Determinants Of Improvement In Ejection Fraction: Previous Studies
Several studies have assessed the sequential changes in global left ventricular function during the acute, subacute, and chronic phases after myocardial infarction. Large thrombolytic trials, using contrast ventriculography or radionuclide angiography to assess ejection fraction, have shown no overall change in global ejection fraction during the first weeks after thrombolytic treatment. Improvement in regional infarct zone function is often counteracted by a decrease in non-infarct zone hyperkinesia. However, despite the absence of large group changes, there is considerable individual improvement.
One of the most important determinants of improvement in the ejection fraction appears to be sustained successful reperfusion. Harrison and colleagues carried out early and one week catheterisations in 542 patients treated with intravenous thrombolysis for acute myocardial infarction: acute TIMI grade 3 flow in the infarct related artery was independently associated with improvement in the left ventricular ejection fraction at one week. Meijer and colleagues showed an increase in the ejection fraction from 51 % within 48 hours after thrombolysis to 55 % after three months in 95 patients with sustained reperfusion, compared with no change in 34 patients with reocclusion of the infarct related artery.
How Ubiquinol Can Benefit Americas Heart Health
Lipid-soluble Ubiquinol is easily available as an oral supplement and has been shown to effectively replace levels of CoQ10 that have been depleted as a result of statin medications. Statin users should be aware that taking CoQ10 in its non-reduced form is not the best solution because the body is often unable to convert CoQ10 into Ubiquinol. Ubiquinol, however, is the active, antioxidant form that can easily be absorbed by the body and is ready to be used by cells.
In addition to having that glass of wine at dinner, going for a run and cutting back on unhealthy foods, supplemental doses of Ubiquinol can go a long way toward supporting Americas heart health. Ubiquinol is available over-the-counter at nearly every pharmacy and is often found on the same shelves as conventional CoQ10 supplements. Beginning as early as 30, when the bodys ability to convert conventional CoQ10 into the active Ubiquinol form may diminish, just about everyone can benefit from taking a Ubiquinol supplement. As age increases, so too can beneficial Ubiquinol intake. If you over 40 or are dealing with a health condition, your bodys ability to produce CoQ10and convert it to Ubiquinolmay be compromised. For the 25 percent of American men and women who are reaping the benefits of statin medication, the unintended consequence of decreased CoQ10 levels can be safely and easily remedied by a couple hundred milligrams of Ubiquinol per day.
Know Your Sodium Limits And Regulate Fluids
- Check your sodium intake. The average American consumes about 3,400 milligrams of sodium per day, which can result in the body holding excess fluids and create an added strain on the heart.
- Follow your sodium recommendations. For most patients with heart failure, the AHA recommendations of no more than 1,500 milligrams of sodium per day are appropriate, but your treatment plan may have an alternate recommendation. Read labels and follow your treatment plan carefully.
- Discover ways to help you reduce sodium in your diet.
Don’t Miss: Reflux And Palpitations
If You Have Fluid Retention
Diuretics. Diuretics such as furosemide and torsemide help the body eliminate excess fluid that can cause swelling or shortness of breath. Although the reasons why heart disease impairs the body’s ability to maintain fluid balance are complex, most people who require a diuretic need it indefinitely. “This is one of the most important drugs to individualize, since the optimal dose can vary from 10 milligrams to 400 mg a day, depending on how well the kidneys are working,” says Dr. Stevenson.
How To Train After A Heart Attack
Now we know that you shouldnt wait for a long time after a heart attack before exercising. But should you be taking it easy with your clients? Should you use a lower intensity?
The answer quite clearly is no. A higher intensity is actually required to have the beneficial effects on the heart. Translation: just going for a leisurely walk is not good enough .
One study compared two exercise intensities: moderate intensity , and high intensity . What they found was that high intensity improved their cardiovascular fitness more than moderate intensity. But, this was more than one week after a heart attack.
In the initial period after a heart attack , its better to do low to moderate intensity exercise and over time raise the intensity.
What about strength training? Thats what this study wanted to find out should you just do cardio after a heart attack, or should you also do strength training? To answer that question, researchers divided participants into two groups:
- Group 1: only cardio, at 65-85% of maximal heart rate
- Group 2: cardio plus strength training
The results: the group that did cardio AND strength training had improved ejection fractions. The group that did only cardio did not improve ejection fraction.
The frequency recommended by the American College of Sports Medicine is at least times per week.
In summary, exercise prescription after a heart attack is as follows:
You May Like: Does Acid Reflux Cause Heart Palpitations
Useful In Specific Cases
Cardiac resynchronization therapy . Sometimes called biventricular pacing, CRT is very useful in hearts with a specific electrical pattern that indicates poorly coordinated contractions of the left and right sides of the heart, which may worsen heart failure symptoms. CRT synchronizes the contractions of the right and left ventricles for optimal pumping power. CRT has a modest effect on survival, decreases hospitalizations, and greatly increases quality of life for these people. “This device-based therapy is truly a remarkable step forward, and the only therapy we can offer that makes more than half of patients feel better almost immediately,” says Dr. Stevenson.
Low Ejection Fraction Diagnosis
With advanced technology in labs that are among the best-equipped in the country, well use one or more imaging tests to precisely measure your ejection fraction. These tests may include:
- Radiographic imaging, such as a CT scan or MRI
- Echocardiogram, a heart ultrasound
- Nuclear cardiology imaging, which uses a safe dose of radioactive material to evaluate blood flow through your heart
- Cardiac catheterization, a minimally invasive procedure where we gently guide a thin tube, or catheter, with a tiny camera through a blood vessel to your heart
Find out more about our heart and vascular testing and diagnosis.
Recommended Reading: How Much Blood Does The Heart Pump
Improve Ejection Fraction Of Heart
Ask U.S. doctors your own question and get educational, text answers â it’s anonymous and free!
Ask U.S. doctors your own question and get educational, text answers â it’s anonymous and free!
HealthTap doctors are based in the U.S., board certified, and available by text or video.
What Causes High Ejection Fraction
Ejection fraction of 75% or more can indicate a heart condition such as hypertrophic cardiomyopathy. Hypertrophic cardiomyopathy occurs if heart muscle cells enlarge and cause the walls of the ventricles to thicken. The ventricle size often remains normal, but the thickening may block blood flow out of the ventricle. If this happens, the condition is called obstructive hypertrophic cardiomyopathy.
Hypertrophic cardiomyopathy is very common and can affect people of any age. If effects men and women equally. It is a common cause of sudden cardiac arrest in young people, including athletes.
Recommended Reading: Can Flonase Cause Heart Palpitations
What Happens With Heart Failure
The term Heart Failure suggests that the heart has stopped working or has failed. This is not the case. What it actually means is that the heart is not working as well as it should, and cannot pump enough blood to meet the bodys needs.
This happens because the heart is weakened by conditions or diseases that damage the heart muscle. Most of these conditions weaken the heart little by little, over a period of time.
What Are The Treatment Options For Abnormal Ef
There are a variety of treatment options for abnormal EF, including:
- Angiotensin converting enzyme inhibitors, angiotensin II receptor blockers , or beta-blockers. These medications can reduce the amount of hormones that weaken your heart muscle. They can also slow the progression of heart disease.
- Diuretics. These drugs can help get rid of excess fluid thats causing swelling and shortness of breath.
- Eplerenone or spironolactone. These agents help you eliminate excess fluid and can help decrease stiffening of your heart.
- Biventricular pacemaker. This pacemaker helps to synchronize the contractions of your left and right ventricles so theyre working to their highest capacity.
- Implantable cardiac defibrillator. This device can be directly implanted into your chest. It sends small electrical triggers to your heart to keep it beating regularly.
- Hydralazine-nitrate. These two drugs have been successful in lowering blood pressure in people who still have symptoms when taking ACE, ARBs, and beta-blockers.
You May Like: Does Tylenol Increase Heart Rate
What Causes Heart Failure
Cardiomyopathy is the general term for a heart that is enlarged or damaged by one of several diseases. Cardiomyopathy can be caused by coronary artery disease, valvular heart disease, viral or bacterial infections that attack the heart, drugs that damage the heart muscle, prolonged alcohol abuse, some metabolic diseases, as well as other causes.
Coronary Artery Disease is the most common cause of Heart Failure. CAD is a narrowing of the arteries that supply blood to the heart muscle. Cholesterol deposits clog the arteries, decreasing the supply of blood and oxygen to the heart. This can weaken the heart muscle. Opening the arteries may improve Heart Failure. CAD can result in a myocardial infarction or heart attack. A heart attack occurs when plaque and clotting cause a complete blockage in a coronary artery. The heart muscle that was receiving blood from the blocked artery dies, causing permanent muscle damage. An enlarged heart from CAD or from a prior heart attack may be referred to as ischemic cardiomyopathy. Six out of every seven patients hospitalized with Heart Failure have a history of coronary artery disease, and three out of four have a history of high blood pressure.
Other conditions some of which are temporary and treatable, can cause Heart Failure. These include:
- Arrhythmias
- Thyroid disease
- Unknown causes
Recognizing Depression And Anxiety
Everyone feels anxious or blue some of the time. But if these feelings persist and they interfere with your ability to do and enjoy daily activities, or if your relationships are affected, you should seek help. People who are depressed often feel tired and have no energy. They may lose interest in sex, have trouble sleeping and lose their appetite. Although fatigue and loss of appetite are also common symptoms of Heart Failure, they are more likely due to depression if accompanied by any of the symptoms listed on the next page. You may be depressed if you have any of the following symptoms for more than 2 weeks:
- Excessive sleepiness
- Feeling keyed up or always on edge
- Restlessness
- Feeling shaky
Many people in our society feel there is some stigma associated with having emotional problems like depression or anxiety. As a result, they may be reluctant to talk to anyone about how they are feeling. However, having emotional problems is nothing to be ashamed about. It is important to recognize and treat depression and anxiety. If you are having difficulty coping with feelings about Heart Failure, you should seek help and support. In other words, if depression and anxiety are interfering with your life or causing distress, it is important for you to seek help from your doctor or nurse.
You May Like: Can Acid Reflux Cause Palpitations
Heart Disease In Canada
- About one in 12 Canadians lives with heart disease. Chances are you either currently have, or at one point will have a client with heart disease.
- Every five minutes, one Canadian with heart disease will die. This is where we shine as fitness professionals because much of heart. disease is preventable with a combination of exercise, proper nutrition, and sleep.
- Of the people who are at risk for heart disease, 49% are at whats considered to be high risk the vast majority of those are over 40.
Fortunately, as fitness professionals, we can help prevent heart attacks with exercise and lifestyle modifications.
Phenotyping Hfmref Beyond Ef
Owing to the limitations of the EF construct and measurement, numerous alternative methods are advocated for and are emerging to phenotype HF. Myocardial tissue characterization by cardiac MRI is part of the routine diagnostic work-up in patients with HF of unknown aetiology. Emerging studies also highlight the importance of cardiac MRI in patients with EF > 40%,,. Late gadolinium enhancement is known to be a major prognostic marker and a validated predictor of SCD and life-threatening arrhythmias in HFrEF. However, LGE also correctly classifies the risk of death and SCD in patients with mild-to-moderate reduction in EF,, and therefore could be considered to identify patients at increased risk of SCD who are suitable for trials that test strategies for primary prevention of SCD regardless of the EF.
The assessment of myocardial strain and in particular global longitudinal strain from speckle-tracking analysis of 2D echocardiography is an emerging technique complementary to EF for the quantification of systolic and diastolic ventricular and atrial function,. Measurement of GLS has revealed how systolic dysfunction can be present even if the EF is preserved or normal,. Large observational studies and meta-analyses also support an incremental and independent role for GLS beyond EF in terms of mortality prediction in patients with EF > 35%,.
Also Check: Which Of The Following Signs Is Commonly Observed In Patients With Right-sided Heart Failure
Clinical Characteristics Of Hfmref
Proper characterization and phenotyping of HFmrEF is important because it might support treatment recommendations based on available data and inform the design of future interventional trials in HFmrEF by facilitating appropriate trial selection criteria. HFmrEF is often defined as intermediate because this classification makes intuitive sense, or as a milder form of HFrEF because of some distinct clinical and treatment response similarities to HFrEF. Both of these approaches are overly simplistic and ignore the extensive emerging research that characterizes HFmrEF in detail in relation to HFrEF and HFpEF. Figure provides a conceptual representation of HFmrEF in relation to HFrEF and HFpEF, and Figs , provide detailed characteristics from specific data sets.
Fig. 1: Phenotype, risk of cause-specific outcomes and effect of therapies in HFrEF, HFmrEF and HFpEF.
Previous research has also assessed the degree of neurohormonal activation across the EF spectrum, showing higher circulating neurohormone levels in patients with HFrEF than in those with HFmrEF or HFpEF,,. The higher neurohormonal activation in HFrEF might reflect the greater HF severity and be a marker of higher rates of cardiovascular events in patients with HFrEF than in patients with HFmrEF or HFpEF, as well as the observed efficacy of neurohormonal inhibition in patients with HFrEF, and potentially in those with HFmrEF, but not in patients with HFpEF ,,.
How Is Heart Failure Diagnosed
To make the diagnosis of Heart Failure the following should be done:
- Health History.
- Physical Exam.
- Chest X-Rayto evaluate the size and shape of the heart and detect any fluid in the lungs.
- EKGto determine heart rhythm and search for previous heart damage or thickened heart muscle.
- Blood Test for BNPa hormone made when the heart is overworked.
- Measure Ejection Fraction to gauge effectiveness of the pumping action of the heart. The EF can be determined with an echocardiogram, nuclear scan or angiogram.
Also Check: Acetaminophen Heart Rate
Investigators Tried To Better Characterize The Prevalence Predictors And Prognosis Of Patients With Recovered Ejection Fraction
While some patients are able to recover left ventricular ejection fraction after initially being diagnosed with heart failure with LVEF below 40%1, it has been largely unclear how this translates into clinical outcomes. To help close this gap in knowledge, Ghimire and colleagues conducted a retrospective study with a real-world cohort of patients with HF to better characterize the prevalence, predictors, and prognosis of patients with recovered ejection fraction . Their study was recently published in European Heart Journal. 1
Take Note
- Earlier studies of heart failure with reduced ejection fraction may have exhibited selection bias.
- This study included a broader spectrum of patients in an effort to better examine the prevalence, predictors, and prognosis of patients with recovered ejection fraction .
- HFrecEF patients tended to be younger, female and more likely to have hypertension, AF, or cancer. HFrecEF patients had a better prognosis than those with persistent HFrEF, and female patients had a lower mortality risk in each subgroup.
The study by Ghimire et al analyzed patients over age 18 with a physician-assigned diagnosis of HF referred to the 2 largest echocardiography centers in Alberta, Canada, between April 1, 2008, and March 31, 2016, and who underwent 2 echocardiograms separated by 6 months . A total of 10,641 patients with a diagnosis of HF who had objective measurement of their LVEF on both echocardiograms were included.
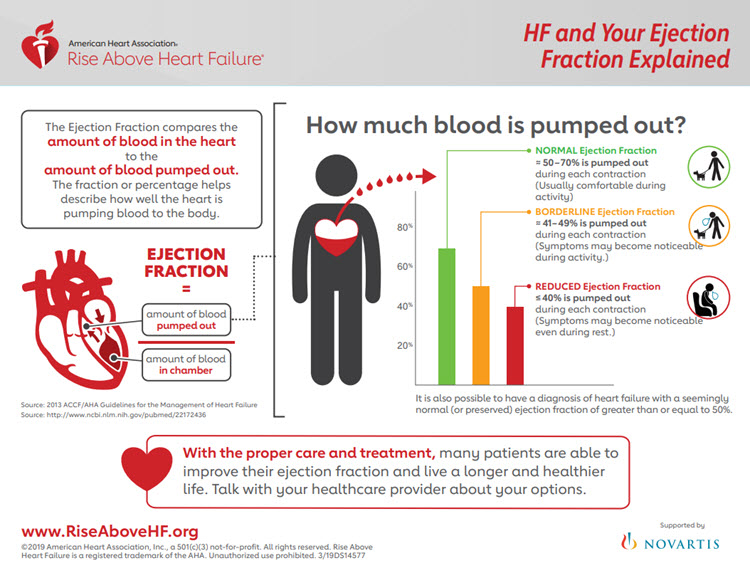
Ejection Fraction And Its Importance
Ejection Fraction is a key indicator of a healthy heart and is frequently used by physicians to determine how well your heart is functioning as a pump. Ejection fraction is the percentage of blood that is pumped out of the heart during each beat. In a healthy heart, 50-75 percent of the blood is pumped out during each beat. Many people with heart disease pump out less than 50% and many people with Heart Failure pump out less than 40%.
Ejection Fraction is one of the many ways doctors classify the type and severity of Heart Failure and damage to the heart muscle.
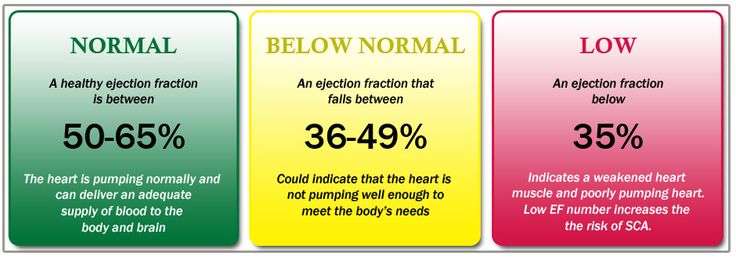
Ejection Fraction ranges
- An Ejection Fraction above 50% indicates that your heart is pumping normally and is able to deliver an adequate supply of blood to your body and brain.
- An Ejection Fraction that falls below 50% could indicate that the heart is no longer pumping efficiently and is not able to meet the bodys needs.
- An Ejection Fraction of 35% or less indicates a weakened heart muscle. The heart is pumping poorly, which can significantly increase a persons risk for sudden cardiac arrest.
Measuring your Ejection Fraction
For Heart Failure patients, knowing your ejection fraction is just as important as knowing your blood pressure and your cholesterol. Ejection fraction is often measured using an echocardiogram, a simple and painless test often performed right in the doctors office. Ejection faction can also be measured with other tests including:
- Echocardiography
- Nuclear stress testing
Recommended Reading: List The Steps Of How To Calculate Your Target Heart Rate Zone
