Loop Diuretics Ultrafiltration And Dialysis Strategies
Loop diuretics are commonly used in patients with HF. In HF, the doseresponse curve shifts downward and to the right. Thus, a higher dose is required to achieve the same therapeutic effect . However, higher loop diuretic dosages in HF were associated with worse clinical outcomes, including WRF . These studies were criticized since patients with more severe HF and preexisting renal disease require higher diuretic doses . Indeed, in another trial involving 308 patients, after adjusting for cardiovascular risk and clinical stability, diuretic dose was not associated with increased risk . The frequency of dosing of loop diuretics is another issue. A single dose of furosemide elicits transient natriuresis and loop diuretics may be given two or more times per day or continuously. However, continuous dosing was not more effective than an optimally prescribed bolus regimen, as proven in the Diuretic Optimization Strategies Evaluation trial . The addition of nonloop diuretics may overcome the escape phenomenon due to activation of the RAS and sympathetic system and sodium reabsorption by more distal sodium transporters .
The Term Terminal End Stage Of Cardiac Disease Refers To A Patient Who Has A Life Expectancy Of Six Months Or Less After Being Diagnosed With The Condition
It depends on the severity of her heart failure and kidney failure. Only a doctor can make a clinical judgment of the life expectancy of a patient with congestive heart failure. What is the life expectancy for an elderly person with congestive heart failure in a recent study, it was reported that patients hospitalized with moderate systolic heart failure faced a median expected survival time of 2.4 years if they were aged 71 to 80 years and 1.4 years if they were aged 80 years or more.
Vasopressin Type 2 Receptor Antagonists
Vaptans are recently marketed drugs. Since vaptans increase free water excretion and increase serum sodium levels , they may have potential benefits in HF . In animal models of HF, tolvaptan increased urine volume, decreased lung congestion and improved survival but did not modify blood pressure. Additionally, renal histopathologic damage, including tubular fibrosis and glomerulosclerosis, was ameliorated .
There are also human studies. In the EVEREST trial, tolvaptan caused an early and sustained reduction in body weight and improved serum sodium but did not improve mortality or morbidity .
In another study, conivaptan and loop diuretics were compared in stable HF patients. There were no differences with regard to hemodynamics, neurohormonal activation, renal blood flow and GFR. Conivaptan and furosemide similarly increased urine volumes, but only furosemide increased urinary sodium excretion. Conivaptan significantly augmented both the diuretic and the natriuretic response to furosemide when both were combined .
Don’t Miss: Can Low Vitamin D Cause Heart Palpitations
Kidney Disease Congestive Heart Failure
During 1980-2005, approximately 10 million hospitalizations had kidney disease listed as.
whereas 6.9% had septicemia, 6.4% had congestive heart failure, and 5.9% had acute myocardial.
Among patients with chronic kidney disease.
defined by a diagnosis of clinically significant valvular disease, congestive heart failure, myocardial infarction, unstable angina, or stroke.
People with kidney disease or kidney failure are at risk for heart disease. Working with your healthcare provider and dietitian will help you find a lifestyle that can lower your chances of getting heart disease or help keep heart disease from getting worse. If you are on dialysis, you can read more about tips on heart health and dialysis here.
Its contribution to the retention of sodium in patients with congestive heart failure, cirrhosis.
with aldosterone insufficiency , in whom hyperkalemia is common and can.
Figure 1 Cumulative probability of heart failure in populations with chronic kidney disease , dialysis, and a kidney transplant. CHF, congestive heart failure ESKD, end-stage kidney disease. Reproduced with permission from Collins AJ, Foley R, Herzog C, et al. Excerpts from the United States Renal Data System 2007 annual data report.
This is pulmonary edema and if left untreated can cause respiratory distress. Heart failure also affects the kidneys.
Heart Failure and CKD. 6,732 views Apr 22,
Addressing the Disease Burden Associated With Anemia of Chronic Kidney Disease. PeerView CME.
How Do Doctors Treat Heart Disease
If you have heart disease and CKD, your doctor may prescribe medicines to treat your heart disease.
Medicines to treat heart disease include:
- Diuretics : Medicines that lower blood pressure, remove extra fluid and help your kidneys get rid of water and salt.
- Ace inhibitors: Heart medicines that widen your blood vessels, lower blood pressure and improve blood flow.
- Beta blockers: Medicines that lower blood pressure by blocking the hormone adrenaline, which helps your heart beat more slowly and with less force.
Some of these medicines may cause problems with your kidneys. Talk to your doctor about which medicines could work best for you.
Your doctor will also encourage you to make healthy life changes, such as to be active and eat kidney-friendly foods. They can help you find a dietitian to create a healthy eating plan.
Don’t Miss: Which One Of The Following Instructions For Monitoring Your Exercise Heart Rate Is Correct
Dialysis Therapy And Mortality In Older Adults With Heart Failure And Advanced Chronic Kidney Disease: A High
- Sijie Zheng,
Roles Conceptualization, Data curation, Funding acquisition, Investigation, Writing review & editing
Affiliations Department of Nephrology, Kaiser Permanente Oakland Medical Center, Oakland, CA, United States of America, Department of Medicine, University of California, San Francisco, CA, United States of America, Division of Research, Kaiser Permanente Northern California, Oakland, CA, United States of America
-
Roles Data curation, Formal analysis, Investigation, Methodology, Visualization, Writing original draft, Writing review & editing
Affiliation Division of Research, Kaiser Permanente Northern California, Oakland, CA, United States of America
-
Roles Project administration, Supervision, Writing review & editing
Affiliation Division of Research, Kaiser Permanente Northern California, Oakland, CA, United States of America
-
Roles Writing review & editing
Affiliation Department of Nephrology, Kaiser Permanente San Rafael Medical Center, San Rafael, CA, United States of America
-
Roles Conceptualization, Data curation, Funding acquisition, Investigation, Writing review & editing
Affiliation Department of Nephrology, Kaiser Permanente Oakland Medical Center, Oakland, CA, United States of America
We Cant Keep Doing This Any Longer
However, for some patients with chronic heart failure even though their ejection fraction stays the same over several years the kidneys just one day decide to start giving up the good fight.
Creatinine blood test numbers may or may not be getting higher, but the BUN sure will. This stands for blood urea nitrogen.
The kidneys filter toxins out of the body, eliminating them through urine. As the kidneys deteriorate, urea builds up in the bloodstream, affecting the entire body.
The patient grows weaker and develops other symptoms such as brain fog, increasing grogginess and suppressed appetite. In a very elderly patient, these symptoms can mimic the natural effects of old age.
This worsening can go on for a while, but what sometimes happens is that literally overnight theres a much worsened scenario:
The patient is too weak to exit bed, wont eat, has altered mental status and just wants to sleep.
This abrupt worsening of the clinical picture is obvious and prompts family members to get the patient to the emergency room.
The kidneys are now calling it quits.
Theyve compensated long enough. They are going into acute decompensation fueled by chronic heart failure but also the side effects of the diuretic drugs that are taken to combat fluid retention. Old age doesnt help.
This is end renal failure secondary to chronic heart failure. This is a common fatal complication of CHF.
Read Also: How To Bring Your Heart Rate Down
Changes In Kidney Function During Intercurrent Illness
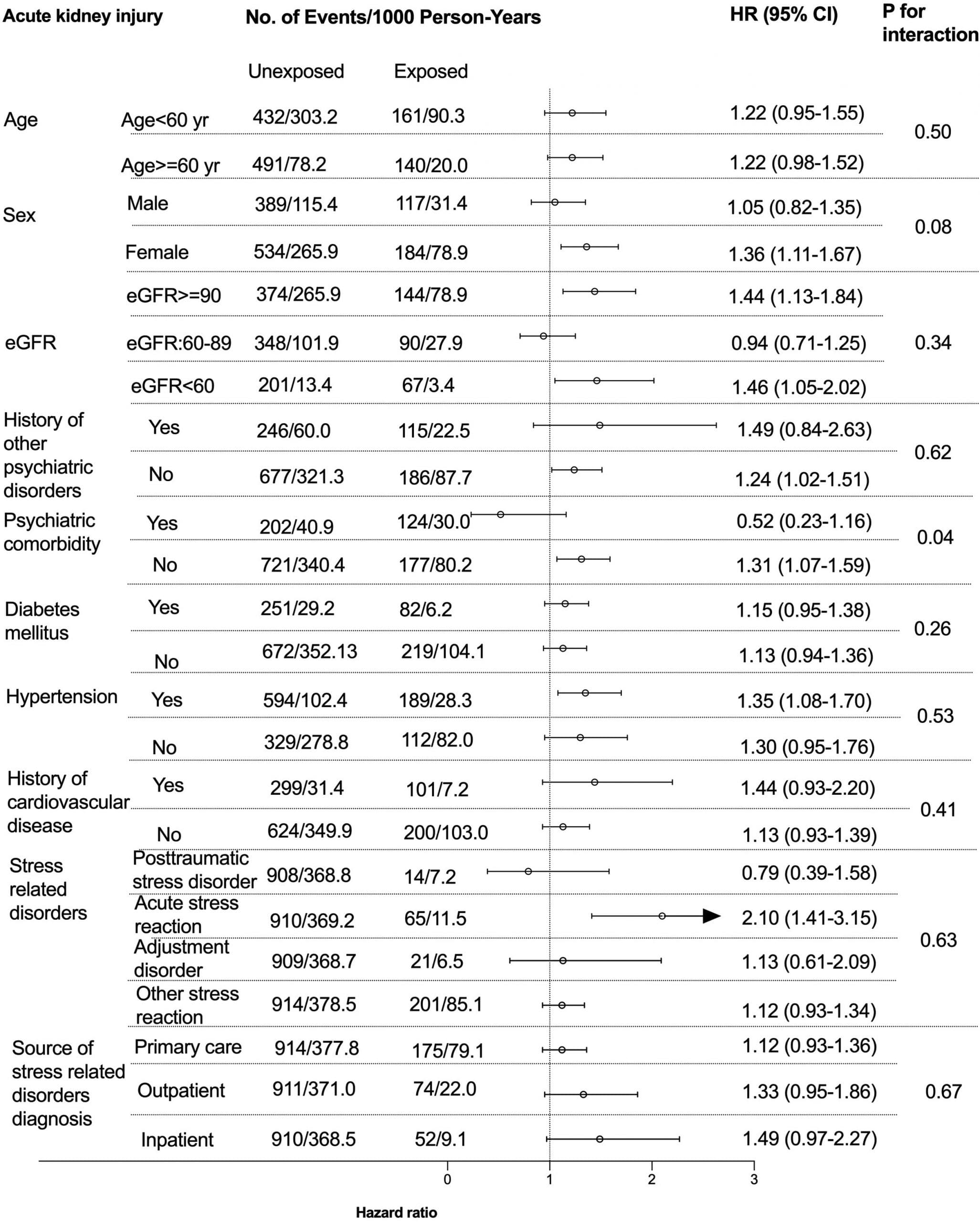
Regardless of whether patients are treated with RAAS inhibitors, changes in renal function are common during acute intercurrent illness the incidence of AKI is between 7% and 18% of hospitalised patients. AKI is a powerful risk marker for poor outcome and is strongly associated with an increase in the risk of subsequent admission for heart failure. Renal function often does not to return to baseline level in survivors of AKI, especially in those with pre-existing CKD.
The incidence of AKI as defined by hospital coding is rising rapidly, which may reflect a genuine increase or simply greater awareness. Conditions associated with the development of AKI are also common indications for RAAS inhibitors and thus AKI in association with RAAS blockade is a common clinical scenario. However, it is not clear that ACEI/ARB therapy alone is associated with a substantially increased risk of AKI.
In patients on a RAAS inhibitor, intercurrent illness commonly causes AKI, but there is no evidence that stopping the RAAS inhibitor is beneficial.
-
If a patient with HFrEF develops hyperkalaemia :
-
Potassium 5.5mmol/L, monitor closely, medication review and consider suspending RAAS inhibitor.
-
Potassium 6.0mmol/L, stop RAAS inhibitor.
If the patient with HFrEF has a rise in creatinine during intercurrent illness:
Stop any other medication that may worsen renal function, including diuretic if clinically appropriate.
If by 30%,RAAS inhibitor should be stopped.
Classification Of Cardiovascularrenal Disorders
In 2015, an international group of 16 board-certified veterinary experts reviewed the cardiovascularrenal syndrome.1 They defined cardiovascularrenal disorders as disease, toxin, or drug-induced structural and/or functional damage to the kidney and/or cardiovascular system, leading to disruption of the normal interactions between these systems, to the ongoing detriment of one or both. The group proposed the following veterinary classifications: primarily cardiovascular, primarily renal, and concurrent disease.
Don’t Miss: How To Rule Out Heart Attack At Home
Other Interventions For Patients With Reduced Ejection Fraction
-Blockers.
In a meta-analysis of patients with heart failure and CKD, -blocker treatment reduced the risk of all-cause and cardiovascular mortality but increased the risk of bradycardia and hypotension . -Blockers need to be introduced with caution, if at all, in patients with cardiogenic shock or decompensated heart failure because they may precipitate worsening of symptoms.
ACE Inhibitors or ARBs.
ACE inhibitors and ARBs often result in mild, short-term declines in eGFR, but they should not be discontinued for this reason . For example, in a secondary analysis of the SOLVD trial, among the individuals randomly assigned to enalapril, the initial decline in kidney function was not associated with adverse outcomes. In fact, patients who continued to receive enalapril despite initial worsening of kidney function had decreased mortality compared with the placebo group . ACE inhibitors or ARBs must be introduced with caution, if at all, in patients with declining kidney function because they may precipitate further GFR reduction. Similarly, in patients with declining kidney function, ACE inhibitors or ARBs at times need to be held given their effect on inhibiting efferent arteriolar vasoconstriction, and thereby promoting additional decline in GFR.
Aldosterone Antagonists.
Hydralazine and Nitrates.
In patients with heart failure and reduced ejection fraction who cannot tolerate or are allergic to ACE inhibitors or ARBs, hydralazine and nitrates are recommended .
What Are The Consequences Of Renal Congestion
Renal congestion leads to increased renal interstitial pressure that affects the entire capillary bed and the tubules, possibly also inducing local hypoxia. Tubular compression raises the luminal pressure, further attenuating the transglomerular pressure gradient, and lowering the GFR. It is important to appreciate that an increase in renal interstitial pressure due to venous congestion is physiologically different from that caused by elevations in arterial pressure, which is associated with natriuresis .
Inflammation may also promote and be a consequence of renal congestion . Inammation may cause vascular dysfunction via endothelial activation and enhanced arterial stiffness, reduce myocardial contractility through functional suppression of contractility and increased myocardial cell death, contribute to progressive renal dysfunction and brosis and increase endothelial permeability, thus facilitating fluid extravasation into lung alveoli and absorption of pro-inammatory endotoxin from the bowel . Conversely, in HF and venous congestion, activation of the RAS and sympathetic system promotes/enhances the inflammatory response. In addition, accumulating evidence suggests that volume overload per se and venous congestion independent of RAS and sympathetic system activation promote the expression of inammatory mediators .
Mechanisms of increased inflammation during venous congestion.
Recommended Reading: How To Know Your Heart Rate
Interactions Between Dm And Ckd
The link between DM and CKD, independent of HF, is beyond the scope of the current review. However, it is important to acknowledge that DM is the leading cause of CKD . Moreover, patients with DM and CKD are at high risk for CVD, including HF . In patients with DM, risk factors for CKD include older age, male sex, smoking, obesity, and hypertension . Among these risk factors, obesity and hypertension can stimulate inflammatory, fibrotic, and hemodynamic changes , resulting in high intraglomerular pressure as well as glomerular hyperfiltration with eventual progression to CKD .
Conflict Of Interest Statement
Financial arrangements of the authors with companies whose products may be related to the present report are listed below, as declared by the authors: Kris Vijay has served as a consultant, speaker, and/or advisor for Amarin Corporation, Amgen, AstraZeneca, Aventyn, Baxter International, Boehringer Ingelheim/Eli Lilly and Company, Esperion Therapeutics, Legacy Heart Care, Novo Nordisk, and Pfizer. He is a board member of the Cardiorenal Society of America, Life 365, and the National Lipid Association. Brendon L. Neuen has received fees for advisory boards, steering committee roles, scientific presentations, and travel from AstraZeneca, Bayer AG, and Janssen Pharmaceuticals, with all honoraria paid to his employer. Edgar Lerma has no conflicts to declare.
Recommended Reading: Is Congestive Heart Failure Hereditary
Discussion Of Aki In This Patient
This patient developed AKI while undergoing diuresis. As alluded to earlier and discussed in more detail later, AKI in the setting of decongestion has been associated with improved prognosis in some studies . The exact pathophysiologic cause of AKI in our patient cannot be determined, but possibilities include decreased forward perfusion and diuretic-induced neurohormonal activation. The worsening of kidney function despite diuresis and paracenteses suggests that increased venous pressure was not the primary cause.
We have been traditionally taught that prerenal azotemia is associated with low FeNa and bland urine sediment, while intrinsic renal disease due to acute tubular necrosis is associated with high FeNa and granular casts. These distinctions, however, are likely neither very sensitive nor specific, and there may be overlap, particularly when there is tubular damage with low FeNa. This suggests the ability of nondamaged parts of the nephron to conserve sodium. Overlap may also occur during diuretic therapy, when the FeNa may be high in the setting of prerenal pathophysiology. In the latter setting, the FeUrea may be more accurate in distinguishing ATN from prerenal azotemia . Given the bland urine sediment and the clinical presentation, the cause of AKI was consistent with CRS, although one cannot rule out some component of ATN because the FeUrea was equivocalit was above the threshold of 35% used to define prerenal azotemia.
Management Of Hf In Patients With Ckd
The co-existence of CKD and HF has major clinical implications as baseline renal function is a strong determinant of outcome in patients with HF. Moreover, renal function is an important factor in the management of HF as it alters the pharmacokinetics and pharmacodynamics of several cardiovascular medications, necessitating drug dose adjustments. Conversely, certain cardiovascular medications can interfere with renal function and, hence, must be administered with caution in patients with underlying CKD.
Because patients with CKD have been relatively underrepresented in HF clinical trials, evidence based management of patients with concomitant CKD and HF is limited. Therefore, treatment strategies in such patients, including those described in this review, are based mainly on results of observational data from unselected cohorts, or from post-hoc analysis of clinical trials in which patient sub-groups with renal dysfunction were included.
Also Check: What Is Considered A Low Heart Rate
Outcomes Of Hf Dm And Ckd
There is now increased research focus on the impact of comorbidities across the spectrum of HF . In particular, DM and CKD are common comorbidities associated with both HF with reduced ejection fraction and HF with preserved ejection fraction . These comorbidities are thought to drive HFpEF development via systemic inflammation and its effects on cardiac function. By contrast, cardiac insult is thought to precede HFrEF, with later development of DM and CKD . However, more research is needed to clarify the mechanisms that underlie the progression of DM and CKD to HFpEF versus those linking HFrEF to DM and CKD.
Regardless of the type of HF, the combined effect of HF, DM, and CKD leads to an increased risk of hospitalization and mortality in the patients who are impacted . Real-world data from almost 90,000 individuals in the United Kingdom reported hospitalization and mortality rates during the first year after HF diagnosis in patients with HF , HF + CKD , HF + DM , and HF + DM + CKD . CV-related hospitalization rates were highest in patients with all 3 conditions compared to patients with HF only , HF + CKD , and HF + DM . Non-CV-related hospitalization rates were also highest among patients with all 3 conditions compared to patients with other morbidities . Last, mortality rates were 78.6% in patients with HF + CKD + DM, 20.5% in patients with HF only, 24.9% in patients with HF + CKD, and 25.1% in patients with HF + DM .
Ckd: Protect Your Heart
Over time, CKD often gets worse and can lead to kidney failure. A person with kidney failure will need regular dialysis or a kidney transplant to survive.
Although dialysis is needed because of CKD, heart disease is the most common cause of death for someone on dialysis. This is because when kidneys dont function properly, the heart has to work harder to circulate blood, leading to high blood pressure and possibly heart disease.
If you or a loved one needs dialysis, look at these tips to help protect your heart:
- Choose foods that are healthiest for your heart and your kidneys. Ask your doctor for a referral to a dietitian whos trained in CKD nutrition to understand which foods and beverages are best for you. You can learn more about dialysis and a healthy diet here.
- Regular physical activity helps to lower your blood pressure and improve your heart health. Moving more doesnt have to be strenuous! Some great ways to get active are gardening, yoga, or a brisk walk around the block. Ask your doctor about which activities are best for you and if there are any you should avoid.
- Manage your weight and blood sugarthis can be done with diet and exercise! Meet with a dietitian to create an eating plan that works for you and your kidneys or check out these resources to help you manage your blood sugar.
Read Also: Congestive Heart Failure Signs And Symptoms
