What To Look For
The good news is that you can tell if you’re beginning to retain fluid merely by getting on the scale. “Weight change is the earliest sign of a problem with fluid balance. Most people will retain 8 to 15 pounds of excess fluid before they see leg and belly swelling. However, symptoms such as coughing and shortness of breath, loose stools, nausea and feeling full when without eating much may develop at the 5-to-7 pound mark” says Dr. Lewis. He instructs his patients to take action as soon as they notice their weight going up. “Don’t wait until you don’t feel well, you may have gained 5 or more pounds by then and could be well on your way to a serious problem.”
If Your Weight Has Increased Ask Yourself:
- Have I consumed more salt/sodium than usual in the last few days?
- Have I been drinking more fluid than recommended?
- Has there been a change in the amount of urine Im producing?
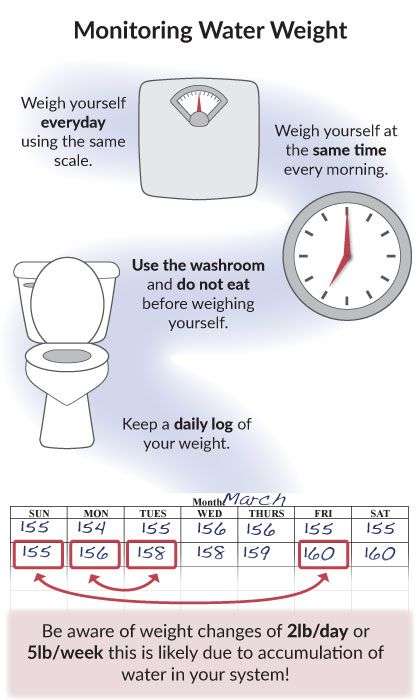
If you have gained more than two pounds in one day, or five pounds in a one week, this may be a sign that you are retaining fluid. You may need to begin taking/take more diuretics and should contact your health care provider.
Stages Of Heart Failure
In 2001, the American Heart Association and American College of Cardiology described the “Stages of Heart Failure.” These stages, which were updated in 2005, will help you understand that heart failure is often a progressive condition and can worsen over time. They will also help you understand why a new medication was added to your treatment plan and may help you understand why lifestyle changes and other treatments are needed.
The stages classified by the AHA and ACC are different than the New York Heart Association clinical classifications of heart failure that rank patients as class I-II-III-IV, according to the degree of symptoms or functional limits. Ask your doctor what stage of heart failure you are in.
Check the table below to see if your therapy matches what the AHA and ACC recommend. Note that you cannot go backward in stage, only forward.
The table below outlines a basic plan of care that may or may not apply to you, based on the cause of your heart failure and your special needs. Ask your doctor to explain therapies that are listed if you do not understand why you are or are not receiving them.
The New York Heart Association clinical classifications of heart failure rank people as class I-II-III-IV, according to the degree of symptoms or functional limits. You can ask your doctor if you want to know what stage of heart failure youâre in.
You May Like: Does Sugar Increase Heart Rate
Tips For Controlling Your Fluid Intake:
- Plan ahead. Spread out the fluid you drink over the day.
- At first, use a 2 L pop bottle to keep track of the fluid you are drinking. For example, when you have a cup of coffee, measure out the same amount of water, and pour it into the pop bottle. When you have filled the bottle, you have had all the fluid you are allowed for the day. You can also keep track by recording the fluid amounts on a piece of paper that you keep on the fridge.
- With a measuring cup, measure the amount of fluid held by your drinking glasses, coffee cup and soup bowl. Knowing how much fluid they hold will help you to plan the amount of fluid you can drink for the day.
- Use small cups and sip slowly.
- Take your pills with apple sauce or soft food.
- Drain excess fluid from canned fruit.
- If you are thirsty, try sucking on small amounts of hard candy or frozen grapes to help with a dry mouth. If you are diabetic, make sure the candies are sugar-free.
- Some people also find that brushing their teeth often or rinsing their mouth with chilled mouth wash helps managing thirst.
Heart Failure Guidelines Go
Developed for healthcare professionals who care for heart failure patients in the post-acute setting, our new Heart Failure Guidelines Go-To-Guide provides information about the latest, evidence-based heart failure treatment guidelines. The guide also includes resources that can help healthcare professionals in the post-acute setting apply the latest guidelines.
Recommended Reading: Can Constipation Cause Heart Palpitations
Monitoring Your Water Weight
Usually, if your weight increases by a few pounds over the course of several days, it is not because you have gained fat or muscle. Noticeable changes in weight over a few days typically relate to accumulation of water, or water weight. This may be the first sign of fluid buildup due to heart failure.
Monitoring your weight is an important way to manage your heart failure. You should:
- Weigh yourself every morning the same way:
- Go to the washroom and empty your bladder
- Wear the same thing every morning
- Dont eat before weighing yourself
- Use the same scale every day
What Is The Outlook For People With Heart Failure
With the right care, heart failure may not stop you from doing the things you enjoy. Your prognosis or outlook for the future will depend on how well your heart muscle is functioning, your symptoms, and how well you respond to and follow your treatment plan.
Everyone with a long-term illness, such as heart failure, should discuss their desires for extended medical care with their doctor and family. An “advance directive” or “living will” is one way to let everyone know your wishes. A living will expresses your desires about the use of medical treatments to prolong your life. This document is prepared while you are fully competent in case you are unable to make these decisions at a later time.
Show Sources
Don’t Miss: What Is The Average Recovery Time For Open Heart Surgery
Heart Failure Treatment Is A Team Effort
Heart failure management is a team effort, and you are the key player on the team. Your heart doctor will prescribe your medications and manage other medical problems. Other team members — including nurses, dietitians, pharmacists, exercise specialists, and social workers — will help you achieve success. But it is up to YOU to take your medications, make dietary changes, live a healthy lifestyle, keep your follow-up appointments, and be an active member of the team.
If you notice anything unusual, don’t wait until your next appointment to discuss it with your doctor. Call them right away if you have:
- Unexplained weight gain
- Swelling in your ankles, feet, legs, or belly that gets worse
- Shortness of breath that gets worse or happens more often, especially if you wake up feeling that way
- Bloating with a loss of appetite or nausea
- Extreme fatigue or more trouble finishing your daily activities
- A lung infection or a cough that gets worse
- Fast heart rate
- New irregular heartbeat
Find Alternative Thirst Quenchers
Its tempting to guzzle a bunch of water when youre thirsty. But sometimes, just moistening your mouth can do the trick.
The next time youre tempted to gulp down some water, try these alternatives.
- Swish water around your mouth and spit it out.
- Suck on sugar-free candy or chew sugar-free gum.
- Roll a small ice cube around the inside of your mouth.
Read Also: How To Wear Heart Rate Monitor
When Should I Get Emergency Care
Go to the ER or call 911 if you have:
- New, unexplained, and severe chest pain that comes with shortness of breath, sweating, nausea, or weakness
- Fast heart rate , especially if you are short of breath
- Shortness of breath that doesn’t get better if you rest
- Sudden weakness, or you can’t move your arms or legs
- Sudden, severe headache
- Fainting spells
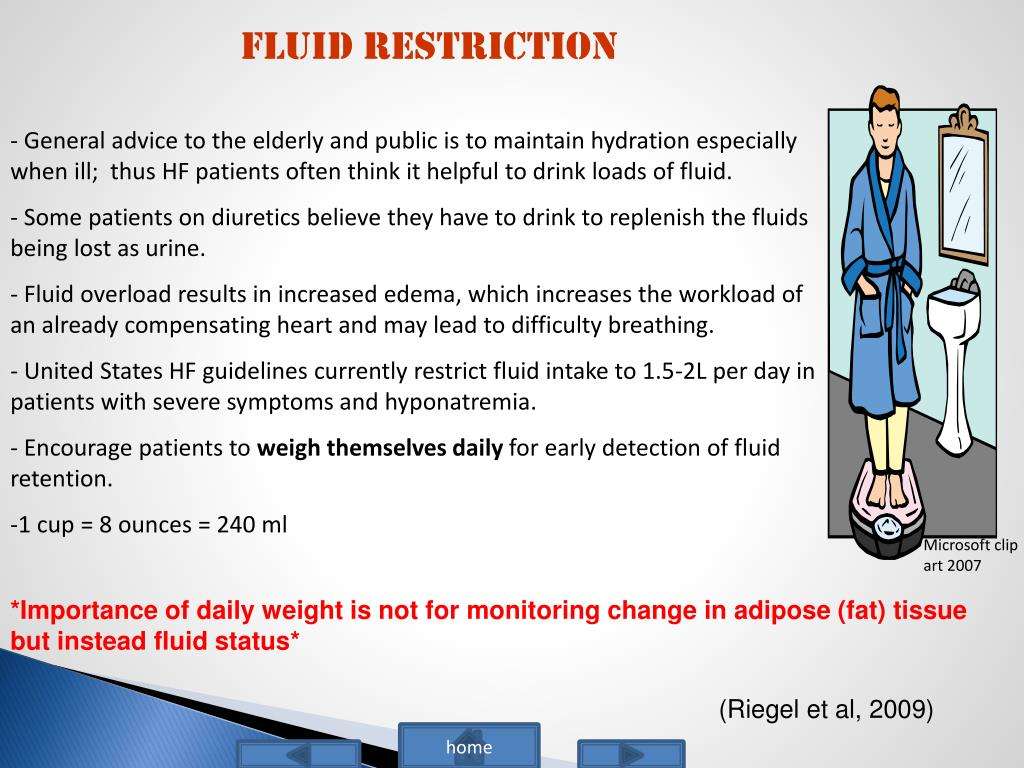
Drink The Right Amount Of Fluids
When your heart failure is not very bad, your health care provider may not place you on a fluid restriction. As your heart failure becomes worse, your health care provider may limit your fluids to 6-9 cups a day. Having other conditions like kidney disease may factor into their decision, too. If you are not sure how much you should drink per day, ask your health care provider.
Most of your hydration should come from water .
Other examples of fluids are:
- Sparkling water
- Milk
- Tea and coffee
- Soft drinks
Also Check: What Is A Normal Heart Rate For A Pregnant Woman
What If You Need Extra Calories And Nutrients
In severe heart failure, more calories are often needed because of the increased workload of the heart and lungs. But calorie requirements will vary, based on your current nutritional status.
If you are underweight or malnourished, you will need to increase your intake to obtain sufficient calories and protein to prevent the loss of muscle tissue, maintain or gain weight, and achieve a healthy level of protein in the blood.
In people whose activity is very limited , it is important to obtain sufficient calories and protein to prevent the development of pressure injuries . Increased food intake is often difficult for individuals who have moderate to severe heart failure because of the congestion, poor appetite, shortness of breath, and nausea that are often caused by this condition or by the medicines used to treat it.
The body’s increased energy demands along with the obstacles to sufficient intake can often lead to malnutrition in people who have heart failure. The following is a list of suggestions to help you boost your appetite and to help you increase your calories and protein with as little volume and discomfort as possible.
Tips for increasing your calorie and protein intake
Is There A Treatment For Heart Failure
There are more treatment options available for heart failure than ever before. Tight control over your medications and lifestyle, coupled with careful monitoring, are the first steps. As the condition progresses, doctors specializing in the treatment of heart failure can offer more advanced treatment options.
The goals of treating heart failure are to try to keep it from getting worse , to ease symptoms, and to improve quality of life.
Some common types of medicines used to treat it are:
- ACE inhibitors
- Aldosterone antagonists
- ARBs
- ARNIs
- Selective sinus node inhibitors
- Soluble guanylate cyclase stimulator
Your doctor may also recommend a program called cardiac rehabilitation to help you exercise safely and keep up a heart-healthy lifestyle. It usually includes workouts that are designed just for you, education, and tips to lower your chance of heart trouble, like quitting smoking or changing your diet.
Cardiac rehab also offers emotional support. You can meet people like you who can help you stay on track.
Also Check: What Is Diastolic Heart Failure
When To Call The Doctor
- You are tired or weak.
- You feel short of breath when you are active or when you are at rest.
- You feel short of breath when you lie down, or an hour or two after falling asleep.
- You are wheezing and having trouble breathing.
- You have a cough that does not go away. It may be dry and hacking, or it may sound wet and bring up pink, foamy spit.
- You have swelling in your feet, ankles, or legs.
- You have to urinate a lot, particularly at night.
- You have gained or lost weight.
- You have pain and tenderness in your belly.
- You have symptoms that you think might be from your medicines.
- Your pulse, or heartbeat, gets very slow or very fast, or it is not steady.
What Are The Types Of Heart Failure
Systolic dysfunction happens when the heart muscle doesn’t contract with enough force, so there is less oxygen-rich blood pumped throughout the body.
Diastolic dysfunction happens when the heart contracts normally, but the ventricles donât relax properly or are stiff, and less blood enters the heart during normal filling.
A calculation done during an echocardiogram, called the ejection fraction , is used to measure how well your heart pumps with each beat to help determine if systolic or diastolic dysfunction is present. Your doctor can discuss which condition you have.
Don’t Miss: What Makes Heart Rate Go Up
Poltica De Acceso Abiertoy Derechos De Autor
Medwave no cobra a los usuarios por el derecho de ver y leer los artículos de texto completo. En otras palabras, el contenido completo de Medwave está liberado y puede ser visto por cualquier público lector, sin necesidad de registrarse en la base de datos de la revista. Sin embargo, si el lector desea recibir las alertas o publicar comentarios a los mismos, deberá estar registrado en Medwave.
Artículos más leídos
Fluid Restriction In Heart Failure
If your heart has stopped beating, then there is no stopping fluid from coming back up. So you simply need to make sure that fluid doesnt get back into your lungs. Fortunately, fluid restriction therapy can help a lot in this regard. The fluid is the liquid which is kept in the lungs. The more fluid in the lungs, the more likely you are to get fluid in your lungs.
In my opinion, the best way to do this is to take a look at your diaphragm. This is a muscle on the front of your body that is responsible for breathing. It can be very hard to keep the diaphragm from moving. So a lot of folks are recommended to wear a lung mask to try and keep it from moving. This however, is a very uncomfortable method of controlling fluid.
In fact, it is a very painful method. Not only is it uncomfortable, but it is also a lot of stress to your lungs. In fact, it can lead to them becoming inflamed which is why I recommend the lung mask method in the first place.
Ive read that if you have heart failure your diaphragm may be very sensitive to any movement of the chest. To prevent this from happening, you can add a layer of fluid to your chest by inserting a tube of fluid into your chest. This tube of fluid can be made from any of a variety of materials that are easily available. For example, a medical grade silicone tube is a common choice.
Read Also: Energy Drinks And Heart Attacks
Taking Action Against Fluid Retention
If you gain more than 2 pounds in a day or 4 pounds in a week, Dr. Eldrin advises taking these steps:
- Think about the foods you ate in the days before your weight gain and look for sources of extra sodium or fluid in your diet that you may be able to eliminate.
- If your weight doesn’t return to normal in a day or two, call your doctor or nurse for advice. You may need to increase your diuretic medicine or reconsider how much fluid you are drinking.
How Does Heart Failure Change How Your Body Regulates And Uses Nutrients
As heart failure progresses, the heart loses its ability to pump strongly, and blood flow throughout the body decreases. This causes a number of reactions throughout the body. Decreased blood flow to the kidneys hinders their ability to remove excess sodium from the body.
Reduced cardiac output from ineffective pumping stimulates the kidneys to retain fluid. Retained fluid causes congestion in the lungs and difficulty breathing. Excess sodium in the body results in the release of a hormone called aldosterone that causes the body to retain fluid as well. Fluid builds up in the body and causes congestion in the lungs, which makes breathing difficult. Also, fluid may build up in the wall of your intestines, which can make it difficult to absorb nutrients from your food. If your body does not receive the nutrition that it needs, you will lose muscle tissue and your body will not be able to fight off infections.
Don’t Miss: What Is Considered Resting Heart Rate
Restricting Water Intake: Necessary Or Not
Dr Vega: That is great advice. It is important to think about water intake, too. Again, a common recommendation to patients is a fluid restriction to less than 2 L a day of free liquids. Again, we are not sure how effective that might be. A meta-analysis of randomized trials that examined liberal fluid intake versus a more restricted intake found no difference in terms of mortality or readmission. Is fluid restriction for everyone, or should you reserve it for certain patients? Patients can get very frustrated with fluid restriction.
Dr Piña: I do not restrict fluids at all. If patients follow the reasonable sodium diet you and I have just discussed, the water follows. A lot of the thirst has to do with the disease and the central mechanism of angiotensin II, which causes thirst, and patients think that they need more fluid. If you neurohormonally block that mechanism well, patients will not have that thirst. So I do not restrict fluid at all unless the patient is hyponatremic. That is when you get into trouble, and that is the hardest one to do. Patients who are not neurohormonally blocked, which is usually the reason behind the hyponatremia, are usually undermedicated. Once you medicate them, the thirst gets better. But until then, it is very hard to restrict fluids. These folks will drink from the faucet. They will drink from the bathroom. There is a huge drive to drink that fluid. Those patients need to be handled very carefully.
What About Supplements?
Tables
Nutrition Guide For Heart Failure
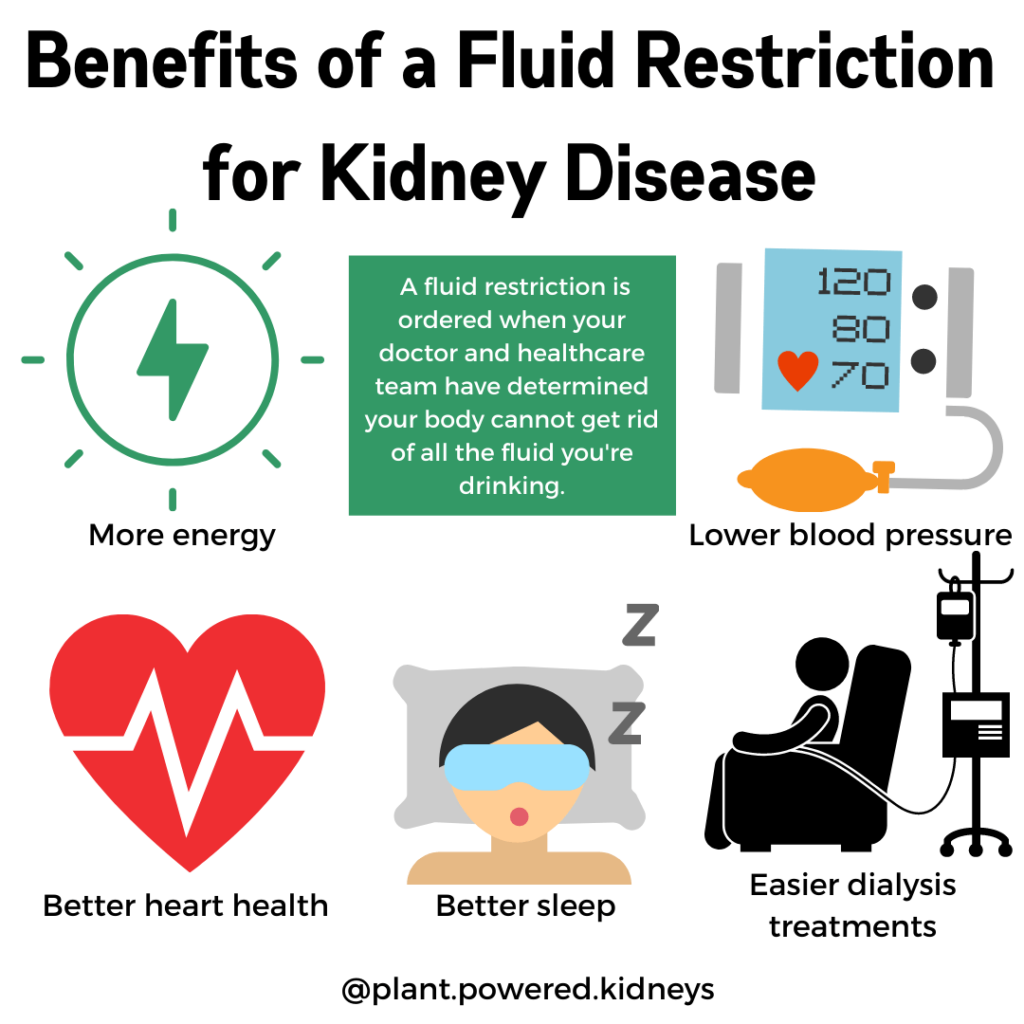
Following a low-sodium diet and drinking less fluid can help you feel better and allow your heart failure medicines to work better. A low-sodium diet may even keep you out of the hospital. It is not an easy diet to follow. You may find eating with heart failure is a bit of a balancing act. While you dont want to eat too much of high sodium foods, you have to be sure to eat enough to maintain good nutrition.
Nutrition and Heart Failure
The recommended salt intake is 2,000 mg of sodium per day.
Salt is a mineral that is made of sodium and chloride. It is found in food, table salt and sea salt. Sodium acts like a sponge and makes the body hold water.
Eating too much sodium when you have heart failure can cause fluid buildup in your legs, stomach and lungs and force you heart to work harder.
Most of the sodium we eat is hidden in foods. Even food that does not taste salty can contain a lot of sodium.
You should restrict the amount of sodium you eat to 2,000 mg or less each day. Try to keep the sodium content of each meal to less than 600 mg. This helps spread out your sodium intake over the day to prevent excessive fluid retention.
You can take a few basic steps to reduce the amount of sodium in your diet:
- Dont add salt when you cook or at the table
- Learn to read food labels
- Choose more foods that are lower in sodium
- Limit high sodium foods
Reading a Food Label for Sodium
Follow these easy steps to read the label:
Low-Sodium Foods
Also Check: Risk Factors For Heart Attack
