How Ultromics Helps Detect Heart Failure
The new HF guidelines highlight how effective and efficient echocardiographic left ventricular function is to guide treatment decisions for patients with heart failure. Ultromics is an AI-powered platform which can be connected through the cloud to automate LV insights, and provide reports whenever an echocardiogram is performed. The technology offers significantly improved heart failure detection by automating ejection fraction , volumes, and notably global longitudinal strain , with zero variability.
These new Heart Failure Guidelines illustrate that now, more than ever, clinicians and their patients can significantly benefit from accurate detection and earlier prevention through echocardiography. To learn more about how EchoGo is revolutionizing the way clinicians diagnose and treat HF, download our free Heart Failure Guide today.
References:
Acc Aha And Hfsa Partner To Release 2022 Heart Failure Guidelines
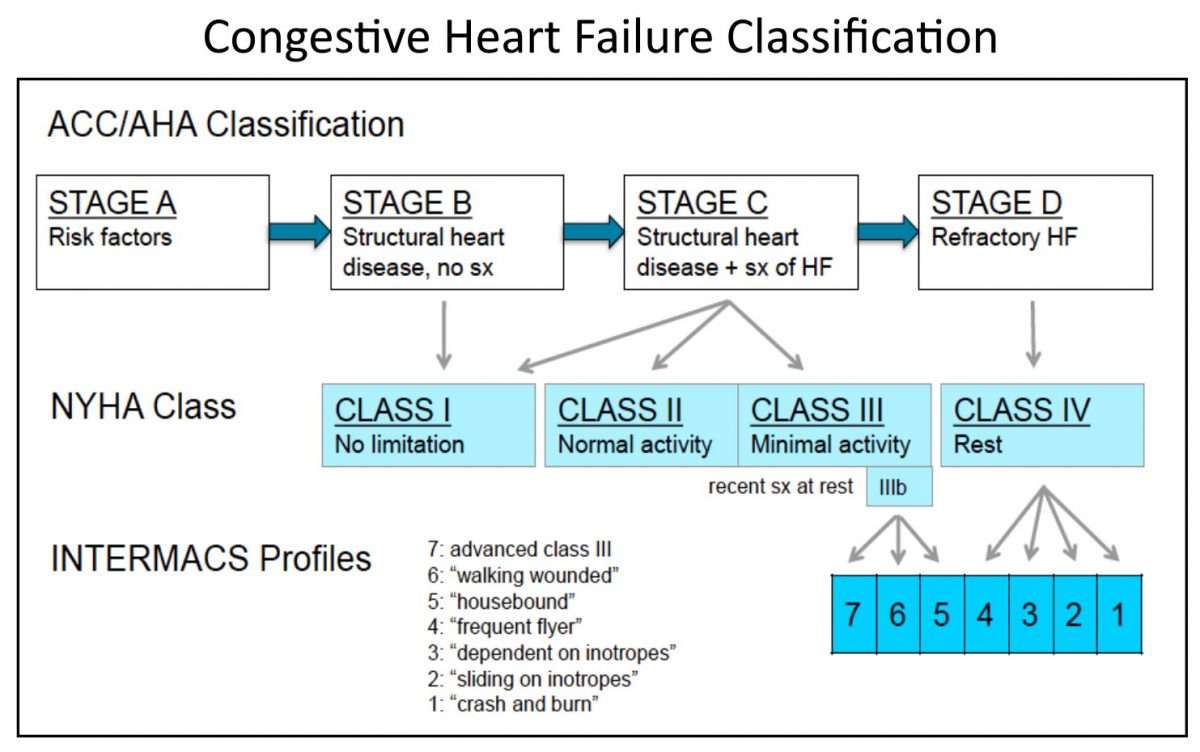
Released on the eve of ACC.22, the 2022 heart failure guidelines represent a collaborative effort by the ACC/AHA/HFSA and include major additions, including a new focus on the use of SGLT2 inhibitors and revisions to the ACC/AHA stages of heart failure.
The American College of Cardiology, American Heart Association, and Heart Failure Society of America have released a new joint guideline outlining evidence-based strategies for prevention, diagnosis, and management of heart failure.
One primary goal with the new guideline was to use recently published data to update our recommendations for the evaluation and management of heart failure, said Paul A. Heidenreich, MD, MS, guideline writing committee chair, in a statement from the American College of Cardiology. One focus was prevention of heart failure through optimizing blood pressure control and adherence to a healthy lifestyle.
Published on April 1, which is just a day prior to the start of the American College of Cardiologys 71st annual Scientific Session , the 159-page document broken down into 14 sections with multiple subsections and cites more than 700 reference documents. Composed by Heidenreich and a team of more than 50 fellow authors, the guideline is based on an evidence review of relevant studies and data published through September 2021.
New Classification Of Ejection Fraction
The updated heart failure guidelines also made changes to the four left ventricular ejection fraction classifications.
The updated levels of ejection fraction are:
- HFrEF : less than or equal to 40%
- HFimpEF : improved from less than 40% to above 40%
- HFmrEF : between 41%49%
- HFpEF : above 50% but with increased filling pressures
Also Check: Why Do Athletes Have Lower Heart Rate
Acc/aha/hfsa Guideline For The Management Of Heart Failure
On April 1, 2022, a new joint guideline for the management of heart failure was published from the American College of Cardiology, the American Heart Association, and the Heart Failure Society of America.
The 2022 ACC/AHA/HFSA Guideline for the Management of Heart Failure increases the focus on preventing HF, updates treatment strategies for people with symptomatic heart failure to include SGLT-2 inhibitor medicines and emphasizes care coordination with a heart failure specialty team. The guideline also offers recommendations for managing cardiac amyloidosis, cardio-oncology complications, comorbidities in the setting of heart failure, as well as consideration for implantable devices and advanced therapies for people with stage D heart failure.
Supplemental resources to help you apply the guidelines to your practice are available to download below.
B Vte Prophylaxis In Hospitalized Patients
Recommendation for VTE Prophylaxis in Hospitalized Patients
Referenced studies that support the recommendation are summarized in the Online Data Supplements.
| COR |
|---|
|
In patients hospitalized with HF, prophylaxis for VTE is recommended to prevent venous thromboembolic disease . |
Synopsis
HF has long been recognized as affording additional risk for venous thromboembolic disease. When patients are hospitalized for decompensated HF, or when patients with chronic stable HF are hospitalized for other reasons, they are at increased risk for venous thromboembolic disease. The risk may be associated with higher HF symptom burden . This risk may extend for up to 2 years after hospitalization but is greatest in the first 30 days . The use of anticoagulation with subcutaneous low-molecular-weight heparin, unfractionated heparin, fondaparinux, or approved DOAC are used for the prevention of clinically symptomatic deep vein thrombosis and pulmonary embolism .
Recommendation-SpecificSupportingText
| 1. |
Recommended Reading: How Low Is Too Low For Heart Rate
Heart Failure Guidelines Go
Developed for healthcare professionals who care for heart failure patients in the post-acute setting, our new Heart Failure Guidelines Go-To-Guide provides information about the latest, evidence-based heart failure treatment guidelines. The guide also includes resources that can help healthcare professionals in the post-acute setting apply the latest guidelines.
Aha/acc/hfsa Heart Failure Guidelines Emphasize Prevention
- 10th May 2022
| Professor Paul Leeson Professor of Cardiovascular Medicine at the University of Oxford and co-founder of Ultromics. |
New industry Heart Failure guidelines were published on April 01 2022, and launched at the American College of Cardiology annual session in Washington, D.C.
The update was a joint effort by experts from the American College of Cardiology , the American Heart Association , and the Heart Failure Society of America .
The new guidelines help healthcare providers treat patients who have heart failure as well as patients who are at risk for the disease.
The last full set of HF guidelines published by these societies dates back to 2013, with a focused update released in 2017. Of note, the European Society of Cardiology released its newest heart failure guidelines last fall during the ESC Congress. There are many areas of overlap between the two documents.
Professor Paul Leeson shares key takeaways from the new guidelines.
Don’t Miss: How Many Aspirin To Prevent Heart Attack
Acc Aha Hfsa 2022 Heart Failure Management Guidelines: A Guideline Topline
The new HF guidelines prioritize primary prevention, revise disease stages to encourage early intervention, and now include SGLT2i as guideline-directed medical therapy.
The new 2022 guidelines on management of heart failure reflect a unique collaboration between the American College of Cardiology, American Heart Association, and the Heart Failure Society of America.
The new recommendations retain and combine elements from guidelines published in 2013 and 2017 and, based on extensive review of new data, include important evidenc-based additions and revisions. Top among the new recommendations is a Class 2a recommendation for use of SGLT-2 inhibitors in HFpEF and revised ACC/AHA stages of heart failure.
For primary care clinicians the revised staging of heart failure reinforces a primary focus of the new guidlines on prevention of heart failure thus the new Stage A: At-risk for heart failure emphasizes early identification of and treatment to reduce risk factors that include a range of cardiometabolic disease.
The Guideline Topline that follows includes the new stages of heart failure and a quick look at the 10 topline guidlines take-home points identified by the writing committe.
ACC/AHA/HFSA Stage A: At risk for heart failure
CVD, cardiovascular disease
Classification Of Hf By Left Ventricular Ejection Fraction
LVEF is considered important in the classification of patients with HF because of differing prognosis and response to treatments and because most clinical trials select patients based on ejection fraction . RCTs with evidence of survival benefit in patients with HF have mainly enrolled patients with HF with an LVEF 35% or 40%, often labeled HF with reduced ejection fraction . In this guideline, HFrEF is defined as LVEF 40% . HF with preserved EF represents at least 50% of the population with HF, and its prevalence is increasing . HFpEF has been variably classified as LVEF > 40%, > 45%, or 50%. Because some of these patients do not have entirely normal LVEF but also do not have major reduction in systolic function, the term preserved EF has been used. In this guideline, the threshold for HFpEF is an LVEF 50% .
Table 4 Classification of HF by LVEF
| Type of HF According to LVEF | Criteria |
|---|
|
Previous LVEF 40% and a follow-up measurement of LVEF > 40% |
|
LVEF 41%49% |
|
|
Evidence of spontaneous or provokable increased LV filling pressures |
|
LVEF 50% |
|
|
Evidence of spontaneous or provokable increased LV filling pressures |
Please see Appendix 3 for suggested thresholds for structural heart disease and evidence of increased filling pressures.
HF indicates heart failure LV, left ventricular and LVEF, left ventricular ejection fraction.
Figure 3
Classification and Trajectories of HF Based on LVEF
Recommended Reading: Can Flonase Cause Heart Palpitations
New Classification And Nomenclature
The new HF classification based on left ventricular ejection fraction identifies four classes of HF, namely HF with reduced EF , HF with improved EF , HF with mildly reduced EF , and HF with preserved EF , as shown in Figure . Importantly, the evidence of spontaneous or provokable increased left ventricular filling pressures is needed to confirm a diagnosis of HFmrEF and HFpEF.
New HF classification. HFimpEF: HF with improved EF HFmrEF: HF with mildly reduced EF HFpEF: HF with preserved EF LV: left ventricle LVEF: left ventricular ejection fraction. *Evidence of spontaneous or provokable increased LV filling pressures includes elevated natriuretic peptide , invasive haemodynamic parameters and/or non-invasive measurements including LV wall thickness 12 mm, left atrial volume index 29 mL/m2, left ventricular mass index > 116/95 g/m2, relative wall thickness > 0.42, GLS, global longitudinal strain < 16%, average E/e’ 15, Septal e’ < 7 cm/s, Lateral e’ < 10 cm/s, tricuspid regurgitation velocity > 2.8 m/s, estimated pulmonary artery systolic pressure > 35 mm Hg.
Refined Heart Failure Classifications
The updated guidelines also provide new classifications for some key heart failure terms based on left ventricular ejection fraction measurements:
- HF with reduced ejection fraction includes people with LVEF 40%.
- HF with improved ejection fraction includes individuals with previous LVEF 40% and a follow-up measurement of LVEF > 40%.
- HF with mildly reduced ejection fraction includes people with LVEF 41-49% and evidence of increased LV filling pressures.
- HF with preserved ejection fraction includes individuals with LVEF 50% and evidence of increased LV filling pressures.
The ACC/AHA/HFSA recommendations breakdown treatment guidelines for each patient group in significant detail.
You May Like: How To Stop Symptoms Of Heart Attack
Organization Of The Writing Committee
The writing committee consisted of cardiologists, HF specialists, internists, interventionalists, an electrophysiologist, surgeons, a pharmacist, an advanced nurse practitioner, and 2 lay/patient representatives. The writing committee included representatives from the ACC, AHA, and Heart Failure Society of America . Appendix 1 of the present document lists writing committee members relevant RWI. For the purposes of full transparency, the writing committee members comprehensive disclosure information is available in a Supplemental Appendix.
Areas Of Focus Include:
Management strategies in stage C HF, including:
New treatment strategies in HF, including sodium-glucose cotransporter-2 inhibitors and angiotensin receptor-neprilysin inhibitors .
Management of HF and atrial fibrillation , including ablation of AF.
Management of HF and secondary MR, including MV transcatheter edge-to-edge repair.
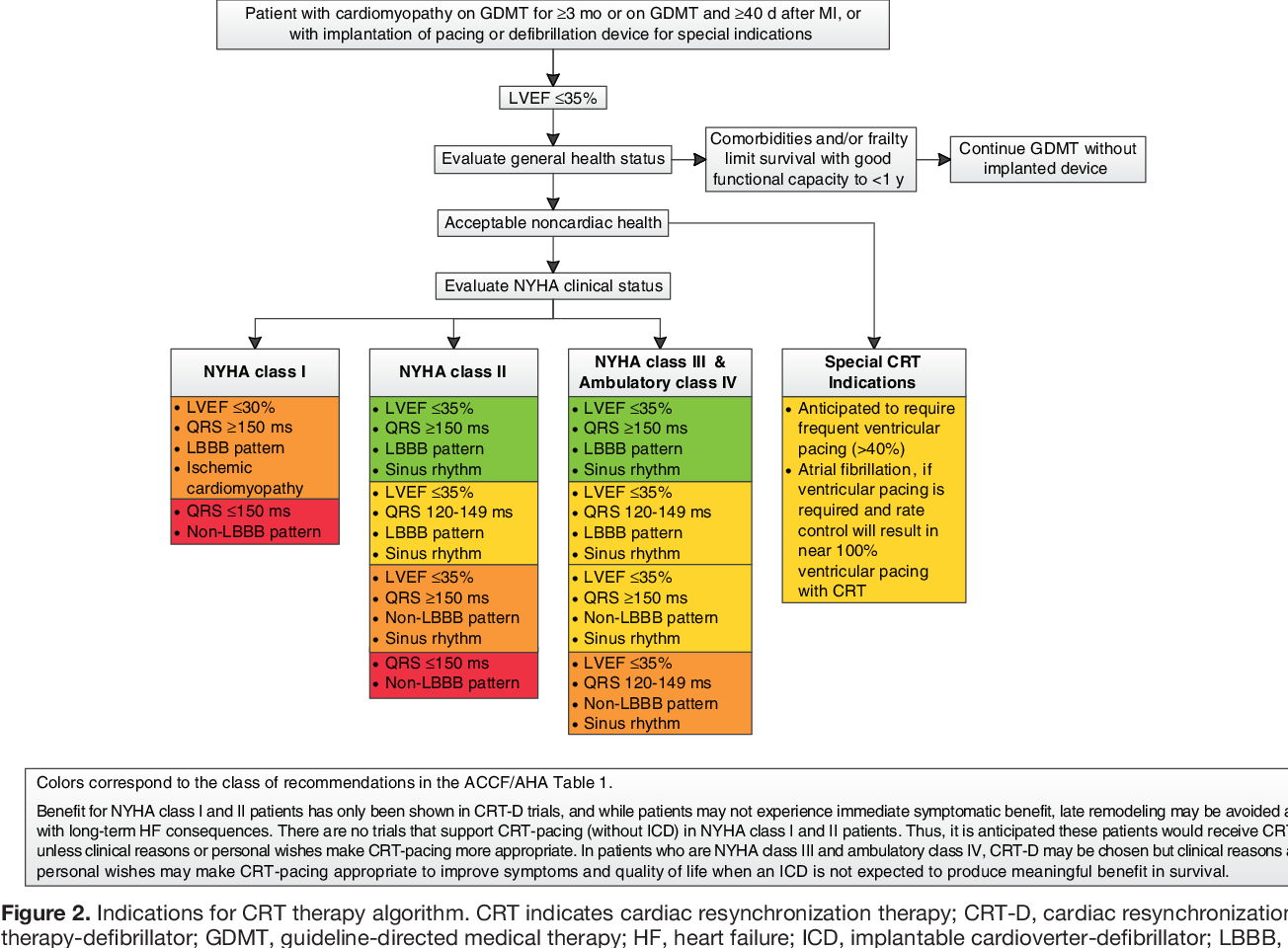
Left ventricular assist device use in stage D HF.
The intended primary target audience consists of clinicians who are involved in the care of patients with HF. Recommendations are stated in reference to the patients and their condition. The focus is to provide the most up-to-date evidence to inform the clinician during shared decision-making with the patient. Although the present document is not intended to be a procedural-based manual of recommendations that outlines the best practice for HF, there are certain practices that clinicians might use that are associated with improved clinical outcomes.
In developing the 2022 HF guideline, the writing committee reviewed previously published guidelines and related statements. Table 1 contains a list of these guidelines and statements deemed pertinent to this writing effort and is intended for use as a resource, thus obviating the need to repeat existing guideline recommendations.
Table 1 Associated Guidelines and Statements
Statements
The full SIHD guideline is from 2012 . A focused update was published in 2014 .
You May Like: Does Dehydration Cause High Heart Rate
New Acc Aha Hfsa Guidelines Recommend Sglt
The joint recommendations cite DAPA-HF and EMPEROR-HF as evidence of the drug class’ benefit for differing stages of heart failure.
The American College of Cardiology , American Heart Association and Heart Failure Society of America have released a joint guideline addressing updates to heart failure prevention and treatment of symptomatic disease with the emerging SGLT-2 inhibitor drug class.
The new guidelinepublished and presented during the ACC 2022 Scientific Sessions in Washington DCimplement findings from trials including DAPA-HF and EMPEROR-HF, which previously shown the benefit of SGLT-2 inhibitors dapagliflozin and empagliflozin, respectively, in reducing composite cardiovascular events and mortality in patients with heart failure with reduced ejection fraction among other cardiovascular and cardiometabolic outcomes.
Additionally, the guideline puts further emphasis on primary heart failure prevention through measures including blood pressure control and changes to high-risk patients diet and exercise. More than 120 million Americans currently have high blood pressure another 100 million are obese and 28 million have diabetes, meaning a significant rate of the US population can be categorized as at-risk for heart failureor Stage A, per the new guideline risk stages.
The 4 stages are as follows:
New symptomatic heart failure definitions at stage C from the guideline include:
Evidence Review And Evidence Review Committees
In developing recommendations, the writing committee uses evidence-based methodologies that are based on all available data . Literature searches focus on randomized controlled trials but also include registries, nonrandomized comparative and descriptive studies, case series, cohort studies, systematic reviews, and expert opinion. Only key references are cited.
An independent evidence review committee is commissioned when there are 1 questions deemed of utmost clinical importance and merit formal systematic review to determine which patients are most likely to benefit from a drug, device, or treatment strategy, and to what degree. Criteria for commissioning an evidence review committee and formal systematic review include absence of a current authoritative systematic review, feasibility of defining the benefit and risk in a time frame consistent with the writing of a guideline, relevance to a substantial number of patients, and likelihood that the findings can be translated into actionable recommendations. Evidence review committee members may include methodologists, epidemiologists, clinicians, and biostatisticians. Recommendations developed by the writing committee on the basis of the systematic review are marked SR.
You May Like: How To Know If You’re Having A Heart Attack Male
Acc Aha Hfsa Issue Joint Heart Failure Guideline
New ACC/AHA/HFSA guideline redefines heart failure stages to focus on prevention, updates treatment options and emphasizes care coordination with a heart failure specialty team
April 1, 2022 A new joint guideline published today from the American College of Cardiology, the American Heart Association, and the Heart Failure Society of America, increases the focus on preventing heart failure in people who are showing early signs of pre-heart failure, and updates treatment strategies for people with symptomatic heart failure to include SGLT-2 inhibitor medicines. The guideline also offers recommendations for managing cardiac amyloidosis, cardio-oncology complications, comorbidities in the setting of heart failure, as well as consideration for implantable devices and advanced therapies for people with stage D heart failure.
Heart failure is a chronic condition that is usually manageable with medication and lifestyle changes. The most common causes of heart failure include narrowed heart arteries, heart attack, high blood pressure and valvular heart disease. Other causes can include, but are not limited to, familial or genetic cardiomyopathies, amyloidosis, metabolic disease, autoimmune disorders or exposure to cardiotoxic agents, such as chemotherapy or other medications. Primary prevention is important for those at risk of HF or pre-HF.
For individuals with stage C HF, the new guideline refines the current four classifications of HF based on LVEF with new terminology:
The Stages Of Heart Failure
Another key detail from these recommendations is updated stages of heart failure. These stages include:
- Stage A: At Risk for Heart Failure. At risk, but without symptoms.
- Stage B: Pre-Heart Failure. No symptoms or signs of heart failure, but evidence of one of the following: structural heart disease, such as reduced ejection fraction, enlargement of the heart muscle, abnormalities in heart muscle contraction, or valve disease increased filling pressures as measured via ultrasound or risk factors from stage A plus increased levels of B-type natriuretic peptide or persistently elevated cardiac troponin, an indicator of heart muscle injury.
- Stage C: Symptomatic Heart Failure. Structural heart disease with current or previous symptoms of heart failure.
- Stage D: Advanced Heart Failure: Heart failure with symptoms that interfere with daily life, are difficult to control and result in recurrent hospitalizations despite continued guideline-directed medical therapy.
As the recommendations point out, more than 121 million people in the United States have high blood pressure, another 100 million are obese and 28 million have diabetes this means a large proportion of the countrys population can be viewed as a Stage A heart failure patient.
Also Check: How Do I Lower My Heart Rate
New Acc/aha/hfsa Guideline Redefines Heart Failure Stages To Focus On Prevention Updates Treatment Options And Emphasizes Care Coordination With A Heart Failure Specialty Team
Contact: Sam Roth, [email protected],
WASHINGTON and DALLAS –
A new joint guideline published today from the American College of Cardiology, the American Heart Association, and the Heart Failure Society of America, increases the focus on preventing heart failure in people who are showing early signs of pre-heart failure, and updates treatment strategies for people with symptomatic heart failure to include SGLT-2 inhibitor medicines. The guideline also offers recommendations for managing cardiac amyloidosis, cardio-oncology complications, comorbidities in the setting of heart failure, as well as consideration for implantable devices and advanced therapies for people with stage D heart failure.
Heart failure is a chronic condition that is usually manageable with medication and lifestyle changes. The most common causes of heart failure include narrowed heart arteries, heart attack, high blood pressure and valvular heart disease. Other causes can include, but are not limited to, familial or genetic cardiomyopathies, amyloidosis, metabolic disease, autoimmune disorders or exposure to cardiotoxic agents, such as chemotherapy or other medications. Primary prevention is important for those at risk of HF or pre-HF.
New York Heart Association classification is used when people reach symptomatic or advanced HF, to describe their functional capacity and determine treatment strategies.
Additional Resources:
