Increase In Arterial Blood Pressure
NSAIDs can cause sodium and water retention, as well as reduce formation of the vasodilator prostacyclin in the vessel wall. The risk of increased blood pressure during treatment with NSAIDs has long been known. This side effect seems to be present in all NSAIDs except low dose ASA, although some NSAIDs appear to be safer than others . According to a meta-analysis by Johson, et al. , analgesics from the group of NSAIDs lead to an elevation in mean blood pressure by 5 mmHg, but in this study, the increase in blood pressure reached the level of statistical significance only in the subgroup with medically controlled hypertension.
The blood pressure increasing effect is present also in the case of selective COX-2 inhibitors. According to a meta-analysis by Chan, et al. , the risk of blood pressure increase is higher with coxibs than with non-selective NSAIDs . The same study highlighted the differences between various coxibs. Significant increases in blood pressure were found with rofecoxib and etoricoxib, while the effect of celecoxib on blood pressure appeared to be minimal.
Could Prescribed Nsaids Raise Heart Failure Risk
Study of millions of health records suggests an association, but can’t prove cause-and-effect
HealthDay Reporter
WEDNESDAY, Sept. 28, 2016 — Use of prescription-strength ibuprofen, naproxen and other commonly used pain relievers may be tied to a higher risk of heart failure, researchers report.
Medicines like these fall into a category of painkillers known as non-steroidal anti-inflammatory drugs . These medications may raise a person’s relative risk of heart failure by nearly 20 percent, according to the analysis of medical records for nearly 10 million patients.
That risk increases with the amount of NSAIDs a person is taking, said study author Andrea Arfe, a Ph.D. student at University of Milano-Bicocca, in Italy.
A person’s risk of hospitalization for heart failure doubles for some NSAIDs used at very high doses, including diclofenac , etoricoxib , indomethacin , and piroxicam , Arfe said.
Also, “our findings — which focused only on prescription NSAIDs — might apply to over-the-counter NSAIDs as well,” Arfe said. “Although over-the-counter NSAIDs are typically used at lower doses and for shorter durations, they are sometimes available at the same doses as prescription NSAIDs and they may be inappropriately overused.”
Still, the nature of the study can only point to an association between NSAID use and heart failure risk — it can’t prove cause-and-effect. And one expert believes that most patients who need an NSAID for their pain can safely continue using the drugs.
Recent Cardiovascular Safety Studies
Since the MARC previously discussed the cardiovascular safety of diclofenac in 20131 and ibuprofen in 20152, several new studies on the cardiovascular safety of NSAIDs have been published.
Medsafe presented a report on the recent literature to the MARC at the 177th meeting on March 20193. These studies include two key clinical trials4,5, and two large observational studies using healthcare databases6,7. In addition, there have been two meta-analyses of older studies8,9, a Danish healthcare registry study examining the risk of out-of-hospital cardiac arrest with NSAIDs10, and a case-control study nested in a cohort derived from European electronic healthcare databases that examines the risk of hospital admission for heart failure exacerbation in new users of NSAIDs11.
The MARC reviewed these studies and concluded that it is currently not possible to differentiate NSAIDs by their individual cardiovascular risk profiles12. All NSAIDs increase cardiovascular risk, and the risk is increased with both short-term and long-term use.
Also Check: Can Panic Attacks Mimic Heart Attacks
Nsaids And Heart Failure
Last reviewed 01/2018
- there is evidence that people with heart failure who took NSAIDs were at substantially greater risk of death or being admitted to hospital for treatment of heart failure or MI, than non-users
- risk was greater with higher doses, and diclofenac was associated with a particularly high risk
Reference:
Nsaids And The Risk Of Heart Problems And Stroke
NSAIDs may increase your risk of stroke and heart disease. Here’s what you should know.
Evidence has emerged in recent years indicating that non-steroidal anti-inflammatory drugs increase the risk of heart attacks, strokes and other heart problems. You may be familiar with traditional ones such as ibuprofen , naproxen , diclofenac as well as, the selective COX-2 inhibitor celecoxib . They are widely used to treat arthritis because they help relieve pain and reduce inflammation.
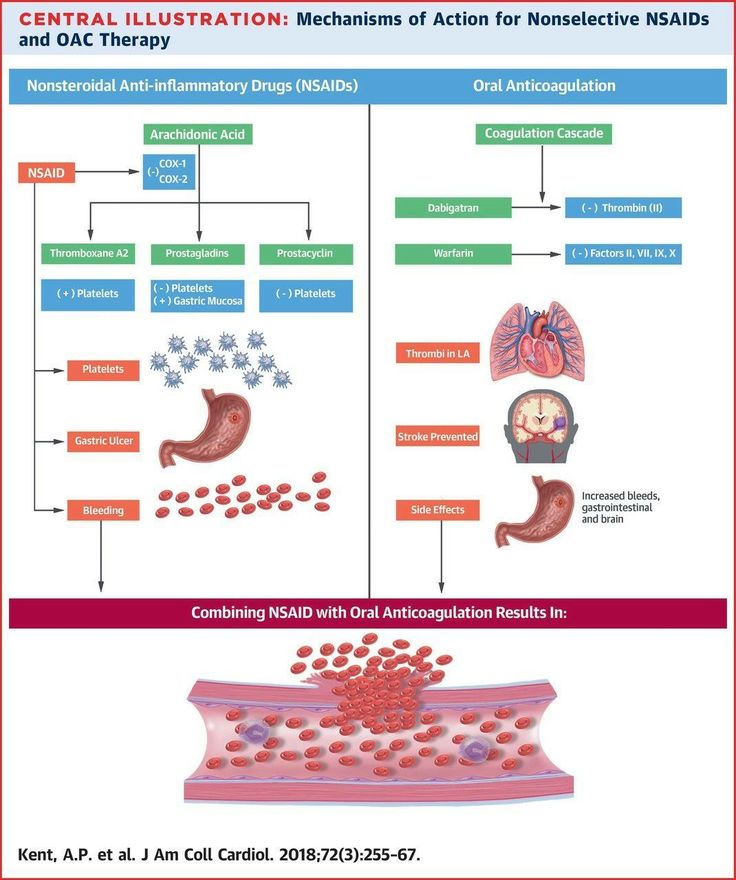
How NSAIDs Work
All NSAIDs work by blocking hormone-like substances called prostaglandins, which are involved in pain and inflammation as well as many other bodily functions, including protecting the stomach lining from its own digestive fluids. Traditional NSAIDs block prostaglandins by inhibiting two enzymes COX-1, which plays a role in stomach protection, and COX-2, which is responsible for pain and inflammation. The newer celecoxib blocks only the COX-2 enzyme, making it is less likely to cause damage to the stomach.
Studies Show NSAIDs Affect the Heart
Since 2001, several studies including one from 2011 inBMJand a 2013 review inThe Lancet have linked long-term, high-dose NSAID use to a greater risk for heart attack, stroke, heart failure and death from cardiovascular disease. In 2004, the very popular selective COX-2 inhibitor Vioxx was pulled from the market over concerns about an increased risk of heart attacks and stroke.
Considering NSAID Risks and Arthritis Pain
Hello,
You May Like: How To Improve Heart Rate Variability
When To Seek Medical Attention
If you are taking NSAIDs and feel any new signs or symptoms such as fatigue, dizziness, headache, shortness of breath, or belly, chest, or back pain, you may be experiencing a medical complication from your NSAID use. You should seek immediate medical attention, even if you do not feel that your symptoms are life-threatening.
If you experience any of the following symptoms, whether you have been taking NSAIDs or not, you could be having a heart attack or stroke. Call an ambulance or have someone take you to the emergency room immediately if you experience:
- New or worsening chest pain
- Have chest discomfort that feels like someone is sitting on your chest
- Sudden slurred speech
- Weakness in one part or side of the body
Nsaid Use Linked To Increased Heart Failure Risk In Type 2 Diabetes
Short-term use of nonsteroidal anti-inflammatory drugs could increase the likelihood of experiencing a first-time heart failure hospitalization among patients with type 2 diabetes, according to a new study presented at the European Society of Cardiology Congress 2022.
With NSAIDs, including ibuprofen, among the most commonly used medications, results of the study, which indicate use was associated with a more than 40% increase in the likelihood of a first-time heart failure hospitalization, raise a red flag related to use of these agents in patients with type 2 diabetes.
In our study, approximately one in six patients with type 2 diabetes claimed at least one NSAID prescription within one year, said lead investigator Anders Holt, MD, of Copenhagen University Hospital, Denmark, in a statement from the ESC. In general, we always recommend that patients consult their doctor before starting a new medication, and with results from this study we hope to help doctors mitigate risk if prescribing NSAIDs.
This study, Risk of Heart Failure Following Short-Term Non-Steroidal Anti-Inflammatory Drug Use in Patients with Type 2 Diabetes, was presented at ESC Congress 2022.
Related Content:
Don’t Miss: How To Not Have A Heart Attack
Nsaids And Adverse Effects
As with any medication, NSAIDs are not without adverse effects. The most commonly experienced side effects are nausea, vomiting, diarrhea, constipation, decreased appetite, rash, dizziness, headache, and drowsiness. The more severe side effects seen with NSAID use are fluid retention, renal failure , liver failure, gastric ulcers, and increased or prolonged bleeding following an injury or surgical procedure.1,3
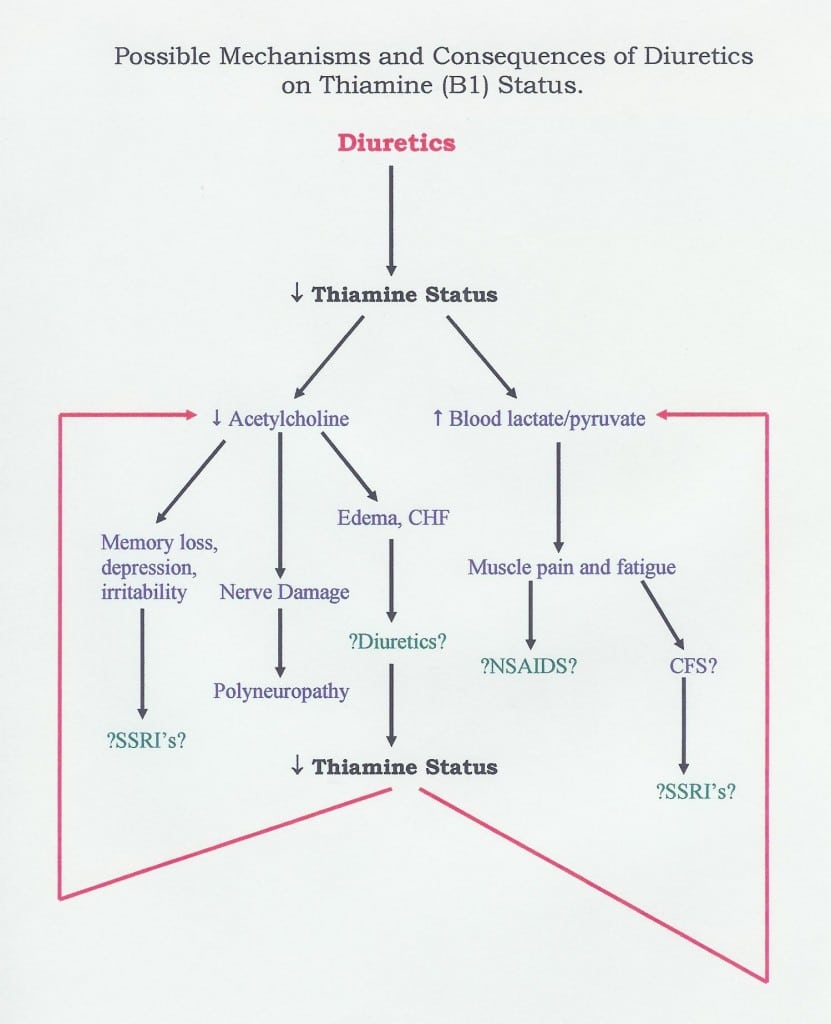
Many of the adverse effects associated with NSAID use can be explained by their effect on phospholipid metabolism. Membrane phospholipids are broken down by phospholipase A2 to arachidonic acid, the substrate for the COX enzymes. COX-1 is constitutively expressed in the stomach, kidneys, and intestinal endothelium, where it leads to vasoconstriction and platelet aggregation. COX-2 is upregulated during times of inflammation, where it causes vasodilation and inflammation via the migration of macrophages, leukocytes, and fibroblasts. It is this balance between the two enzymes that is ultimately disrupted upon administration of NSAIDs .1,4
On the other end of the spectrum, irreversible COX-1 inhibition has been shown to be cardioprotective, which is apparent with low-dose aspirin. Nonselective NSAIDs inhibit both COX-2 and COX-1. Because COX selectivity varies among the nonselective NSAIDs, so will the NSAID-associated cardiovascular risk.1,4
What This Study Tells Us
The recent meta-analysis indicates that there is no difference between NSAIDs or celecoxib regarding the risk of myocardial infarction.
Consistent with previous analyses, high doses were associated with greater risk of cardiac events. For example, no risk of cardiac events was found with low dose of ibuprofen2.
Although there is small increased risk of cardiac events associated with NSAID use, the benefit outweighs the risk of harm when used according to the instructions in the data sheet.
The MARC has previously recommended that the lowest possible dose of NSAID for the shortest period of time should be used and long-term treatment with NSAIDs should be reviewed regularly 3.
Individual risk factors should be taken into account before prescribing a NSAID and the patient should be advised of the risk of harm.
Recommended Reading: How Do You Find Your Max Heart Rate
What The Researchers Found
As shown in the Table below, compared with placebo,
- coxibs and diclofenac increased major vascular events, major coronary events, and vascular death. For 1,000 people prescribed a coxib or diclofenac for 1 year, 3 more had major vascular events, 1 of which was fatal.
- ibuprofen increased coronary events.
- all NSAIDS roughly doubled the risk of heart failure. For 1000 people taking coxibs for 1 year, 4 more had heart failure.
- all NSAIDS increased GI complications. For 1000 people taking coxibs for 1 year, 3 more had GI complications.
Nsaids: How Dangerous Are They For Your Heart
- By Christian Ruff, MD, MPH, Contributor
Nonsteroidal anti-inflammatory drugs, commonly referred to as NSAIDs, are one of the most common medications used to treat pain and inflammation. Ibuprofen, naproxen, indomethacin, and other NSAIDs are effective across a variety of common conditions, from acute musculoskeletal pain to chronic arthritis. They work by blocking specific proteins, called COX enzymes. This results in the reduction of prostaglandins, which play a key role in pain and inflammation. There are two types of NSAIDs: nonselective NSAIDs and COX-2 selective NSAIDs .
There is a growing body of evidence that NSAIDs may increase the risk of harmful cardiovascular events including heart attack, stroke, heart failure, and atrial fibrillation. Given the widespread use of NSAIDs, these findings have generated significant concern among patients and healthcare providers. I am frequently asked by patients: is it safe to continue to take NSAIDs?
Read Also: Leaky Heart Valve Surgery
Current Guideline And The Use Of Nsaids
In 1986, The World Health Organization developed the analgesic ladder for the treatment of cancer pain with the three-step sequential approach for pain medication administration depending on the severity of pain. NSAIDs are considered group one medications, recommended for mild pain and are the first step in treating pain . They are commonly prescribed in the setting of acute pain, such as acute musculoskeletal injury. In addition, they are also commonly used in the setting of arthritic pain and exceed the analgesic effects of acetaminophen, because of their anti-inflammatory effects .
Professional societies, including American Geriatric Society, American College of Rheumatology, and the European League Against Rheumatism, recommend using NSAIDs with caution and limit their use to the lowest effective dose and shortest duration. They recommend that, when used, common gastrointestinal, renal and cardiovascular side effects should be routinely monitored . Considering this recommendation, the prevalence of inappropriate use of NSAIDs is concerning. In 2015, Ussai et al., did a retrospective study of 3,050 subjects with chronic pain. They found that 97% of chronic pain subjects took NSAIDs for more than 21 consecutive days.
Nsaid Use And Heart Failure Risk
A total of 16081 cases and 1193537 matched controls were current users of NSAIDs. Figure 1 reports the distribution of current use of individual NSAIDs among all cases and controls. Among controls, the most frequently used traditional NSAIDs were diclofenac , nimesulide , and ibuprofen , while the most frequently used COX 2 inhibitors were celecoxib , rofecoxib , and etoricoxib .
Fig 1 Distribution of current use of individual NSAIDs among cases and controls and pooled associations between current use of individual NSAIDs and risk of hospital admission for heart failure, with past use of any NSAID as reference. Estimates obtained by pooling individual data from all available databases. Pooled odds ratios and 95% confidence intervals estimated by fitting a conditional logistic regression model after correcting for available covariates
Don’t Miss: Congestive Heart Failure Chf
Nsaids And Gastrointestinal Adverse Effects
Aging itself can increase risk of GI bleeding . It is known that GI bleeding and ulceration from NSAIDs use increase in severity and frequency with increasing age . NSAID use increases the risk of GI bleeding in the elderly four folds . The mechanism underlying NSAIDs induced GI adverse effects lies in the fact that these medications inhibit prostaglandin synthesis, causing weakening of the protective GI mucosal barrier, predisposing one to bleeding.
NSAIDs-induced gastroduodenal ulcers can be prevented by the use of GI protective agents, such as, Misoprostol, H2-receptor antagonists or proton pump inhibitors . This strategy is used in approximately 20% of elderly patients who are on chronic NSAIDs . Another strategy to minimize GI adverse effects is to substitute nonselective NSAIDs with COX-2 selective NSAIDs. Multiple studies have revealed that COX-2 inhibitors, such as lumiracoxib, celecoxib, and rofecoxib, caused less damage to GI mucosa compared to non-selective NSAIDs . Rhame et al. confirmed these findings when they studied elderly patients on low-dose aspirin. They found that celecoxib has superior GI safety profile, compared with non-selective NSAIDs .
However, there are increase risks of cardiovascular adverse effects with the use of COX-2 inhibitors . Thus, tailoring a patients GI risk factors versus cardiovascular risk factors is necessary to determine the choice of GI protection options for patients on chronic NSAIDs .
Nsaids And Cardiovascular Adverse Effects
Since rofecoxib and valdecoxib, were withdrawn from market in 2004 and 2005 respectively, due to adverse cardiovascular events such as edema, myocardial infarction, thrombotic events, stroke and hypertension, concerns regarding all COX-2 inhibitors potential for cardiovascular adverse effects have been raised .
Page et al. conducted a case-control study in elderly patients who were first hospitalized with congestive heart failure. They compared NSAIDs user and non- user. The use of NSAIDs was associated with increased risk of first hospital admission due to congestive heart failure .
Thus, all NSAIDs may be associated with increased cardiovascular adverse effects and each medications risk/benefit profile should be considered before prescribing to individual patients .
Also Check: Why Is My Heart Rate Always High
Fda Strengthens Warning That Nsaids Increase Heart Attack And Stroke Risk
- By Gregory Curfman, MD, Assistant Professor of Medicine, Former Editor-in-Chief, Harvard Health Publishing
Back in 2005, the FDA warned that taking nonsteroidal anti-inflammatory drugs like ibuprofen and naproxen increased the risk of having a heart attack or stroke. In July 2015the FDA took the unusual step of further strengthening this warning. This was done on the advice of an expert panel that reviewed additional information about NSAIDs and their risks. Because ibuprofen and naproxen are available over-the-counter and so widely used, its important to be aware of the ibuprofen warnings and naproxen warnings and to take steps to limit the risk.
Many people take NSAIDs to relieve mild to moderate pain. These medications may be particularly effective in conditions in which pain results primarily from inflammation, such as arthritis or athletic injury. While you can buy ibuprofen and naproxen on your own, doctors commonly write prescriptions for celecoxib , diclofenac and other NSAIDs. Aspirin is also an NSAID, but it does not pose a risk of heart attack or stroke. In fact, aspirin is commonly used to prevent heart attacks and strokes. So, it is not covered by this warning.
The FDA has noted the following ibuprofen warnings and naproxen warnings along with similar risks of other NSAIDs:
American Heart Association Stance
In 2007, the American Heart Association addressed the concern that selective COX-2 inhibition may potentiate a cardiovascular event in patients who are at an increased risk. The AHA states that physicians and patients must weigh the risks and benefits of each agent before choosing a treatment plan for pain relief. Patients should be treated only for the shortest amount of time and with the lowest dosage of drug necessary to gain symptom relief.13,17
A stepwise approach is suggested, beginning with the agents that have the lowest associated cardiovascular risk and moving to the agents with higher risk if treatment failure occurs. Non-NSAID products, such as acetaminophen or nonacetylated salicylates, are the preferred agents in patients with high cardiovascular risk. If these treatments are not tolerated or fail to control pain, the use of NSAIDs may be warranted. Patients beginning NSAID therapy should start with a nonselective NSAID, such as ibuprofen or naproxen. However, the literature suggests naproxen as the nonselective NSAID of choice for these patients. If pain control is not established with nonselective NSAIDs, the next trial should be with an agent that is semiselective for COX-2, such as meloxicam or diclofenac.17
Don’t Miss: What To Do For Congestive Heart Failure
