After A Successful Surgery
A liver transplant is compulsory to get rid of hepatic failure entirely. To receive the operation, patients will have to wait until they find a suitable donor. Sometimes, the waiting period is too long for them to bear, and some people never find the right donor.
However, people say that getting the transplant, how hard it may seem, is just the initial stage of the fight. The statistics of the National Institute of Diabetes and Digestive and Kidney Diseases tell us that most hepatic failure patients have to spend three weeks in the hospital to overcome the severe effects of a transplant. This is also the time when doctors evaluate your bodys figures and decide the success degree of the operation. Sometimes, the verdict will be another extended period of home care.
Patients will not be fully healthy after the transplant, of course, and it might take you about one year to get over the adverse effects of the operation. A homecare instructed by a doctor will give you necessary medical, metal, and emotional care.
Cardiac Cachexia Or Anorexia
Cardiac cachexia or anorexia is characterised by loss of appetite, profound weight loss and loss of muscle and fat tissue. You could suggest the person tries eating small, frequent meals. You should consider high calorie, high protein food, and supplement drinks. There are more tips on our page about hydration and nutrition. A dietitian may be able to provide you and your patient with further guidance.
Caring For Someone At The End Of Their Life
When someone you love is facing the end of life, its an extremely worrying and upsetting time. Given the current situation with coronavirus, you might have lots of questions about what youre allowed to do, especially if your loved one is in a hospice or care home. Many care homes are limiting visitors but government guidance has specified that visiting loved ones who are at the end of their life is important and should continue. Check with your loved ones hospice or care home about what restrictions they have in place. Unfortunately, if you have coronavirus symptoms, you wont be able to visit a loved one. Government guidance states that carers are still able to perform their caring duties if the carer doesnt have coronavirus symptoms. If you live with the person you care for and you have coronavirus symptoms, the government are advising you to ask friends and family for help with providing care or contact your local authority or healthcare provider. If someone you care for has a heart condition, they are at higher risk of severe complications of coronavirus. Be mindful of this when visiting and always follow NHS guidance around hand washing and hygiene.
-
Carers UK has helpful coronavirus guidance.
-
If you’re caring for someone who’s approaching their end of life you can find support on our caring for a heart patient page.
You May Like: What Heart Chamber Pushes Blood Through The Aortic Semilunar Valve
Living With Congestive Heart Failure: What To Expect
Yes, there are several lifestyle changes you should take into account if youve been diagnosed with congestive heart failure. But remember your diagnosis doesnt mean you should necessarily stop doing things you love.
You are supposed to be exercising walking, biking, swimming, or doing light weight exercises, says Mountis. The American Heart Association recommends at least 30 minutes of moderate intensity aerobic activity at least five days a week for optimal heart health. Avoid exercises that make you feel breathless, and make sure to talk to your doctor before starting a new exercise routine.
Your healthcare provider will also likely suggest dietary changes that can help reduce the swelling associated with congestive heart failure and slow the progression of the condition. Those changes may include following a low- or reduced-salt diet, or reducing how much fluid you drink to lessen the bodys water content.
Other lifestyle changes that can slow the progression of heart failure include:
Why Its Important To Know Your Ef
 ALQURUMRESORT.COM” alt=”Last stages of heart failure > ALQURUMRESORT.COM”>
ALQURUMRESORT.COM” alt=”Last stages of heart failure > ALQURUMRESORT.COM”> If you have a heart condition, it is important for you and your doctor to know your EF. Your EF can help your doctor determine the best course of treatment for you. Measuring your EF also helps your healthcare team check how well our treatment is working.
Ask your doctor how often you should have your EF checked. In general, you should have your EF measured when you are first diagnosed with a heart condition, and as needed when your condition changes.
Don’t Miss: How To Calculate Target Heart Rate Zone
Hospice And Congestive Heart Failure
When a heart failure patient has been diagnosed with six months or less to live, the added support of hospice care helps them remain in their home until end of life.
Crossroads Hospice & Palliative Care provides a team of nurses, aides, social workers, volunteers, and chaplains to support the patient and their family through the final stages of congestive heart failure symptoms. To learn more about referring your patient to hospice, please call Crossroads at 1-888-564-3405.
Request A Hospice Evaluation
The primary physician may recommend hospice when the time is right. But as anyone who has faced a serious illness knows, patients and family members often must act as their own advocates to receive the care they need and deserve.
You, your loved one or your trusted physician may request an evaluation to see if hospice is an appropriate option for care.
Also Check: Why Do Av Nodal Cells Not Determine The Heart Rate
How Can I Approach A Hospice Discussion With Family Members And Loved Ones
The final months of life are frequently marked by strong emotions and hard decisions. Talking about hospice, even with those closest to you, can be difficult. Here are some tips to get the discussion started.
For patients speaking to families
Education is key. Educate yourself first. By now, youve probably done some research online. It may be helpful to read and share “Considering Hospice: A Discussion Guide for Families” at HospiceCanHelp.com. This discussion guide is a tool for you to print out and use in a family discussion.
Determine what your family members know. Before bringing up hospice, make sure your family members and caregivers have a clear understanding of your health status. People handle difficult information in different ways. If family members do not accept or understand your prognosis, ask your physician, clergy, a VITAS social worker or a trusted friend to speak with them on your behalf.
Discuss your goals for the future, as well as theirs. As a patient, your greatest concern might be to live without pain, to stay at home or not to be a burden. Ask your family members/caregivers about their concerns as they consider the coming days, weeks and months. Explain that hospice is not giving up. It is an active choice to ensure that everyones needs are met.
For families speaking to patients
Strengths And Limitations Of The Study And Method
Our study has a consistent and in-depth focus on the patients perspective. A major strength is the inclusion of very old patients . It is in the nature of qualitative studies to have a small number of participants. Therefore, the findings cannot be generalised, but they provide specific in-depth insights into the perception and personal experience of old and very old patients with severe heart failure. The patients were only recruited in an inpatient setting at two geriatric hospitals and not in general practice or other outpatient settings. Furthermore, the tendency towards socially desirable statements must be considered. To reduce social bias, the interviewer was not involved in the delivery of health care for the patients and was not employed by either of the geriatric hospitals.
Recommended Reading: Can Ibs Cause Heart Palpitations
Liver Failures Usual Symptoms
Cre: nydailynews.com
It is not a myth that liver failure is often hard to diagnose in the first place. The early signs of the deadly disease are prevalent in many other conditions. Therefore, few people may suspect that they have caught one of the most dangerous diseases in the world.
However, next time when you see those signals in yourself or people you know, have a proper check to make sure you are okay. The initial symptoms include:
- Nausea
- Loss of appetite
- Diarrhea
See? So common. But more serious the condition is, the more severe the symptoms will get. Thats when you know the patients need urgent treatment as soon as possible or their life will be in danger. Those signals include:
- Jaundice
- Sleepiness
- Coma
However, as liver failure progresses, the symptoms become more dangerous, requiring urgent care. One of the livers signs is bilirubin conjugating and excreting the substance through the channels of feces and urine. Having too much unconjugated bilirubin in the system is the culprit of confusion, sleepiness, coma, then ultimately, death.
If you see those symptoms in someone, especially when several signals taking place at once, take them to the hospital right away.
How Does A Healthy Heart Work
The heart is a muscle about the size of your fist. The hearts job is to pump blood, rich in oxygen and nutrients, to all parts of your body. The left ventricle is the main pumping chamber. In a normal heart, the left ventricle ejects 50% or more of its blood volume out into circulation. This percentage is called the ejection fraction or EF.
- Heart Failure is not a disease.
- Heart Failure is the name used to describe a set of symptoms.
- Heart Failure is caused by diseases that affect the ability of the heart to pump blood.
Read Also: How Long Can Someone Live With Heart Failure
How Palliative And Hospice Care Can Help With End
Both palliative and hospice care focus on the whole person, including their physical, emotional, social, and spiritual needs. The main difference is that palliative care can be given at any time during a serious illness, and hospice care is given near the end of life typically when a persons prognosis is six months or less.
Palliative and hospice care can also provide help with making difficult treatment decisions, such as whether to be resuscitated if the persons heart stops, or whether to have a tube placed in their throat to help them breathe.
Similarly, people with end-stage heart failure may need to decide when to disable certain medical devices implanted in their body:
- Implantable cardioverter defibrillator . Patients can have the shock function turned off, or not replace the battery when the current one runs out. Electrical shocks from ICDs can cause unnecessary distress for patients and loved ones at the end of life.
- Left ventricular assist device . Typically, the patient decides when this heart pump will be shut off before it is implanted. The decision can be discussed again as the end of life nears.
What Are The Types Of Heart Failure
There are many causes of heart failure, but the condition is generally broken down into two types:
Heart failure with reduced left ventricular function The lower left chamber of the heart gets bigger and cannot squeeze hard enough to pump the right amount of oxygen-rich blood to the rest of the body.
Heart failure with preserved left ventricular function The heart contracts and pumps normally, but the bottom chambers of the heart are thicker and stiffer than normal. Because of this, the ventricles can’t relax properly and fill up all the way. Because there’s less blood in the ventricles, less blood is pumped out to the rest of the body when the heart contracts.
Read Also: How To Calculate Target Heart Rate Zone
Stages C And D With Preserved Ef
Treatment for patients with Stage C and Stage D heart failure and reserved EF includes:
- Treatments listed in Stages A and B.
- Medications for the treatment of medical conditions that can cause heart failure or make the condition worse, such as atrial fibrillation, high blood pressure, diabetes, obesity, coronary artery disease, chronic lung disease, high cholesterol and kidney disease.
- Diuretic to reduce or relieve symptoms.
YOU ARE THE MOST IMPORTANT PART OF YOUR TREATMENT PLAN!
It is up to you to take steps to improve your heart health. Take your medications as instructed, follow a low-sodium diet, stay active or become physically active, take notice of sudden changes in your weight, live a healthy lifestyle, keep your follow-up appointments, and track your symptoms. Talk to your healthcare team about questions or concerns you have about your medications, lifestyle changes or any other part of your treatment plan.
Saturated Fat And Fried Foods
According to the , eating foods high in saturated fat or trans fat can contribute to heart disease. Trans fat is a type of oil that turns into solid fat during food processing.
Foods containing saturated fats include:
- high fat cuts of meat
5.7 million people in the United States have received a diagnosis of heart failure, also known as congestive heart failure.
In this condition, the heart does not pump enough blood to meet the bodyâs needs. It can affect the right side, the left side, or both sides of the heart.
Right sided heart failure involves the inability of the heart to pump enough blood to the lungs to collect oxygen. In left sided heart failure, the heart is unable to pump enough oxygen-rich blood to all parts of the body.
Heart failure can be due to conditions that overwork, damage, and weaken the heart. When this happens, the body releases certain substances into the blood that have a toxic effect on the heart.
These conditions include:
Read Also: Can Antihistamines Cause Heart Palpitations
What Can You Do If You Have Heart Failure
Heart Failure is a serious disorder and is usually a chronic illness. Many forms of Heart Failure can be controlled with medication, lifestyle change and correction of any underlying disorder. The success of your treatment plan depends on your active involvement. Following your treatment plan can make you feel better, prevent your Heart Failure from getting worse and help you live longer.
What you can do:
What Are The Survival Rates For Heart Failure
Survival rates are based on studies of large groups of people with certain diagnoses and generally presented as a 5-year survival rate, which is the percentage of people who lived for at least 5 years after diagnosis.
You can find online calculators that ask you to submit information to get a life expectancy prediction. However, these calculators are not always accurate since they are based on studies of certain population groups over a period of time .
Table: Survival rates for patients with heart failure
| Survival | |
|---|---|
| 10 | About 24.5% on average |
For example, the 5-year survival rate for patients with heart failure is about 76%. This means that about 76 out of 100 people who were diagnosed with heart failure could live for at least 5 years.
Generally, young patients with heart failure have a better prognosis than older patients. Early diagnosis and treatment help increase life expectancy as well.
Don’t Miss: Ibs And Palpitations
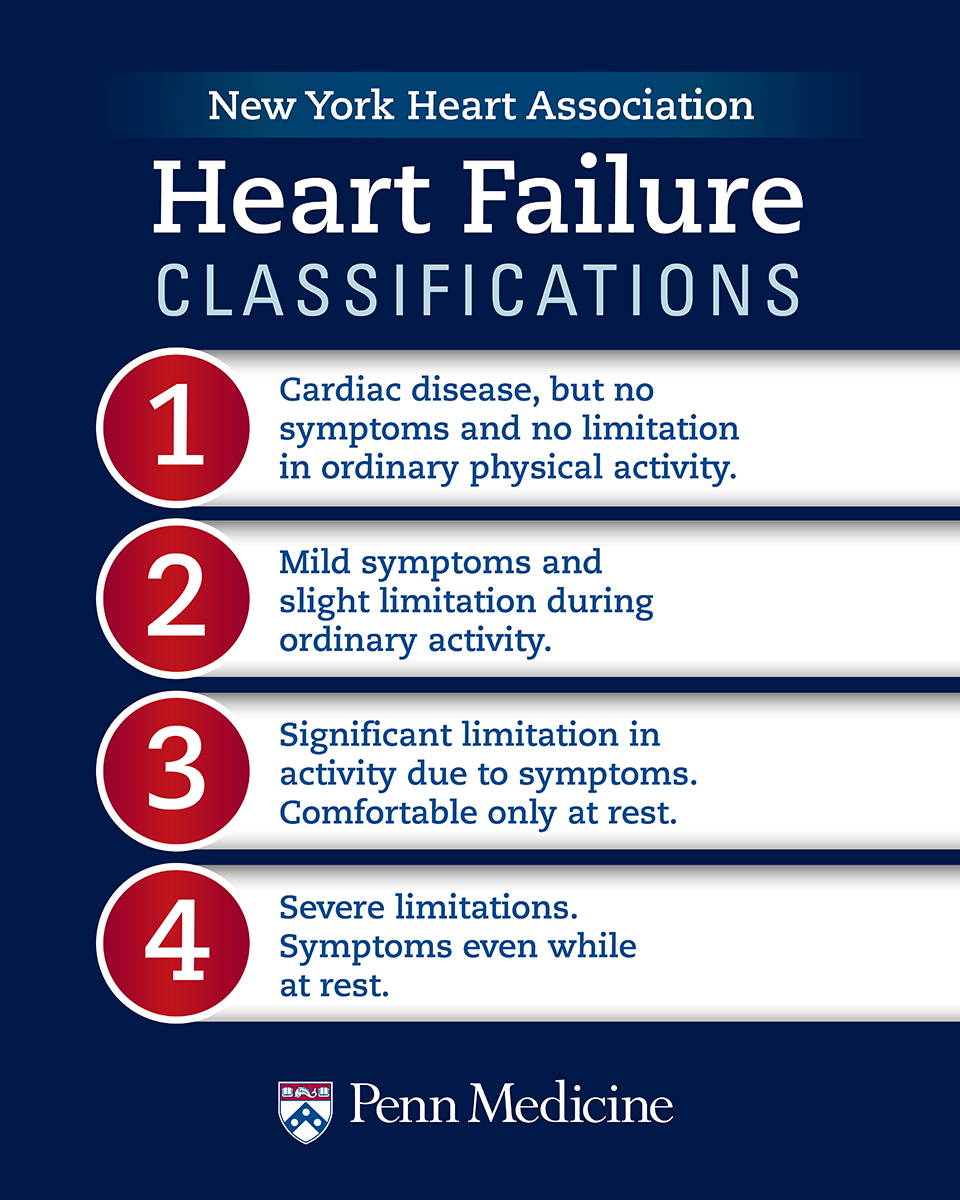
What Are The Stages Of Heart Failure
Heart failure is a chronic long-term condition that gets worse with time. There are four stages of heart failure . The stages range from “high risk of developing heart failure” to “advanced heart failure,” and provide treatment plans. Ask your healthcare provider what stage of heart failure you are in. These stages are different from the New York Heart Association clinical classifications of heart failure that reflect the severity of symptoms or functional limits due to heart failure.
As the condition gets worse, your heart muscle pumps less blood to your organs, and you move toward the next stage of heart failure. You cannot go backwards through the stages. For example, if you are in Stage B, you cannot be in Stage A again. The goal of treatment is to keep you from progressing through the stages or to slow down the progression.
Treatment at each stage of heart failure may involve changes to medications, lifestyle behaviors and cardiac devices. You can compare your treatment plan with those listed for each stage of heart failure. The treatments listed are based on current treatment guidelines. The table outlines a basic plan of care that may apply to you. If you have any questions about any part of your treatment plan, ask a member of your healthcare team.
What Are The Symptoms Of End
Heart Failure: Quick Facts
1. More than 6 million U.S. adults have heart failure.
2. About half of people who develop heart failure die within 5 years of diagnosis.
3. Most people with end-stage heart failure have a life expectancy of less than 1 year.
4. The leading causes of heart failure are diseases that damage the heart, such as heart disease, high blood pressure, and diabetes.
Heart failure worsens over time, so symptoms are most severe during the final stages. It causes fluid to build up in the body, which produces many of these symptoms:
- Shortness of breath . In the final stages of heart failure, people feel breathless both during activity and at rest.
- Persistent coughing or wheezing. This may produce white or pink mucus. The cough may be worse at night or when lying down.
- Weight gain or swelling of the feet, ankles, legs, abdomen, or neck veins.
- Tiredness, weakness.
In addition, people in the final stages of heart failure may suffer from:
- depression, fear, insomnia, and isolation
- anxiety about their future
- trouble navigating the health care system
Recommended Reading: What Causes Left Sided Heart Failure
Heart Failure Patients Too Optimistic
Study Shows Patients Overestimate Their Life Expectancy
A new study shows nearly two-thirds of people with congestive heart failure overestimate their remaining life expectancy by an average of 40% compared with what’s realistic based on their prognosis.
Heart failure, which occurs when the heart is too weak to pump enough blood to meet the body’s needs, causes 55,000 deaths each year and indirectly contributes to 230,000 more deaths annually in the U.S.
Although there have been recent improvements in congestive heart failure treatment, researchers say the prognosis for people with the disease is still bleak, with about 50% having an average life expectancy of less than five years. For those with advanced forms of heart failure, nearly 90% die within one year.
“Patient perception of prognosis is important because it fundamentally influences medical decision making regarding medications, devices, transplantation, and end-of-life care,” write researcher Larry A. Allen, MD, MHS, of the Duke Clinical Research Institute and colleagues in The Journal of the American Medical Association.
