How Does A Healthy Heart Work
The heart is part of the circulatory system, which carries blood throughout the body. The heart is made of muscle and works like a pump to keep the blood moving through the blood vessels .
The heart has 4 chambers the right atrium and the left atrium on top and the right and left ventricles on the bottom. The heart is divided by a solid wall called the septum into 2 sides: the right side sends blood to the lungs to get oxygen, while the left side of the heart moves oxygen-rich blood to the rest of the body through the aorta .
Blood enters the heart through the right atrium and moves to the right ventricle, where it then moves through the pulmonary artery to the lungs to pick up oxygen. The newly oxygenated blood then enters the heart through the left atrium and moves to the left ventricle, where it is sent through the aorta to the rest of the body.
There are also 4 valves in the heart, which open and close to allow blood to move through the chambers:
- The aortic valve, located on the left side of the heart, between the aorta and the left ventricle.
- The mitral valve, located between the left ventricle and the left atrium.
- The pulmonary valve, located on the right side of the heart between the right ventricle and the pulmonary artery .
- The tricuspid valve, located on the right side of the heart between the right ventricle and the right atrium.
The exterior of the heart.
Blood vesselsarteries, veins, and capillaries–are also involved in helping blood flow:
What Is The Recovery Time
Heart transplant surgery is a complicated, extensive surgery procedure and recovery times are typically longer than most heart surgeries. The expected hospital stay is at least seven to 10 days, and usually up to three weeks. The time you spend in the hospital depends on your specific situation, health and how the surgery went. Overall, recovery from this procedure usually takes several months.
How Heart Failure Is Diagnosed
A diagnosis of heart failure or CHF is made by a doctor who specializes in the diagnosis and treatment of heart-related conditions, called a cardiologist. Your cardiologist will take a complete medical history, conduct a physical exam, and may order a variety of tests, including blood work and imaging tests.
The following tests and scans may be performed to help diagnose heart failure:
- Natriuretic peptide tests: Measures levels of B-type natriuretic peptide or N-terminal prohormone of B-type natriuretic peptide , which are released into the blood by the heart
- Echocardiogram: Determines the percent of blood that is pumped out of the heart with each heartbeat and evaluates the structure and function of the heart
- Electrocardiogram : Provides a tracing of the hearts electrical activity
- Stress test: Measures how the heart responds to exercise or chemically induced stress in a controlled environment
- Cardiac catheterization:Shows the interior of the arteries in your heart to see if they are blocked and allows for measurement of right and left heart pressures
- Other imaging tests such as cardiac computed tomography scan, cardiac magnetic resonance imaging , or nuclear heart scan can be used to show how well the heart is working.
You May Like: Icd10 Code For Heart Failure
Symptoms Of Congestive Heart Failure
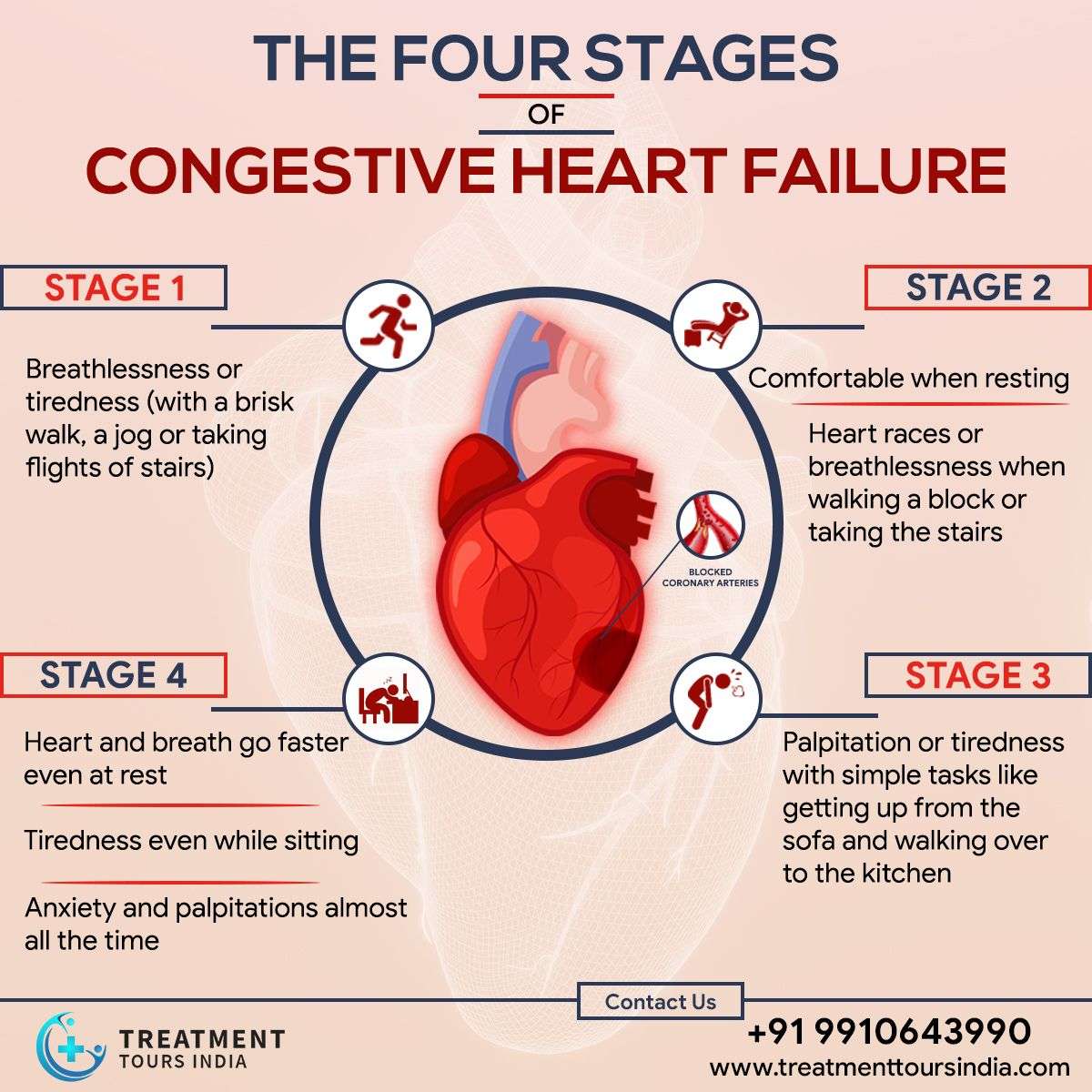
The severity and duration of heart failure symptoms depend on several factors, including the type and class of heart failure.
Some of the most common symptoms include:
- Shortness of breath: Thismay be more prominent with exertion or when lying down. Shortness of breath with exertion occurs due to insufficient blood supply to the body’s cells and tissues with left heart failure. Shortness of breath when lying down can develop when fluid congestion backs up in the lungs due to right heart failure.
- Dizziness, confusion, trouble concentrating, and/or fainting: This can occur with even a mild deficiency of oxygen-rich blood flow to the brain.
- Fatigue: Inadequate supply of oxygen-rich blood to the body’s organs and muscles leads to fatigue.
- Diminished ability to exercise: Due to fatigue and shortness of breath.
- Nocturia : This is caused by an excess of blood flowing through the kidneys when lying down at night. When the kidneys make more urine, it causes an increase in urination.
- Edema : Typically affecting the ankles, feet, lower legs, and abdomen, due to backup of blood to the right side of the heart with right-sided heart failure.
- Rapid or irregular heartbeats : With inefficient heart-pumping action, the heart may intermittently speed up.
- A dry, hacking cough: This is caused by pulmonary edema .
It is important to note that symptoms of CHF may wax and wane. If your symptoms improve, you should continue to follow your CHF treatment plan.
What Happens In Congestive Heart Failure
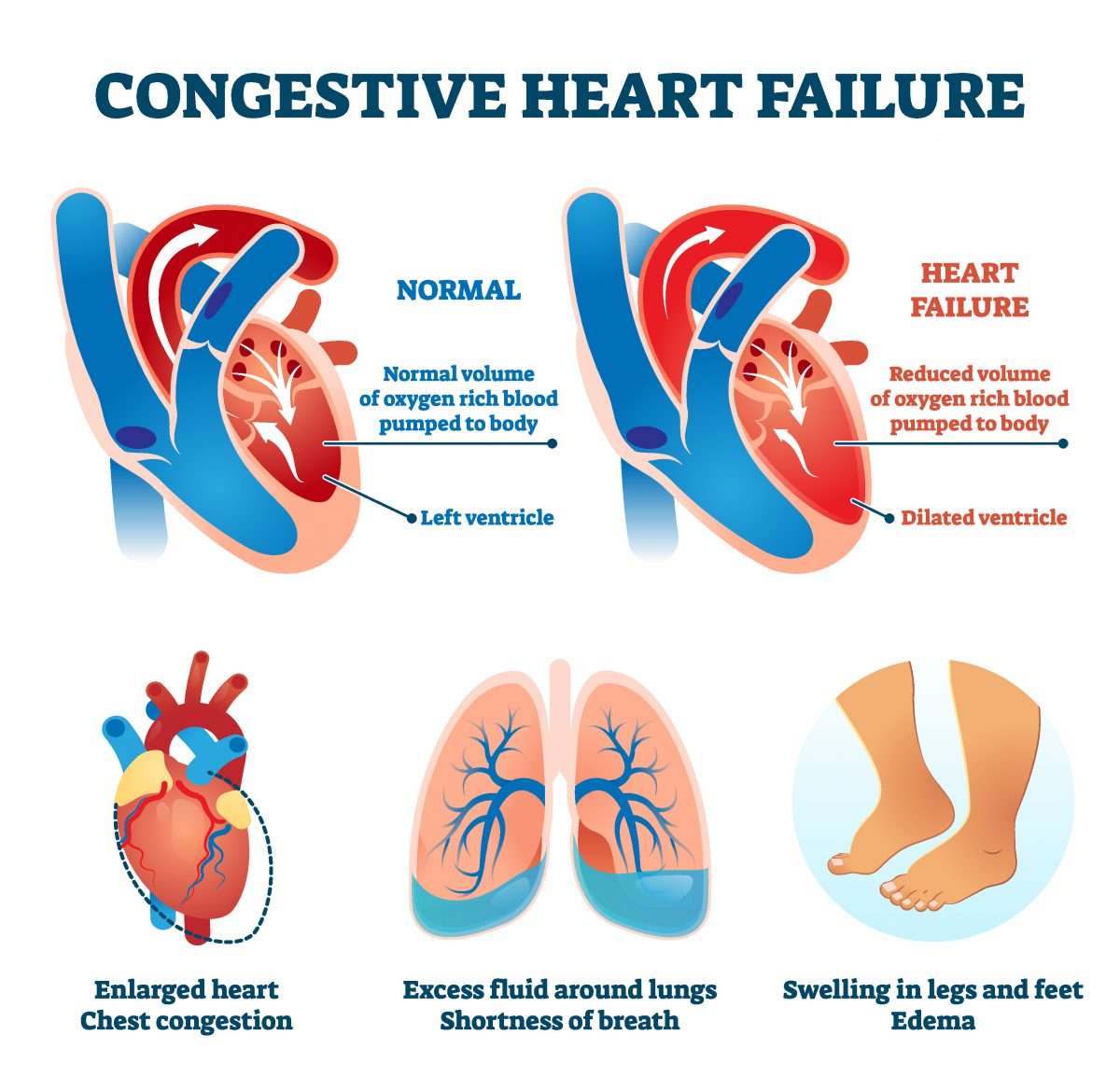
A healthy human heart relaxes and contracts nearly 100,000 times a day and pumps more than 2,000 gallons of blood throughout the body. The cardiovascular system also includes a network of arteries and veins to transport deoxygenated and oxygenated blood to and from the heart. If any part of the system falters, it can disrupt the flow of blood to vital organs.
Heart failure is characterized by a progressive decline in the hearts power to pump blood. When that happens, the heart goes through a series of structural changes and beats faster to pump more blood.
Also, the blood vessels constrict to stabilize blood pressure and restrict blood supply to non-critical organs like the skin and kidneys. When blood flow to the kidneys reduces, it compels the body to retain more fluid and sodium.
All these short-term fixes result in more damage and cause even more stress to the heart muscles. That, in turn, results in further deterioration of the hearts pumping action.
You May Like: Congestive Heart Failure In Dogs Stages
What Medications Are Available To Improve Heart Function
Although diuretics are the first-line agents for congestive heart failure, digoxin is first-line in people who also have atrial fibrillation.
According to Medscape, digoxin produces a small improvement in cardiac output by strengthening the heart muscles. Side effects of digoxin can be serious if dosing is too high.
According to Uptodate, digoxin poisoning can result in life-threatening cardiac arrhythmias, nausea, vomiting, abdominal pain, confusion, delirium, weakness, and electrolyte imbalances.
Prognosis At Each Stage
The outlook for CHF varies greatly between people, as there are many contributing factors for every individuals situation. However, generally speaking, if CHF is discovered in its earlier stages and properly managed, you can expect a far better outlook than if its discovered much later.
Some people whose CHF is discovered early and treated promptly and effectively can hope to have a nearly standard life expectancy.
Recommended Reading: What’s The Difference Between Cardiac Arrest And Heart Attack
If I Have Obesity How Do I Reduce My Risk Of Heart Disease
Losing 5% to 10% of your weight can lower your risk factors for heart disease. Small lifestyle changes can help improve metabolic syndrome, which lessens your heart disease risk. These changes include:
- Aerobic exercise: 150 minutes a week of aerobic exercise can help reduce abdominal fat and overall obesity. That works out to 30 minutes of activity, five days a week. Choosing activities that you enjoy, such as brisk walking, dancing or swimming, can help you stay motivated.
- Dietary changes: Eating fewer calories can help reduce abdominal fat. Changing your diet can also help you lose weight and improve overall obesity. There are studies that support recommending the Mediterranean diet to help reduce your risk of heart attack and death related to heart problems. This diet includes eating mostly plant-based foods such as root and green vegetables, fresh fruits, legumes, nuts and whole grains, plus moderate servings of dairy, eggs, fish, lean poultry and seafood.
What other steps can I take to reduce my risk of heart disease?
Besides lifestyle changes, other options to help reduce your risk of heart disease include:
See your healthcare provider to come up with a plan for your weight loss that makes the most sense for you.
A note from Cleveland Clinic
When Should I See My Healthcare Provider
Your healthcare provider will set up a schedule of visits after your procedure, especially within the first three months. Those visits are critical to making sure you are recovering and arent experiencing any complications or problems related to your new heart.
Your provider will also tell you what signs and symptoms to watch for that mean you need emergency medical attention. Most commonly, the signs and symptoms involve the rejection of your new heart or infections. These symptoms include:
- Drainage or oozing from the incision in your chest.
- Redness or warmth around the incision.
- If your breastbone moves, shifts or causes any kind of cracking or popping sound/feeling when you move.
Your healthcare provider will also recommend and help you do the following:
- Make sure you get preventive dental care .
- Stay current on all your vaccinations .
- Get routine health screenings as needed .
A note from Cleveland Clinic
A heart transplant can be a life-saving medical procedure. However, not everyone can receive a transplant because donor hearts are in limited supply. Healthcare providers can help determine if you’re a good candidate for a transplant, and if so, help you prepare for the next steps. Thanks to advances in medicine, most people feel better and have improved quality of life after their transplant. In the long term, it’s possible to live years or even decades after you get a transplanted heart, giving you a chance to make new memories and experiences with your loved ones.
Recommended Reading: Warning Signs Of Heart Attack For Women
Center For Advanced Heart Failure/cardiomyopathy At Brigham And Womens Hospital
The Center for Advanced Heart Failure/Cardiomyopathy, an integral part of the Heart & Vascular Center at Brigham and Womens Hospital , brings together heart failure experts, including cardiologists, interventional cardiologists, cardiac surgeons, cardiovascular imaging specialists, congenital heart disease specialists, and many others, to care for patients as one team. Together, the team tailors therapies to each patients needs, offering the latest medical, interventional, and surgical approaches to congestive heart failure treatment.
How Can I Improve My Quality Of Life With Heart Failure
There are several things you can do to improve your quality of life if you have heart failure. Among them:
- Eat a healthy diet. Limit your consumption of sodium to less than 1,500 milligrams each day. Eat foods high in fiber. Limit foods high in trans fat, cholesterol, and sugar. Reduce total daily intake of calories to lose weight if necessary.
- Exercise regularly. A regular cardiovascular exercise program, prescribed by your doctor, will help improve your strength and make you feel better. It may also decrease heart failure progression.
- Don’t overdo it. Plan your activities and include rest periods during the day. Certain activities, such as pushing or pulling heavy objects and shoveling may worsen heart failure and its symptoms.
- Prevent respiratory infections. Ask your doctor about flu and pneumonia vaccines.
- Take your medications as prescribed. Do not stop taking them without first contacting your doctor.
- Get emotional or psychological support if needed. Heart failure can be difficult for your whole family. If you have questions, ask your doctor or nurse. If you need emotional support, social workers, psychologists, clergy, and heart failure support groups are a phone call away. Ask your doctor or nurse to point you in the right direction.
Read Also: How To Differentiate Between Anxiety And Heart Attack
How Are Pediatric Congenital Heart Defects Treated
Many children who are born with heart defects do not need treatment. In these cases, the defects are mild or they simply correct on their own .
For children who have a heart defect that must be treated, there are 2 main options: treatment with a catheter, or open heart surgery.
Catheter treatment
Treatment with a catheter is much easier for the child to go through than surgery. Instead of opening the body with an incision as in surgery, the doctor makes a small cut in the skin and inserts a catheter into the body through an artery or vein.
Catheters are used to treat simple heart defects, such as an atrial septal defect. In this procedure, the catheter is moved through a vein until it reaches the septum . There, the catheter places a small device into the septal defect to close it up. The catheter is then removed.
To treat pulmonary valve stenosis, the catheter is equipped with a small balloon that is inflated at the pulmonary valve in order to separate the fused leaflets.
Open heart surgery
In cases where the heart defect cannot be treated with a catheter, the child may need open heart surgery. In these situations, the pediatric heart surgeon opens the chest and operates directly on the heart to repair the defect. This type of treatment is usually done for more serious heart defects.
What Are The Clinical Symptoms Of Congestive Heart Failure
CHF affects many organs in the body due to poor blood perfusion, including the lungs, kidneys, and liver. Trouble breathing and exercise intolerance can occur.
In severe cases, one is unable to perform activities of daily living such as getting out of bed, dressing, walking, and bathing.
In left-sided heart failure, swelling of the feet and legs can occur. Kidney failure can also contribute to swelling.
Unexplained weight loss despite adequate caloric intake is common, also known as cachexia. This Youtube video explains the science behind congestive heart failure and provides an animated model detailing the anatomy of the heart.
Don’t Miss: What Heart Rate Is Dangerous
Stage B Treatment Options
While stage A CHF is managed with lifestyle changes, the treatment plan for stage B typically includes taking medications regularly. People at this stage should still make the same lifestyle changes as those appropriate for stage A. However, your doctor may also prescribe additional treatments such as:
- Angiotensin-converting enzyme inhibitors or angiotensin II receptor blockers, if you arent taking any as part of your stage A treatment plan
- Beta blockers if youve had a heart attack and your EF is 40% or lower, if you arent taking any as part of your stage A treatment plan
- Possible surgery or intervention as a treatment for coronary artery blockage, heart attack, valve disease, or congenital heart disease
What Are The Different Types Of Chf
Heart failure can occur on the left side of the heart, the right side, or both. Most commonly, it begins in the heart’s primary pumping chamber – the left ventricle. Each specific type of CHF is accompanied by its own distinct characteristics:
- Right-sided CHF – Right-sided CHF develops when the right ventricle struggles to deliver blood to the lungs. As blood backs up into the blood vessels, the body begins to retain fluid in the abdomen and lower body.
- Left-sided CHF – Left-sided CHF is the most common form of CHF and begins when the left ventricle cannot effectively deliver blood throughout the body. Eventually, this can lead to fluid retention throughout the body, particularly around the lungs.
Cases of left-sided CHF can be further classified into one of two sub-types, characterized by the manner in which the ventricle is affected:
- Systolic CHF – Systolic CHF occurs when the left ventricle is unable to contract with enough force to circulate blood properly.
- Diastolic CHF – Diastolic CHF occurs when the heart muscle becomes stiff. Because the chamber must relax in order to fill with blood between contractions, this stiffness means that an inadequate amount of blood is available to pump out to the rest of the body.
Also Check: Congestive Heart Failure Belching
How Is Chf Diagnosed
After reporting your symptoms to your doctor, they may refer you to a heart specialist, or cardiologist.
The cardiologist will perform a physical exam, which will involve listening to your heart with a stethoscope to detect abnormal heart rhythms.
To confirm an initial diagnosis, a cardiologist might order certain diagnostic tests to examine your hearts valves, blood vessels, and chambers.
There are a variety of tests used to diagnose heart conditions. Because these tests measure different things, your doctor may recommend a few to get a full picture of your current condition.
Diagnosing Congestive Heart Failure
UT Southwestern cardiologists can often make a preliminary diagnosis of heart failure by taking a detailed medical history and conducting a careful physical examination. Blood and urine tests can reveal problems with the liver and kidneys, measure lipids and thyroid function, and detect signs of diabetes.
Additional tests most noninvasive used to diagnose congestive heart failure might include:
- Electrocardiogram : To look for underlying heart problems such as heart enlargement, abnormal cardiac rhythms, and coronary artery disease
- Echocardiography : To evaluate heart valve function, pumping capacity, and structural changes
- Cardiac MRI: To evaluate the hearts structure and function and look for scarring
- CT imaging: To see detailed, cross-sectional views of the heart and cardiac arteries
- Chest X-ray: To evaluate the structure of the heart and lungs
- Cardiopulmonary stress test: To measure the hearts aerobic capacity
- Cardiac catheterization/angiography: To look for blockages in the coronary arteries
Don’t Miss: How To Stop Heart Palpitations During Pregnancy
Outlook For Heart Failure
Heart failure is a serious long-term condition that will usually continue to get slowly worse over time.
It can severely limit the activities you’re able to do and is often eventually fatal.
But it’s very difficult to tell how the condition will progress on an individual basis.
It’s very unpredictable. Lots of people remain stable for many years, while in some cases it may get worse quickly.
What Are The Treatments For Heart Failure
Your treatment will depend on the type of heart failure you have and how serious it is. There’s no cure for heart failure. But treatment can help you live longer with fewer symptoms.
Even with treatment, heart failure usually gets worse over time, so you’ll likely need treatment for the rest of your life.
Most treatment plans include:
You may need heart surgery if:
- You have a congenital heart defect or damage to your heart that can be fixed.
- The left side of your heart is getting weaker and putting a device in your chest could help. Devices include:
- A biventricular pacemaker .
- A mechanical heart pump or a total artificial heart).
As part of your treatment, you’ll need to pay close attention to your symptoms, because heart failure can worsen suddenly. Your provider may suggest a cardiac rehabilitation program to help you learn how to manage your condition.
Recommended Reading: What Is Open Heart Surgery
