 points. 280 or higher: 11 points.
- Age 4049 years: Under 160: 0 points. 160-199: 3 points. 200-239: 5 points. 240-279: 6 points. 280 or higher: 8 points.
- Age 5059 years: Under 160: 0 points. 160-199: 2 points. 200-239: 3 points. 240-279: 4 points. 280 or higher: 5 points.
- Age 6069 years: Under 160: 0 points. 160-199: 1 point. 200-239: 1 point. 240-279: 2 points. 280 or higher: 3 points.
- Age 7079 years: Under 160: 0 points. 160-199: 0 points. 200-239: 0 points. 240-279: 1 point. 280 or higher: 1 point.
If cigarette smoker: Age 2039 years: 8 points. Age 4049 years: 5 points. Age 5059 years: 3 points. Age 6069 years: 1 point. Age 7079 years: 1 point.
All non smokers: 0 points.
HDL cholesterol, mg/dL: 60 or higher: Minus 1 point. 50-59: 0 points. 40-49: 1 point. Under 40: 2 points.
Systolic blood pressure, mm Hg: Untreated: Under 120: 0 points. 120-129: 0 points. 130-139: 1 point. 140-159: 1 point. 160 or higher: 2 points. Treated: Under 120: 0 points. 120-129: 1 point. 130-139: 2 points. 140-159: 2 points. 160 or higher: 3 points.
You May Like: Watch With Heart Rate Monitor
Development Of The Minnesota Heart Failure Criteria
We began by examining the prevalence of each criterion variable in all subjects, as well as in cases identified by the short Framingham Criteria separately for MHSAMI and MHSCHF . As expected, more subjects in MHSCHF than in MHSAMI presented with each of the seven heart failure criterion variables. Among cases identified by the short Framingham Criteria, pulmonary rales were less common in MHSAMI as compared with MHSCHF , as were the S3 heart sound and dyspnea . MHSAMI subjects who fulfilled the short Framingham Criteria for heart failure more often had a high heart rate and pulmonary edema . The prevalences of cardiomegaly and low ejection fraction were similar between MHSCHF and MHSAMI.
TABLE 2.
Distribution of heart failure signs and symptoms at the time of the index hospitalization, by data set, Minnesota Heart Survey, 1995 and 2000
| Heart failure sign/symptom present? |
|---|
TABLE 3.
| Heart failure sign or symptom . |
|---|
The posterior probabilities of diagnostic class membership for subjects with all signs and symptoms and a known LVEF , as well as those with missing data on LVEF , are shown in Web appendix 2 . One hundred and fifty of the 192 possible response patterns were observed in our study population we observed at least 10 patients in 82 categories. The response patterns listed in Web appendix 2, together with LCA class assignment based on their respective posterior probabilities, form the Minnesota Heart Failure Criteria.
Heart Failure With Preserved Ejection Fraction Characteristics
As expected in HFpEF patients,11, 12 the patients in KaRen were old , were often female, and had a high prevalence of atrial fibrillation. Moreover, our HFpEF patients had several comorbidities, as expected in patients in their 80s, reflecting frailty. This could contribute to explain why in a previous analysis from KaRen, outcomes were greatly determined by nonCV predictors, in particular age, nonCV syncope, and anaemia, consistent with frailty.7 Conversely, it was notable in the present study that HF factors such as those in FCHF were associated with nonCV outcomes, suggesting complex interactions between HF factors and comorbidities in determining CV and nonCV outcomes.
You May Like: What Is The Recovery Time For Open Heart Surgery
Defintions And Symptoms Of Heart Failure
These definitions of HF generally apply to the stages at which clinical symptoms are present and can be classified by either the New York Heart Association functional classification system or the American College of Cardiology Foundation/American Heart Association classification which describes stages of HF based on structural changes and symptoms.2
Sometimes symptoms are nonspecific, making it unclear if there is heart failure or another medical condition.1 If HF is suspected, the first step in the diagnostic evaluation is a thorough clinical history and a physical exam. These results combined with blood tests will provide an indication of whether further testing is required. If all are normal, it may prompt the physician to look for other causes if an EKG is abnormal it may suggest moving on to other tests, such as an echocardiogram to further evaluate heart function.1
Epidemiology And Natural History Of Chf
Applying these new criteria, McKee and colleagues characterized theepidemiology of CHF in the Framingham cohort. They followed 5,209 men and women fromthe Framingham cohort for up to sixteen years. Eliminated from the analysis were 17subjects who had a diagnosis of CHF at the time of Framingham recruitment. Subjectswere assessed every two years with vital signs, ECG, chest x-ray, urinalysis, vitalcapacity on pulmonary function testing, and blood work. Only 2% of subjectswere completely lost to follow up.3A total of 142 individuals developed definite CHF according to theFramingham criteria. The rate of CHF per person-year rose more than 10 times betweenthe age of 2939 years and 7074years .
The longitudinal design of the cohort facilitated the characterization ofantecedent comorbidities in the 142 individuals with CHF . Definite hypertension, defined using criteriaemployed at the time , was present in 75% of cases. This wastypically accompanied by evidence of cardiomegaly on chest X-ray or ECG. Coronaryheart disease was present in approximately half of the individuals withhypertension. Conversely, coronary heart disease without hypertension was present inonly 10% of individuals with CHF.
Risk factors seen in patients who developed congestive heart failureduring the 16 years of follow-up in the McKee study. HCVD = hypertensivecardiovascular disease, CHD = coronary heart disease, RHD = rheumatic heartdisease.
You May Like: Does Exercise Lower Heart Rate
Clinical Recognition Can Be Challenging
Clinical recognition of HF can be challenging, especially for primary care providers.2 The diagnostic criteria for evaluating heart failure are based on parameters established by clinical experts. There are guidelines established to facilitate the decision making of providers in their routine practice. The guidelines provide up to date clinical information that can help in the diagnosis and treatment of patients with heart failure. Ultimately, decisions on individual patient care are made by the patient and their provider.1
Since the 1970s, multiple sets of diagnostic criteria have been developed with varying sensitivities. The Framingham, Duke, Gothenburg, ESC, and Boston criteria were established before noninvasive techniques for assessing systolic and diastolic dysfunction became widely available. The criteria were designed to assist in the diagnosis of heart failure. All of these criteria have proven helpful in guiding healthcare providers, particularly in diagnosing advanced or severe heart failure.4 Today, the Boston criteria are considered preferable when making a diagnosis of heart failure.5
Acute Heart Failure Diagnostic Workup
The diagnostic workup for acute heart failure begins with a rapid assessment of the patients health history, including a detailed account of any symptoms, history of heart disease in the family, whether the patient smokes, what medications they take, and if they have any other medical conditions. The physical examination should be comprehensive. Patients with acute decompensated heart failure will present a general appearance that includes anxiety, diaphoresis, and poor nutritional status.6
Physicians often use the Framingham Diagnostic Criteria for Heart Failure, which requires the presence of either two major criteria or one major and two minor criteria to make the diagnosis.5 The criteria are as follows:
Read Also: How To Keep Heart Healthy After Heart Attack
Heart Failure Diagnosis And Epidemiology
FAST FACTS
Heart failure diagnosis is usually based on Framingham criteria: either two major, or one major and two minor criteria. Less severe heart failure can manifest without fulfilling these criteria.
The ACCF/AHA 4 Stages and the New York Heart Association functional classifications of heart failure are complementary.
In the United States:
Heart failure annual incidence increased from 250,000 cases in 1970 to 825,000 cases in 2010, contributing to a prevalence of 5.1 million individuals 20 years of age.
Lifetime risk for developing heart failure at the age of 40 years and greater is 1 in 5 in both men and women.
Between 1979 and 2010, annual heart failure hospitalization rates tripled, with 1,023,000 hospital discharges in 2010.
In the Medicare population, heart failure is the most common cause for hospitalization.
After heart failure discharge, readmission rates for recurrent heart failure or other causes are 24% within the first month and 50% within the first 6 months.
In 2012, direct and indirect medical costs associated with heart failure were $30.7 billion.
One in 9 deaths includes heart failure on the death certificate.
The diagnosis of heart failure may emerge from history, physical examination, or laboratory data.
CLINICAL CRITERIA OF HEART FAILURE
|
Weight loss* |
*Weight loss > 4.5 kg 5 days into treatment can be classified as a major or minor criterion
HEART FAILURE CLASSIFICATION
PANDEMIC OF HEART FAILURE
HEART FAILURE AS A DISEASE OF AGING
