Factors That Can Worsen Symptoms Of Heart Failure
The symptoms of heart failure can be worsened by a number of factors, including:
- anaemia
- too much salt, fluid, or alcohol in the diet
- pregnancy
- some viral and bacterial infections
- kidney diseases
Treatment for heart failure may include:
- medicines, such as;
- diuretics to remove excess fluid and improve symptoms of heart failure
- mineralcortiocoid receptor antagonists are also recommended and used in most patients with heart failure to reduce mortality and hospitalisation
- ACE inhibitors to open up blood vessels, reduce blood pressure and reduce sodium retention and water retention
- certain beta-blockers to slow the heart rate and reduce its work
- aldosterone blockers to reduce blood pressure and reduce the effects of damage to the heart muscle
- ACE inhibitors, beta blockers and aldosterone blockers can increase survival and reduce the likelihood of hospitalisation.
B History Part : Prevalence:
Symptoms of Heart Failure
Dyspnea, orthopnea, and paroxysmal nocturnal dyspnea
Dyspnea is one of the common symptoms of heart failure and refers to the awareness of discomfort while breathing. It is often described as shortness of breath, breathlessness, difficulty in breathing, etc.
During the early stages of heart failure, dyspnea usually occurs only during physical activity, but later dyspnea could occur even at rest. Orthopnea is dyspnea at rest in the supine position and it is commonly attributed to pulmonary congestion that occurs during recumbency.
Paroxysmal nocturnal dyspnea refers to the sensation of shortness of breath that awakens the patient within the early hours of falling asleep and usually resolves within 15 to 30 minutes of assuming an upright posture. Because dyspnea is a common symptom in numerous conditions that affect other organ systems such as the lungs, it is not surprising that it has been found to have high sensitivity and positive predictive value but a low specificity for the diagnosis of heart failure.
In contrast, orthopnea and PND are more specific for heart failure. The absence of either of these symptoms is reported to have a high negative predictive value. The exact mechanisms for the development of dyspnea in heart failure are not known, but activation of J receptors in the pulmonary interstitial space by edema fluid could contribute to the sensation of dyspnea.
Fatigue and exercise intolerance
Edema
Wheezing and cardiac asthma
Mortality Differences Over Time
The prognosis for chronic HF has improved, when compared with very early studies such as the Framingham Heart and Offspring Studies , where 1-year survival was 60.5% and 5-year survival was 31.5%. However, more recently, there has been no change or very modest improvements in survival. A large Scottish cohort study found an increased median survival time from 1.3 years to 2.3 years between 1986 and 2002 and similarly a more recent Canadian cohort study found a minimal change in 1-year survival between 1997 and 2007, from 64.3% to 66.2% in acute HF and from 82.3% to 83.8% in chronic HF.
The lack of improvement in survival time is disappointing given the number of evidence-based treatment options that have been in use over the past 20 years. In part this may be explained by the fact no treatment has been shown to improve survival in HFpEF or HFmrEF. Analysis of prescribing patterns does however suggest there is suboptimal use of proven treatments for patients with HFrEF, highlighting an important area of focus for GPs. Patients with HF also frequently have several comorbidities, which will impact on their prognosis, as seen by the range of mortality causes. A holistic approach to care is needed in these patients that goes beyond a simple algorithm-based HF treatment strategy.
Read Also: Can Acid Reflux Cause Palpitations
Terms Used In This Guideline
Heart failure with preserved ejection fraction
This is usually associated with impaired left ventricular relaxation, rather than left ventricular contraction, and is characterised by normal or preserved left ventricular ejection fraction with evidence of diastolic dysfunction .
Heart failure with reduced ejection fraction
Heart failure with an ejection fraction below 40%.
Mineralocorticoid receptor antagonist
History And Physical Examination
Patients with heart failure can have decreased exercise tolerance with dyspnea, fatigue, generalized weakness, and fluid retention, with peripheral or abdominal swelling and possibly orthopnea.3; Patient history and physical examination are useful to evaluate for alternative or reversible causes .3,4,8 Nearly all patients with heart failure have dyspnea on exertion. However, heart failure accounts for only 30 percent of the causes of dyspnea in the primary care setting.24 The absence of dyspnea on exertion only slightly decreases the probability of systolic heart failure, and the presence of orthopnea or paroxysmal nocturnal dyspnea has a small effect in increasing the probability of heart failure .21,23
The presence of a third heart sound is an indication of increased left ventricular end-diastolic pressure and a decreased LVEF. Despite being relatively uncommon findings, a third heart sound and displaced cardiac apex are good predictors of left ventricular dysfunction and effectively rule in the diagnosis of systolic heart failure .21,23
Don’t Miss: Can Reflux Cause Heart Palpitations
Drug Therapy For Heart Failure With Reduced Ejection Fraction
The goal of management of heart failure with reduced ejection fraction is to control symptoms, prevent progression of left ventricular dysfunction, decrease hospitalisation and improve survival. Drugs which block neurohormonal activation are the cornerstone of therapy. They include ACE inhibitors and beta blockers, as well as aldosterone antagonists . A new combination of sacubitril and valsartan enhances neurohormonal modulation by increasing beneficial natriuretic peptides.;
Heart Failuresigns And Symptoms
Heart failure is a condition in which the heart fails to function properly. The terms “heart failure” and “congestive heart failure ” don’t mean that the heart has actually “failed” or stopped but mean one or more chambers of the heart “fail” to keep up with the volume of blood flowing through them.
Heart failure is brought on by a variety of underlying diseases and health problems.
Your condition may involve the left side, the right side or both sides of the heart. Each side has two chambers:
- An atrium or upper chamber
- A ventricle or lower chamber
Any one of these four chambers may not be able to keep up with the volume of blood flowing through it.
Two types of heart dysfunction can lead to heart failure, including:
- Systolic Heart Failure This is the most common cause of heart failure and occurs when the heart is weak and enlarged. The muscle of the left ventricle loses some of its ability to contract or shorten. In turn, it may not have the muscle power to pump the amount of oxygenated and nutrient-filled blood the body needs.
- Diastolic Failure The muscle becomes stiff and loses some of its ability to relax. As a result, the affected chamber has trouble filling with blood during the rest period that occurs between each heartbeat. Often the walls of the heart thicken, and the size of the left chamber may be normal or reduced.
Recommended Reading: Vitamin D3 And Heart Palpitations
Prognosis For Heart Failure
Generally, patients with heart failure have a poor prognosis unless the cause is correctable. Five-year survival after an initial hospitalization for heart failure is about 35% regardless of the patient’s ejection fraction. In overt chronic HF, mortality depends on severity of symptoms and ventricular dysfunction and can range from 10 to 40%/year.
Specific factors that suggest a poor prognosis include hypotension, low ejection fraction, presence of coronary artery disease, troponin release, elevation of BUN, reduced GFR, hyponatremia, and poor functional capacity .
BNP, NTproBNP, and risk scores such as the MAGGIC Risk Score and the Seattle Heart Failure model, are helpful to predict prognosis in HF patients as an overall group, although there is significant variation in survival among individual patients.
HF usually involves gradual deterioration, interrupted by bouts of severe decompensation, and ultimately death, although the time course is being lengthened with modern therapies. However, death can also be sudden and unexpected, without prior worsening of symptoms.
Routine Anticoagulation Has No Role In The Patient With Heart Failure
Although heart failure is accompanied by a hypercoagulable state, data are insufficient to support the use of warfarin in patients in normal sinus rhythm without a history of thromboembolic events or echocardiographic evidence of LV thrombus. Aspirin blunts ACEI-mediated prostaglandin synthesis, but the clinical importance of this finding remains unclear., Current guidelines support the use of aspirin in patients with ischemic cardiomyopathy.
Read Also: How Much Blood Does The Heart Pump
What Is A Heart Failure
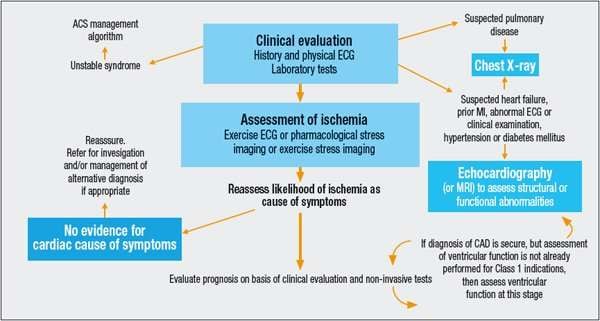
Heart failure is a result of the inability of the cardiac muscle to pump enough oxygenated blood to meet the needs of the various organs and tissues in the body. Diagnosis of heart failure involves figuring out whether the symptoms and physical conditions that a person exhibits indicate heart failure. Usually diagnosing heart failure involves the following steps
- Questioning the patient on their medical history
- Physical examination of the patient
- Performing diagnostic tests to confirm heart failure
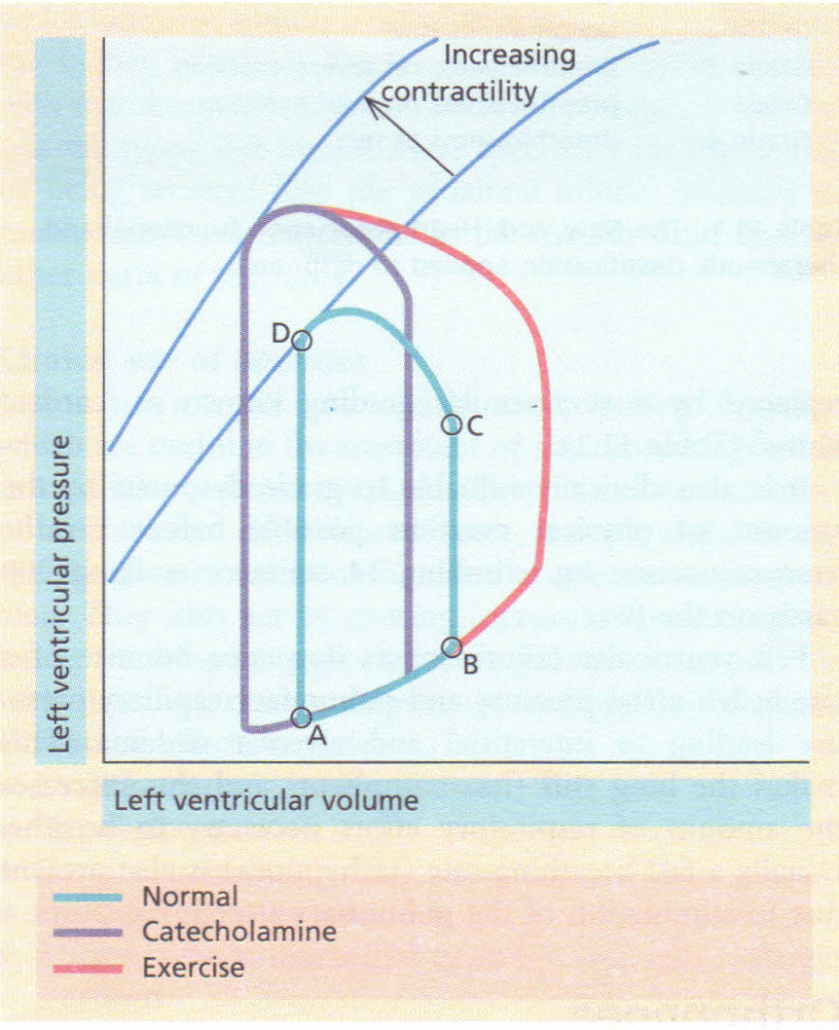
Physiology Of Heart Failure
-
Increasing systolic and diastolic volumes
-
Increasing stroke volume
-
Increasing tissue extraction of oxygen
In well-trained young adults during maximal exercise, heart rate may increase from 55 to 70 beats/minute at rest to 180 beats/minute, and CO may increase from 6 to 25 L/minute. At rest, arterial blood contains about 18 mL oxygen/dL of blood, and mixed venous or pulmonary artery blood contains about 14 mL/dL. Oxygen extraction is thus about 4 mL/dL. When demand is increased, oxygen extraction may increase to 12 to 14 mL/dL. This mechanism also helps compensate for reduced tissue blood flow in heart failure.
You May Like: Reflux And Palpitations
Discussing Prognosis And Hf Trajectory
The Heart Failure Society of America suggest end-of-life planning should be done in coordination with primary care physicians and early enough to allow patients to meaningfully participate. Currently many patients with HF feel they never discuss their prognosis or possible causes of mortality with any healthcare professional, although these discussions are clearly important to help guide treatment and allow for patient-centred advanced care planning.
GPs may be wary of crushing patients hope and so describe HF as an illness to treat rather than an incurable condition and this means the focus of primary care consultations is often on disease management alone. The pattern of illness in HF contributes to this, as doctors find it difficult to predict acute episodes of deterioration during periods of clinical stability and articulating the risk of sudden death is a further challenge. There may be an assumption that other members of the healthcare team such as a specialist nurse or cardiology consultant should take the lead in these discussions. Lack of advanced planning means patients do not get access to all available support including palliative care, which remains underutilised by patients with HF compared with other conditions such as cancer.
Acute Decompensated Heart Failure
Acute decompensated heart failure represents a unique clinical syndrome resulting from interrelated abnormalities of decreased cardiac performance, renal dysfunction, and alterations in vascular compliance. Admission with a diagnosis of ADHF carries a grim prognosis. Half of patients admitted with acute heart failure are readmitted within 6 months, and the mortality after an admission is 12% at 30 days. ADHERE revealed that in-hospital mortality after hospital admission for ADHF ranges from 5% to 8%, with 1-year mortality averaging 40% to 60%. Hospitalization with ADHF is a sentinel event that signals a progression in disease status.
Read Also: Acid Reflux Cause Palpitations
Giving Information To People With Heart Failure
1.3.1 When giving information to people with heart failure, follow the recommendations in the NICE guideline on patient experience in adult NHS services.
1.3.2 Discuss the person’s prognosis in a sensitive, open and honest manner. Be frank about the uncertainty in predicting the course of their heart failure. Revisit this discussion as the person’s condition evolves.
1.3.3 Provide information whenever needed throughout the person’s care.
1.3.4 Consider training in advanced communication skills for all healthcare professionals working with people who have heart failure.
First consultations for people newly diagnosed with heart failure
1.3.5 The specialist heart failure MDT should offer people newly diagnosed with heart failure an extended first consultation, followed by a second consultation to take place within 2;weeks if possible. At each consultation:
-
discuss the person’s diagnosis and prognosis
-
explain heart failure terminology
-
address the risk of sudden death, including any misconceptions about that risk
-
encourage the person and their family or carers to ask any questions they have.
Enlargement Of The Heart
Another important compensatory mechanism is enlargement of the muscular walls of the ventricles . When the heart must work harder, the hearts walls enlarge and thicken, as biceps muscles enlarge after months of weight training. At first, the enlargement allows the heart to maintain the amount of blood it pumps out . However, the enlarged and/or thickened heart eventually becomes stiff, causing or worsening heart failure. Also, the enlargement can stretch the heart valve openings, causing them to malfunction, which causes more pumping problems.
Also Check: How Do You Calculate Max Heart Rate
How Is Congestive Heart Failure Diagnosed
Diagnosis of congestive heart failure is achieved through a comprehensive assessment of the heart muscle, including evaluation of its pumping action and thickness of its walls. This testing also helps to determine the underlying cause of heart failure. Diagnostic tests for congestive heart failure may include:
- Resting or exercise electrocardiogram
- Biopsy or catheterization of the heartand arteries
Aldosterone Antagonism Is Beneficial In Patients With Advanced Heart Failure
The elevated aldosterone levels seen in patients with heart failure promote sodium retention, electrolyte imbalances, and endothelial dysfunction and may directly contribute to myocardial fibrosis. Both the selective agent eplerenone and the nonselective antagonist spironolactone reduce mortality and hospitalizations, with significant reductions in sudden cardiac death ., Hyperkalemia is a concern, especially in patients with underlying chronic kidney disease, and renal function and serum potassium levels must be closely monitored.
Recommended Reading: Does Tylenol Increase Heart Rate
Team Working In The Management Of Heart Failure
1.1.1 The core specialist heart failure multidisciplinary team should work in collaboration with the primary care team, and should include:
-
a lead physician with subspecialty training in heart failure who is responsible for making the clinical diagnosis
-
a specialist heart failure nurse
-
a healthcare professional with expertise in specialist prescribing for heart failure.
1.1.2 The specialist heart failure MDT should:
-
diagnose heart failure
-
give information to people newly diagnosed with heart failure
-
manage newly diagnosed, recently decompensated or advanced heart failure
-
optimise treatment
-
start new medicines that need specialist supervision
-
continue to manage heart failure after an interventional procedure such as implantation of a cardioverter defibrillator or cardiac resynchronisation device
-
manage heart failure that is not responding to treatment.
1.1.3 The specialist heart failure MDT should directly involve, or refer people to, other services, including rehabilitation, services for older people and palliative care services, as needed.
1.1.4 The primary care team should carry out the following for people with heart failure at all times, including periods when the person is also receiving specialist heart failure care from the MDT:
Care after an acute event
For recommendations on the diagnosis and management of acute heart failure see NICE’s guideline on acute heart failure.
Writing a care plan
additional sources of information for people with heart failure.
Stages Of Heart Failure
When you’re diagnosed with heart failure, your doctor will usually be able to tell you what stage it is.
The stage;describes how severe your heart failure is.
It’s usually given;as a class from 1 to 4, with 1 being the least severe and 4 being the most severe:
- class;1 you don’t have any symptoms during normal physical activity
- class 2; you’re comfortable at rest, but normal physical activity triggers symptoms
- class 3 ;you’re comfortable at rest, but minor physical activity triggers symptoms
- class 4; you’re;unable to carry out any physical activity without discomfort and may have symptoms even when resting
Knowing the stage of your heart failure;will help your doctors decide which treatments they think are best for you.
Page last reviewed: 26 October 2018 Next review due: 26 October 2021
Also Check: How Accurate Is Fitbit Charge 2 Heart Rate
Compensated Vs Decompensated Heart Failure
Compensated heart failure is the initial stage of heart failure where different structural and functional changes in the heart compensate for the reduction of cardiac output. ;Symptoms The patient is either asymptomatic or minimally symptomatic with minor symptoms such as grade I dyspnea and mild ankle swelling.
- Exertional dyspnea
- Organomegaly
Management Priority is given to the lifestyle modifications such as cessation of smoking, reduction of alcohol intake, avoiding stress and regular exercises in the management of compensated heart failure. Priority is given to the pharmacological interventions along with radiological and surgical therapeutic procedures in the management of compensated heart failure.
Angiotensin Ii Receptor Blockers Should Be Used In Patients Intolerant Of Aceis But Triple Neurohormonal Blockade Should Be Avoided
Circulating levels of angiotensin II increase to pretreatment levels with long-term angiotensin-converting enzyme inhibition. Angiotensin II receptor blockers bind competitively to the AT1 receptor, providing a downstream effect and thereby blunting this escape phenomenon. A large meta-analysis of 24 randomized trials showed the superiority of ARBs to placebo in patients with intolerable adverse effects with ACEIs and their noninferiority in all-cause mortality or hospitalizations when directly compared with ACEIs. Val-HeFT suggested that addition of valsartan in patients already receiving treatment with ACEIs and -blockers was associated with a trend toward worse outcomes. Similarly, adding valsartan to captopril in patients with heart failure after MI who were receiving background -blocker therapy was associated with an increase in adverse events without any added benefit compared withmonotherapy for either group. A ceiling effect appears to exist beyond which additional neurohormonal blockade may no longer be beneficial and may even trend toward harm. Thus, the clinical dictum should be to use a 2-drug combination first .
Read Also: Does Tylenol Increase Heart Rate
