Heart Contractions And Diastolic Heart Failure
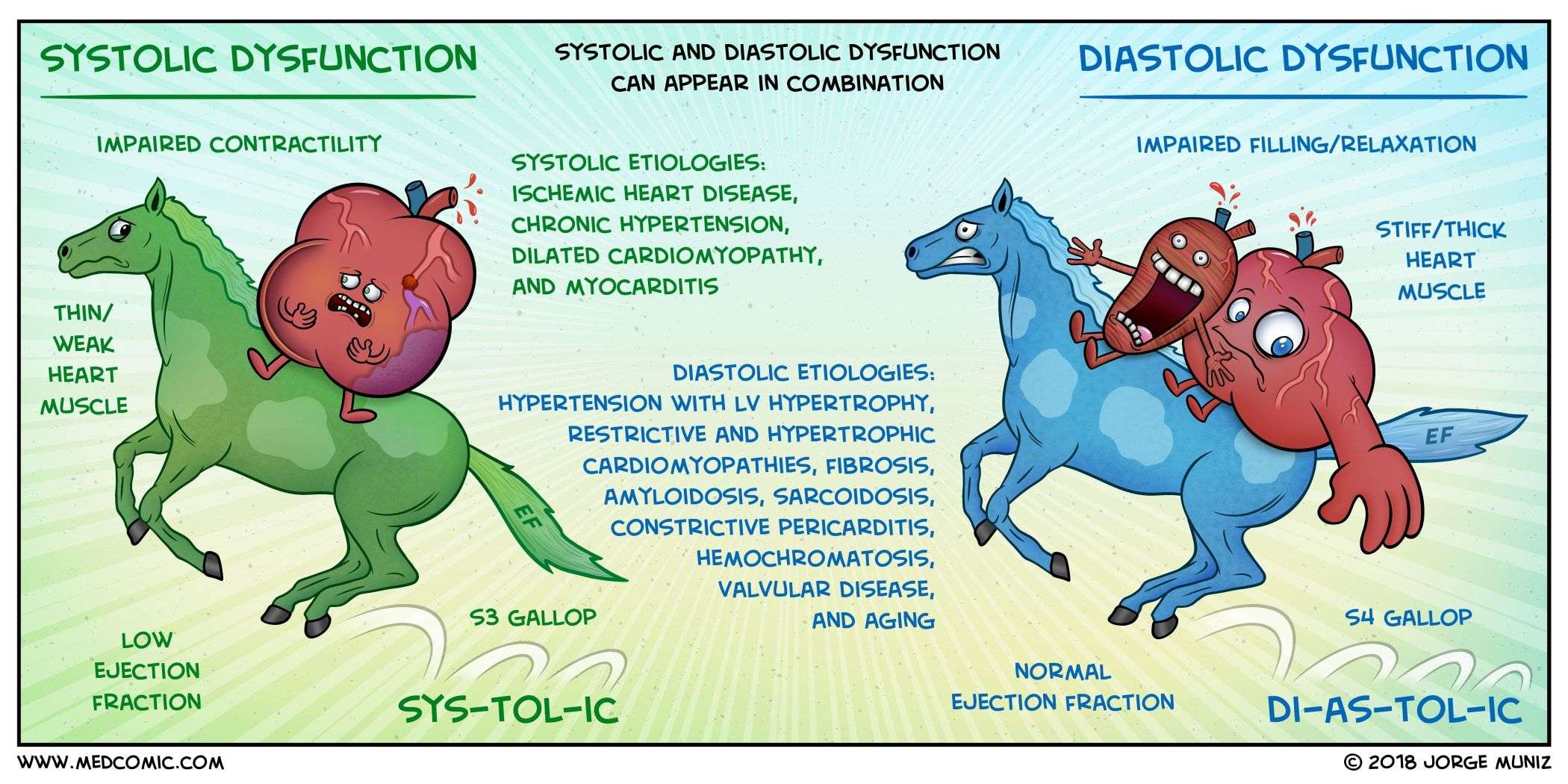
When the heart muscles contract, known as the systole phase, the heart twists and closes slightly like a wringing motion.
Then, in the diastole phase, the muscle fibers relax, unwind, and stretch.
Each of these motions is essential for allowing the heart to expand and draw blood into the ventricles.
With diastolic heart failure, the second phase of a heartbeat is challenged by its inability to relax. This means that the heart must work overtime to do its job.
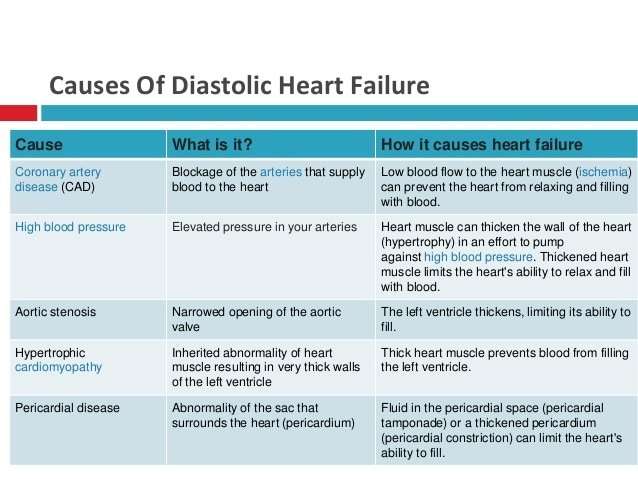
Causes Of Diastolic Heart Failure
As we grow older, our heart and blood vessels become less elastic. This increases their chances of hardening/stiffening. Therefore diastolic heart failure is more common as people get older. Apart from normal aging, the most common reasons are:
High Blood Pressure- If you have this, your heart has to work harder to pump more blood into your body. Thanks to that extra work, your heart muscle can become thick or large, and it eventually becomes stiff.
Diabetes- The disease can make your heart wall thick. Which eventually makes it stiffen.
Coronary artery disease The amount of blood flowing to your heart muscle is blocked or less than normal.
Obesity or Inactivity- With obesity or inactivity, your heart has to work harder to pump blood.
Kidney Disease- Kidney disease can cause heart failure.
Women And Heart Failure
Women are just as likely as men to develop heart failure, but there are some differences:
- Women tend to develop heart failure later in life compared with men.
- Women tend to have heart failure caused by high blood pressure and have a normal EF .
- Women may have more shortness of breath than men do. There are no differences in treatment for men and women with heart failure.
Recommended Reading: Thrz Calculator
Systolic Heart Failure: Causes Symptoms And Treatment
Written byBel Marra HealthPublished onFebruary 21, 2018
Systolic heart failure, also known as a systolic dysfunction, is one of the most common types of heart failure and it typically affects the left ventricle of the heart. The left ventricle does most of the heavy lifting when it comes to pumping blood through the heart. Systole is the critical phase of each heartbeat when the blood is pumped through the heart and sent to other parts of the body.
Ejection fraction is the term used for measuring the exact amount of blood thats being pumped through the different ventricles in the heart at any given time. A normal ejection fraction through the left ventricle should be about 55 percent or more per heartbeat. Any amount lower than that can lead to systolic heart failure, which is essentially a lack of sufficient blood supply being pumped through the heart.
Systolic heart failure occurs when the left ventricle becomes enlarged or inflamed to the point that its unable to fully contract. This prevents it from pumping blood with a strong enough force, which means other parts of the body wont receive sufficient blood supply or the nutrients they need to function normally.
This condition is typically the result of severe or advanced heart disease including high blood pressure, coronary artery disease, cardiomyopathy, and heart valve problems.
Keep reading to gain a comprehensive understanding and definition of systolic heart failure.
Can You Prevent Dd
Although all types of heart failure arent preventable, there are still steps you can take to lower your risk of conditions that can lead to DD. If you show symptoms of DD, your doctor will grade it as mild, moderate or severe.
According to research done on DD and heart disease risk, asymptomatic DD is common in the general population, even in patients without heart failure. It increases with age and is prevalent among older women with systemic hypertension and ventricular hypertrophy. Diastolic dysfunction is linked to excessive weight, diabetes, age and limited physical activity or a sedentary lifestyle.
The heart becomes less efficient at relaxing as we get older, explains Dr. Jaber. When patients come in to get an ultrasound of the heart after experiencing symptoms such as shortness of breath, they should ask about both pumping and relaxation.
Quitting smoking, limiting alcohol intake, dietary changes, weight loss and aggressively controlling hypertension, high cholesterol and coronary artery disease are effective measures you can take to preventDD.
Frequent exercise and managing diabetes should be considered as well, says Dr. Jaber.
You May Like: How Does Heart Disease Affect The Skeletal System
Trouble Arises When The Heart Can’t Properly Relax
Relaxation is every bit as important for your heart as it is for the rest of you. If for some reason the heart has trouble relaxing between beats, then it can’t fill completely. Less blood pumped with each contraction sets the stage for a type of heart failure that goes by many names: diastolic heart failure, heart failure with normal ejection fraction, heart failure with preserved systolic function, and others.
Diastolic heart failure isn’t really new. It’s just that doctors now have tools that let them see how this form of heart failure differs from “regular” heart failure. At least half of the people who develop heart failure each year have diastolic heart failure. Both types of heart failure result in the same thing the heart has trouble supplying the body’s organs and tissues with the oxygen-rich blood they need.
|
Key points
|
Stiffening and bulking up
What to do
In the meantime, the American Heart Association and American College of Cardiology recommend controlling:
Iv Whats The Evidence/references
Borlaug, BA, Paulus, WJ. âHeart failure with preserved ejection fraction: pathophysiology, diagnosis, and treatmentâ. Eur. vol. 32. Heart J 2011. pp. 670
Aurigemma, GP, Gaasch, WH. âClinical practice. Diastolic heart failureâ. N Engl J Med. vol. 351. 2004. pp. 1097
Owan, TE, Hodge, DO, Herges, RM. âTrends in prevalence and outcome of heart failure with preserved ejection fractionâ. N Engl J Med. vol. 355. 2006. pp. 251
Masoudi, FA, Havranek, EP, Smith, G. âGender, age, and heart failure with preserved left ventricular systolic functionâ. J Am Coll Cardiol. vol. 41. 2003. pp. 217
Redfield, MM, Jacobsen, SJ, Burnett, JC. âBurden of systolic and diastolic ventricular dysfunction in the community: appreciating the scope of the heart failure epidemicâ. JAMA. vol. 289. 2003. pp. 194
Wan, SH, Vogel, MW, Chen, HH. âPre-clinical diastolic dysfunctionâ. J Am Coll Cardiol. vol. 63. 2014. pp. 407
Owan, TE, Hodge, DO, Herges, RM. âTrends in prevalence and outcome of heart failure with preserved ejection fractionâ. N Engl J Med. vol. 355. 2006. pp. 251
Bhatia, RS, Tu, JV, Lee, DS. âOutcome of heart failure with preserved ejection fraction in a population-based studyâ. N Engl J Med. vol. 355. 2006. pp. 260
Kitzman, DW, Little, WC, Brubaker, PH. âPathophysiological characterization of isolated diastolic heart failure in comparison to systolic heart failureâ. JAMA. vol. 288. 2002. pp. 2144
Don’t Miss: How To Calculate Target Heart Rate Zone
Diagnostic Approach To Diastolic Heart Failure
The diagnosis of diastolic heart failure requires three conditions to be simultaneously satisfied : presence of signs and symptoms of heart failure presence of normal or only slightly reduced LV ejection fraction and presence of increased diastolic pressure or impaired filling caused by delayed isovolumic relaxation or elevated stiffness. Patients with shortness of breath on exertion, rales, or gallop sound but with near normal systolic function receive usually the diagnosis of congestive heart failure with diastolic dysfunction . More recently a close association of sleep-disorded breathing with diastolic heart failure has been reported but a causal relationship remains to be established . However, attempts to identify diastolic abnormalities have been compromised by the complexity of the factors involved in LV relaxation and filling. Myocardial relaxation, LV suction, viscoelastic properties of the myocardium, ventricular compliance, atrial contraction, left and right ventricular interaction, pericardial restraint as well as heart rate interact and determine directly or indirectly diastolic performance.
Who Gets Diastolic Dysfunction
Diastolic dysfunction and diastolic heart failure are relatively new cardiac diagnoses. They have always been around, of course, but only in the past three decades or so, since echocardiography has been widely used to diagnose heart problems, that these conditions have become commonly recognized.
The diagnosis of diastolic dysfunction is now made quite frequently, especially in people over 45 years of age, most of whom are shocked to hear they have a heart problem at all. While some of these people will go on to develop actual diastolic heart failure, many will not especially if they get appropriate medical care and take care of themselves.
Similarly, diastolic heart failure is also diagnosed frequently today. Almost half the patients who come to emergency roomswith episodes of acute heart failure turn out to have diastolic heart failure.
People with diastolic dysfunction and diastolic heart failure are likely to be older , overweight or obese, hypertensive, female, and have no history of heart attacks . It is currently believed that the risk of developing diastolic dysfunction is the same in men and women, but that older men who are obese and have hypertension are more likely to have heart attacks than women of similar age so their heart failure is more likely to be standard congestive heart failure than diastolic heart failure.
Read Also: Which Of The Following Signs Is Commonly Observed In Patients With Right-sided Heart Failure
What Do The Numbers Mean
Ejection Fraction 55% to 70%
- Pumping Ability of the Heart: Normal.
- Level of Heart Failure/Effect on Pumping: Heart function may be normal or you may have heart failure with preserved EF .
Ejection Fraction 40% to 54%
- Pumping Ability of the Heart: Slightly below normal.
- Level of Heart Failure/Effect on Pumping: Less blood is available so less blood is ejected from the ventricles. There is a lower-than-normal amount of oxygen-rich blood available to the rest of the body. You may not have symptoms.
Ejection Fraction 35% to 39%
- Pumping Ability of the Heart: Moderately below normal.
- Level of Heart Failure/Effect on Pumping: Mild heart failure with reduced EF .
Ejection Fraction Less than 35%
- Pumping Ability of the Heart: Severely below normal.
- Level of Heart Failure/Effect on Pumping: Moderate-to-severe HF-rEF. Severe HF-rEF increases risk of life-threatening heartbeats and cardiac dyssynchrony/desynchronization .
Normal Heart. A normal left ventricular ejection fraction ranges from 55% to 70%. An LVEF of 65%, for example means that 65% of total amount of blood in the left ventricle is pumped out with each heartbeat. Your EF can go up and down, based on your heart condition and how well your treatment works.
HF-pEF. If you have HF-pEF, your EF is in the normal range because your left ventricle is still pumping properly. Your doctor will measure your EF and may check your heart valves and muscle stiffness to see how severe your heart failure is.
Diastolic Heart Failure: Causes Symptoms And Prevention
Diastolic heart failure can be defined as heart failure due to increased resistance in the diastolic filling of the heart. it is usually given as a diagnosis of exclusion when clinical features are suggestive and other pathologies and systolic dysfunction have been excluded.
Diastolic heart failure has latterly emerged as a distinct clinical essence and is characterized by clinical features signifying of heart failure but with minimal or no systolic dysfunction. DHF may occur in up to 50% of patients with heart failure and is associated with the elderly, women, hypertension, obesity, diabetes mellitus, and the presence of concentric left ventricular hypertrophy.
As noted previously, up to 50% of older Heart failure patients have preserved left ventricular systolic function this represents a major clinical problem because few large-scale clinical trials have focused on the treatment of this disorder.
Diuretics are effective in relieving congestion and edema, but they must be used cautiously because patients with diastolic dysfunction are dependent on a sufficient preload to maintain adequate stroke volume. Such patients are often volume sensitive, and are prone to developing pulmonary edema with modest volume overload, while volume contraction and prerenal azotemia may occur in response to over diuresis.
Recommended Reading: Fitbit Charge 2 Accuracy Heart Rate
What Causes Heart Failure
Heart failure can be caused by many medical conditions that damage the heart muscle. Common conditions are:
- Coronary artery disease affects the arteries that carry blood and oxygen to the heart . The normal lining inside the arteries breaks down, the walls of the arteries become thick, and deposits of fat and plaque partially block the flow of blood. Over time, the arteries become very narrow or completely blocked, which causes a heart attack. The blockage keeps the heart from being able to pump enough blood to keep your organs and tissues healthy. When arteries are blocked, you may have chest pain and other symptoms of heart disease.
- Heart attack. A heart attack happens when a coronary artery suddenly becomes blocked and blood cannot flow to all areas of the heart muscle. The heart muscle becomes permanently damaged and muscle cells may die. Normal heart muscle cells may work harder. The heart may get bigger or stiff .
- Cardiomyopathy. Cardiomyopathy is a term that describes damage to and enlargement of the heart muscle not caused by problems with the coronary arteries or blood flow. Cardiomyopathy can occur due to many causes, including viruses, alcohol or drug abuse, smoking, genetics and pregnancy .
- Tobacco and illicit drug use.
- Medications. Some drugs used to fight cancer can lead to heart failure.
Heart Failure Treatment Depends On The Cause
Though both types of heart failure indicate that the heart isnt able to do its job, the treatment plans for each are different.
For systolic heart failure, Yancy says, theres a suite of medicines and in some cases medical devices that are proven to be effective. When those medicines are taken correctly, a patients condition almost always improves.
If a doctor suspects you may have diastolic heart failure, they will probably don a detective hat and start to explore, looking for other conditions that may be causing your symptoms. These include high blood pressure, diabetes, kidney disease, coronary artery disease, or atrial fibrillation, a heart rhythm disorder. Those diseases taken together are probably responsible for 85 to 90 percent of heart failure, when the heart muscle is still beating adequately but nevertheless the heart isnt working properly, says Yancy.
Then its a matter of evaluating the hypertension, searching for the coronary disease, treating the atrial fibrillation, controlling diabetes, addressing the kidney function, and managing the obesity, he says. Its more about evaluation and strategies rather than a list of drugs to help alleviate the heart failure that results from one of these conditions.
Don’t Miss: Does Benadryl Lower Heart Rate
What Is Ejection Fraction
Ejection fraction is the measurement of the amount of blood that is pumped out of the heart via the left ventricle with each beat/contraction. The measurement is only taken from the left ventricle. EF is measured during an echocardiogram which is like an ultrasound of the heart. Normal EF is anything 55% or higher. Reduced EF is anything 50% or lower. An EF of between 50%-55% is generally considered borderline. With diastolic heart failure, the ejection fraction is usually preserved which means it is 50% or higher.
Pathophysiology Of Impaired Diastolic Relaxation
To start with, here’s a reminder of what a normal LV pressure-volume loop looks like. The shape of this loop is governed by the end-systolic and the diastolic pressure-volume relationships on the bottom, the diastolic pressure-volume relationship and on the top the end-systolic pressure volume relationship.
Now, the term “elastance” will be used here because elastance is the change in pressure per change in volume, whereas compliance is a change in volume per change in pressure. The flimsy rationale for using this term is as follows.
- In diastole, the preload volume is what distends the ventricle.
- The ventricle experiences an increase in pressure as the result of this distension
- The mechanical property of the ventricle which changes this pressure/volume relationship is described by the resistance to deformation or the tendency to spring back to original dimensions in response to distension.
- For this property, the closest mechanical terminology is “elastance”
- Conversely, compliance is the change in volume per change in unit pressure, and it would make no logical sense to discuss the ventricle in those terms because the change in volume is the initiating factor.
Anyway. Here’s what an LV pressure-volume loop looks like when the diastolic relaxation is impaired. The shape of the curve is borrowed from a paper by Zile et al they took real measurements from patients with varying degrees of diastolic dysfunction.
Now, let us see what happens when we increase preload.
Read Also: Does Acid Reflux Cause Heart Palpitations
How To Diagnose Diastolic Heart Failure
To diagnose heart failure, patients are asked questions about their medical history and undergo a physical exam. There are advanced procedures and technology involved to effectively diagnose the condition, inform treatment, and monitor the heart. Tests can include:
- Blood test: Check the levels of certain fats, cholesterol, sugar, and protein in the blood that could indicate heart problems.
- Chest X-ray: A common imaging test of the lungs, heart, and aorta.
- Echocardiogram: An ultrasound exam that uses sound waves to take moving pictures of the hearts chambers and valves.
- Electrocardiogram : Measures the electrical activity of the heart and can help determine if parts are enlarged, overworked, or damaged.
- Electrophysiology study: Records the hearts electrical activities and pathways. It can help find what is causing heart rhythm problems and identify the best treatment.
- Stress testing: Conducted during exercise. If a person cannot exercise, medicine is given to increase their heart rate. Used along with an EKG, the test can show changes in the hearts rate, rhythm, or electrical activity as well as blood pressure. Exercise makes the heart work hard and beat fast while heart tests are conducted.
