What Should I Do If I Have A Flare
The best way to manage a heart failure flare-up is to have a heart failure action plan. A heart failure action plan is a written document that provides you with instructions and information on how to manage your heart failure on a daily basis, and how to recognise and cope with worsening symptoms.You can develop your heart failure action plan with your healthcare provider and fit the plan to suit how severe your heart failure is and your wishes. When you have a flare-up, follow the steps on your action plan as discussed with your healthcare provider. At each visit, you and your healthcare provider can review your plan and make adjustments as needed.
However, having an action plan doesn’t replace your doctor. It means you can respond quickly and recognise symptoms that require you to seek medical attention. You should still see your doctor as soon as possible after a flare-up. Tell your doctor or nurse if your symptoms don’t improve after following the steps on your action plan.
You may need to go to hospital for severe flare-ups.
|
See your doctor or go to the nearest emergency department if you or someone you care for has heart failure and experiences the following: |
|
Medical History And Physical Exam
Bring a list of your to your doctors appointment, including how often they happen and when they started. Also, bring a list of any prescription and over-the-counter medicines you take. Let your doctor know if you have any for heart failure.
During your physical exam, your doctor will:
- Measure your heart rate, blood pressure, and body weight.
- Listen to your heart with a stethoscope for sounds that suggest that your heart is not working properly.
- Listen to your lungs for the sounds of fluid buildup.
- Look for swelling in your ankles, feet, legs, liver, and veins in your neck.
Diagnosis Of Acute Heart Failure
Acute heart failure, as well as some of its complications such as pulmonary edema, is a very serious condition. Medical attention should be sought immediately if AHF is suspected.
Diagnosis is based on the symptoms, patient history and physical examination for signs that the heart is failing to pump enough blood.
Diagnostic tests can identify what type of heart failure is involved and which ventricle or side of the heart is involved, as treatments can differ. Tests that may be ordered include:
- Electrocardiogram , which uses electrodes to monitor electrical activity in the heart
- Blood oxygen levels should also be monitored
- Various blood tests can show underlying causes for heart failure or reveal effects of complications
- Chest X-ray, which can be useful to monitor response to treatment
- Echocardiogram , which builds a picture of the heart as it pumps blood and can help identify the type of failure
- MRI or computerised tomography scans can show damage to heart muscle
- Nuclear ventriculography, which uses radioactive materials injected into the bloodstream to form an image of the heart moving
Types of heart failure which may occur in combination can be diagnosed by scanning, and testing the capabilities of the heart include:
Don’t Miss: Blood Pressure Vs Heart Rate
Heart Failure Treatment Is A Team Effort
Heart failure management is a team effort, and you are the key player on the team. Your heart doctor will prescribe your medications and manage other medical problems. Other team members — including nurses, dietitians, pharmacists, exercise specialists, and social workers — will help you achieve success. But it is up to YOU to take your medications, make dietary changes, live a healthy lifestyle, keep your follow-up appointments, and be an active member of the team.
If you notice anything unusual, don’t wait until your next appointment to discuss it with your doctor. Call them right away if you have:
- Unexplained weight gain
- Swelling in your ankles, feet, legs, or belly that gets worse
- Shortness of breath that gets worse or happens more often, especially if you wake up feeling that way
- Bloating with a loss of appetite or nausea
- Extreme fatigue or more trouble finishing your daily activities
- A lung infection or a cough that gets worse
- Fast heart rate
- New irregular heartbeat
Dont Wait Until Its Too Late
If diagnosed early enough congestive heart failure can be helped with natural treatments.
There are some promising natural treatment options that can be incorporated into a program that includes medication and medical management of the disease. One issue occurs when the heart lacks energy or ATP and research shows the majority of patients have low CoQ10 levels. Therefore, CoQ10 supplementation can provide some improvement in patients by helping mitochondrial production of ATP improve, giving the heart additional energy reserves.
What I would have hoped for Kathy is that we could have had that conversation twenty years ago because there is so much that can be done when problems with heart function are caught early enough. In my clinic we run organic acids tests on patients even without any signs of advanced heart disease and we often see early warning signs of CoQ10 levels being low by measuring hydroxymethylglutarate levels in the urine. Abnormal hydroxymethylglutarate is representative of low CoQ10 levels and will show up as an easy to identify marker decades before problems like a heart attack or congestive heart failure occur. The organic acids test panels also include markers for oxidative stress, such as 8-OH-DG which is strongly correlated with onset of heart disease. Lowering 8-OH-DG can provide protection to blood vessels and heart tissue and when complemented with a high plant based and antioxidant rich diet it can be the basis of a preventative program.
Read Also: Can Ibs Cause Palpitations
Diagnosing Chronic Heart Failure
Diagnosis is typically based on a personâs medical history, a physical examination and a series of tests. Tests are used by doctors to identify the underlying cause of the chronic heart failure and may include:
- Echocardiogram : This test uses high-frequency sound waves to provide doctors with an insight into the different functions of the heart. It is considered the most important tool in the diagnosis of heart failure.
- Electrocardiogram : Used to test and record the heartâs rhythm and electrical activity.
- Chest X-ray: Able to give doctors a picture of the heart. Can also reveal if there is a buildup of fluid.
- Brain natriuretic peptide or N-terminal pro-BNP : A blood test to measure BNP or NT-proBNP protein levels, both of which tend to be elevated in people with heart failure.
In some cases, other tests, including urine tests and MRI scans, may also be used.
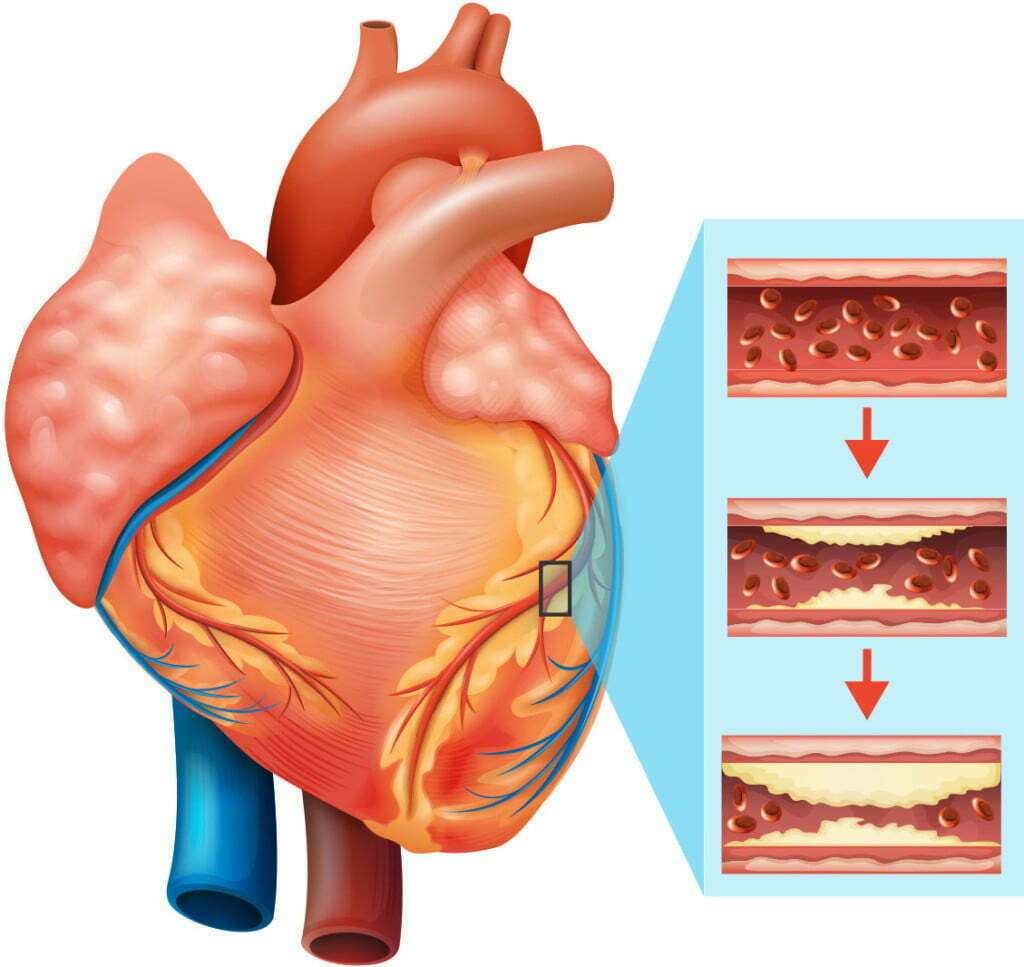
Is Congestive Heart Failure Hereditary
Congestive heart failure can be passed on from generation to generation. Several hereditary factors put people at higher risk if their family members have congestive heart failure, such as high blood pressure, coronary artery disease, cardiomyopathy, and complications from diabetes. A number of conditions can also lead to congestive heart failure, including diseases that directly affect the heart like rheumatic fever and infections such as endocarditis or myocarditis.
Recommended Reading: Lower Part Of Heart Not Working Properly
What Happens In Congestive Heart Failure
The heart has four chambers, a left atrium and right atrium and a left ventricle and right ventricle. Normally, blood:
But in heart failure, the heart cant pump the way it should. The blood and oxygen dont get to the organs. And blood backs up in the heart.
Living Longer And Better
There are many diseases that can masquerade as congestive heart failure. All that swells is not heart failure. In addition to conventional forms of heart failure, there also are similar conditions caused by a stiff heart muscle and secondary heart problems caused by chronic lung conditions. Most of these can be treated.
We now know how important it is to get early diagnosis and treatment for CHF. Patients can now have a brighter outlook on congestive heart failure that wasnt there in decades past. This makes it possible to not only live longer but live better. A fulfilling, symptom-free life is achievable.
COVID-19 showed us that protecting your heart is more important than ever. Be sure to stay on top of treatments, medications, and routine care to keep yourself in the best condition possible to help fight off germs and illnesses.
You May Like: Esophageal Spasms Symptoms Heart Palpitations
How Can I Prevent Heart Failure
You can prevent heart failure by preventing coronary heart disease and heart attack. The best way to do this is to reduce or eliminate the risk factors that lead to heart failure. You could:
- drink alcohol in moderation
- reduce stress and look after your mental wellbeing
If you have had a heart attack, its even more important to manage your risk factors and follow your treatment plan. Make sure you check in frequently with your healthcare team.
Some risk factors such as your age, whether you have other health conditions, or your genes may be outside your control. Speak with your doctor if you have concerns about developing heart failure, and how you can manage it.
Acute Heart Failure Faqs
Q: Can acute heart failure be cured?A: There are different underlying causes of acute heart failure. Most people who develop acute heart failure actually experience a worsening of existing chronic heart failure symptoms. In these cases, there is no definite cure. However, steps can be taken to manage symptoms and to prevent the condition becoming worse. See Preventing acute heart failure.
Also Check: Medical Name For Enlarged Heart
How Is Heart Failure Diagnosed
Your doctor will ask you many questions about your symptoms and medical history. Youâll be asked about any conditions you have that may cause heart failure . Youâll be asked if you smoke, take drugs, drink alcohol , and about what drugs you take.
Youâll also get a complete physical exam. Your doctor will listen to your heart and look for signs of heart failure as well as other illnesses that may have caused your heart muscle to weaken or stiffen.
Your doctor may also order other tests to determine the cause and severity of your heart failure. These include:
Other tests may be ordered, depending on your condition.
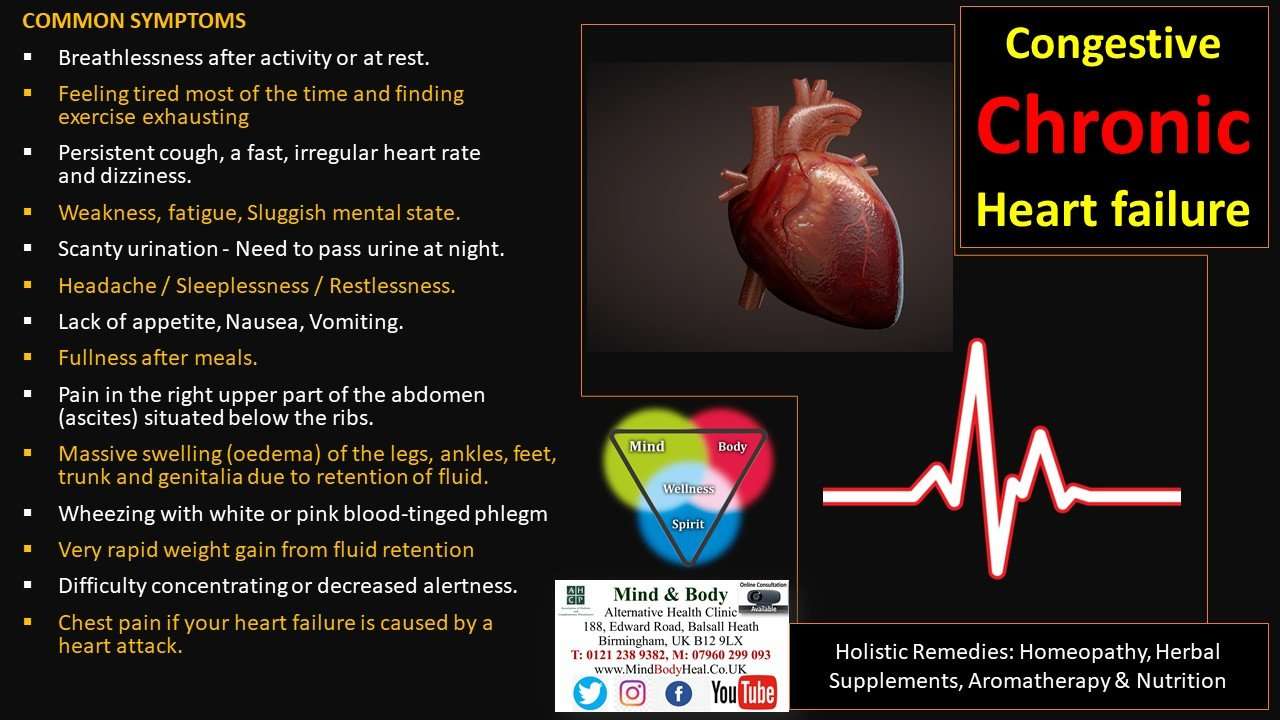
Symptoms Of Acute Heart Failure

Symptoms of acute heart failure can appear very quickly. It can be indicated by the appearance of new symptoms, or by an existing heart condition suddenly becoming worse.
General symptoms of acute heart failure include:
- Shortness of breath while moving or lying flat, also known as dyspnea
- Feeling tired
- A cough that may be worse at night or when lying down
- Swelling of feet, ankles, legs, abdomen or veins in the neck
- Cool peripheries, such as hands and feet, due to reduced cardiac output
- Veins in the neck protruding
Swelling, also known as edema, is caused by fluid building up in different parts of the body because the heart is no longer able to pump efficiently. This is known as congestive heart failure. Depending on the location in the body of the fluid buildup or congestion, this can cause other symptoms. For example:
- Congestion in the kidneys can mean less urine being produced during the day, which leads to frequent urination during the night
- Congestion in the bowel can lead to nausea and vomiting
Medical attention should be sought immediately if any symptoms of acute heart failure develop. Additionally, the free Ada app can be used to carry out a symptom assessment.
Recommended Reading: Heart Rate Up Blood Pressure Down
Why Its Important To Know Your Ef
If you have a heart condition, it is important for you and your doctor to know your EF. Your EF can help your doctor determine the best course of treatment for you. Measuring your EF also helps your healthcare team check how well our treatment is working.
Ask your doctor how often you should have your EF checked. In general, you should have your EF measured when you are first diagnosed with a heart condition, and as needed when your condition changes.
Symptoms Of Heart Failure
Some people who have heart failure have few problems or symptoms. Others have many symptoms. People with heart failure might experience:
- Shortness of breath during activity.
- Shortness of breath when lying down.
- Lack of appetite.
- Waking up in the night, suddenly breathless.
- General tiredness or weakness, including the reduced ability to exercise.
- Swelling of the legs, feet, or ankles.
- Swelling of the abdomen.
- Rapid weight gain .
- Chronic cough or wheezing.
- Nausea.
Don’t Miss: Does Tylenol Help Chest Pain
Prevention Of Chronic Heart Failure
A number of measures can be taken to help lessen the risk of developing chronic heart failure. These include:
- Taking regular exercise, such as walking or swimming
- Maintaining a healthy weight
- Maintaining a healthy and nutritious diet with plenty of vegetables and lean meats
- Limiting alcohol intake
- Stopping smoking
It is also important to address any underlying risk factors, such as high blood pressure and anemia. Doctors are able to advise on how best to manage these conditions.
How Can I Improve My Quality Of Life With Heart Failure
There are several things you can do to improve your quality of life if you have heart failure. Among them:
- Eat a healthy diet. Limit your consumption of sodium to less than 1,500 milligrams each day. Eat foods high in fiber. Limit foods high in trans fat, cholesterol, and sugar. Reduce total daily intake of calories to lose weight if necessary.
- Exercise regularly. A regular cardiovascular exercise program, prescribed by your doctor, will help improve your strength and make you feel better. It may also decrease heart failure progression.
- Don’t overdo it. Plan your activities and include rest periods during the day. Certain activities, such as pushing or pulling heavy objects and shoveling may worsen heart failure and its symptoms.
- Prevent respiratory infections. Ask your doctor about flu and pneumonia vaccines.
- Take your medications as prescribed. Do not stop taking them without first contacting your doctor.
- Get emotional or psychological support if needed. Heart failure can be difficult for your whole family. If you have questions, ask your doctor or nurse. If you need emotional support, social workers, psychologists, clergy, and heart failure support groups are a phone call away. Ask your doctor or nurse to point you in the right direction.
Read Also: Massive Heart Attack Prognosis
Acute Heart Failure Vs Chronic Heart Failure
Acute heart failure has a sudden onset and symptoms can appear without warning.
In chronic heart failure, that difficulty is ongoing and long-term. More people develop chronic heart failure than acute heart failure, and around 80 percent of acute heart failure cases are people with chronic heart failure whose symptoms rapidly become worse.
Signs Symptoms And Complications
Symptoms of heart failure depend on the type of heart failure you have and how serious it is. If you have mild heart failure, you may not notice any symptoms except during hard physical work. Symptoms can depend on whether you have left-sided or right-sided heart failure. However, you can have symptoms of both types. Symptoms usually get worse as your heart grows weaker.
Heart failure can lead to serious and life-threatening complications.
You May Like: Tylenol And High Blood Pressure
How Can I Reduce The Risk Of A Flare
There are things you can to do reduce the risk of a flare-up, including:
- getting support to quit smoking
- getting vaccinated against the flu and pneumococcal disease
- taking your heart failure medicines daily as prescribed by your doctor
- monitoring symptoms such as your breathing and swelling and weighing yourself every day
- joining a cardiac rehabilitation programme
- attending your follow-up appointments regularly.
Information For Healthcare Providers On Heart Failure
The content on this page will be of most use to clinicians, such as nurses, doctors, pharmacists, specialists and other healthcare providers.
The following information on heart failure is taken from Auckland Regional HealthPathways, NZ, accessed March 2021:
|
Practice point |
|
Check new onset shortness of breath Unless history and physical examination clearly indicate a non-cardiac cause for their symptoms, evaluate all patients for heart failure who present with new onset shortness of breath on exertion, orthopnoea, or paroxysmal nocturnal shortness of breath. |
The following information on managing exacerbations of heart failure is taken from Auckland Regional HealthPathways, NZ, accessed March 2021:
|
Red flags |
|
Recommended Reading: Tylenol And Blood Pressure
Improving Quality Of Life
Currently, CHF has no cure. People living with the disease have to commit to heart-healthy lifestyles and take medication regularly.
To stay healthy, here are some tips to follow.
Tips for Living Better with CHF
- Monitor symptoms and check for sudden weight gain and swelling in legs and feet.
- Monitor blood pressure and weight and get lab work done regularly to be aware of your heart health and disease progression.
- Stay positive and find ways to alleviate stress including finding relaxing hobbies, talking to a therapist, finding a support group or talking to loved ones and friends.
- Ask questions about the stage of your disease and guidelines for how active you should be. This includes work, sex and exercise. Depending on the stage of disease, your doctor will have different recommendations about how active you should be, including work, sexm and exercise.
- Keep all appointments with your doctors.
- Make all the lifestyle changes your doctor recommends. If you need help with your diet, ask to see a nutritionist or dietician.
Michelle Llamas has been writing articles and producing podcasts about drugs, medical devices and the FDA for nearly a decade. She focuses on various medical conditions, health policy, COVID-19, LGBTQ health, mental health and womens health issues. Michelle collaborates with experts, including board-certified doctors, patients and advocates, to provide trusted health information to the public. Some of her qualifications include: