Know Your Risk Factors
Certain populations have a higher risk for heart failure than others. Adults who are 65 or older have a higher risk than younger people. However, children and adolescents can have heart failure as well, particularly those who have a congenital heart defect. Men have a slightly higher risk for heart failure than women, and African-Americans have a higher risk than other races or ethnicities.
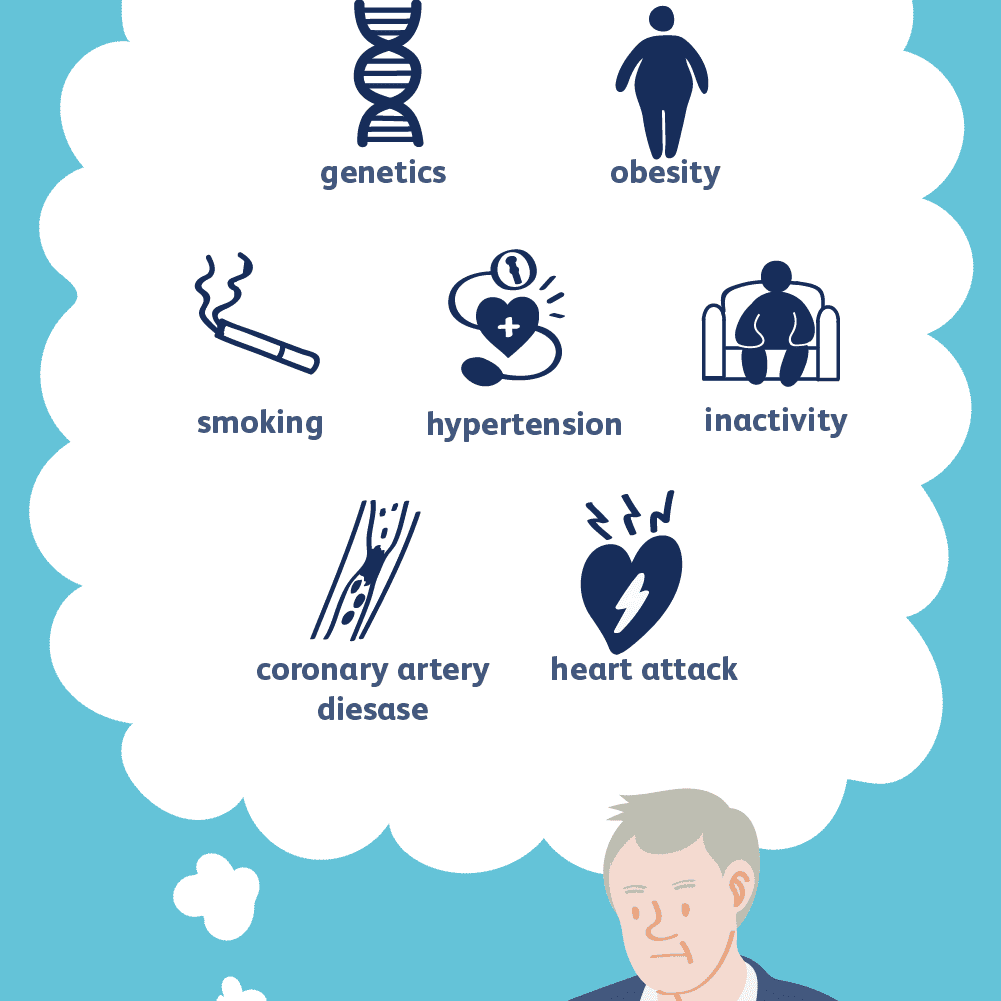
People who are overweight or obese also have a high risk for heart failure, as do people who have previously had a heart attack. Those suffering from coronary artery disease, in which narrowed arteries limit the heart’s supply of oxygen-rich blood, also have a high risk. Diabetes and some diabetes medications can increase the risk for congestive heart failure.
Other risk factors include high blood pressure, smoking, and excessive alcohol consumption.
Causes Of Heart Congestive Heart Failure
Most cases of heart failure are usually caused by underlying medical conditions such as:
High blood pressure : This condition weakens the heart and blood vessels and it triggers the buildup of plaque. This reduces the flow of blood and leads to congestive heart failure.
Cardiac arrhythmia: This is a condition characterized by irregular heartbeats and it a root cause of congestive heart failure.
Heart valve disease: This is a condition whereby the heart valves have problems and it leads to congestive heart failure with time.
Cardiomyopathy: This is a disease affecting the muscles of the heart and it leads to congestive heart failure.
Coronary artery disease: This is a condition characterized by narrowed arteries and it is mostly caused by the buildup of plaques on the walls of the arteries.
This leads to reduced flow of blood and congestive heart failure.
Congenital diseases and defects: These are problems present at birth and sometimes the heart can be affected.
Heart Disease Risk Factors
Cardiovascular disease can take many forms: high blood pressure, coronary artery disease, valvular heart disease, stroke, or arrhythmias
Cardiovascular disease can take many forms: high blood pressure, coronary artery disease, valvular heart disease, stroke, or arrhythmias . According to the World Health Organization, cardiovascular disease causes more than 17 million deaths in the world each year and is responsible for half of all deaths in the United States.
Coronary artery disease, the most common form of cardiovascular disease, is the leading cause of death in America today. Cancer, the second largest killer, accounts for a little more than half as many deaths.
In the United States, more than 80 million Americans have some form of cardiovascular disease. But thanks to many studies involving thousands of patients, researchers have identified certain factors that play important roles in a persons chances of developing heart disease. These are called risk factors.
Risk factors are divided into two categories: major and contributing. Major risk factors have been proven to increase your risk of heart disease. Contributing risk factors can lead to an increased risk of heart disease.
Major Risk Factors
High Blood Pressure . High blood pressure increases your risk of heart disease, heart attack, and stroke. If you are obese, smoke, or have high blood cholesterol levels along with high blood pressure, your risk of heart disease or stroke greatly increases.
You May Like: Do Antibiotics Increase Heart Rate
Congestive Heart Failure: Causes Symptoms And Risk Factors
Congestive heart failure is a condition that is characterized by the inability of the heart to pump sufficient amount of blood required to meet the needs of the body.
This condition is also called by many other names such as cardiac failure, right-sided heart failure, left-sided heart failure, and CHF . It also occurs when the heart is unable to pump blood fast enough.
Congestive heart failure does not signify that your heart has stopped working or its about to stop working. It simply means that your heart cannot pump sufficient amount of blood the way it should that meets the needs of the body.
As a result of this, the heart cannot meet up with the demands of the body and blood returns to the heart faster than it can be pumped out. Then the heart becomes congested.
One or both sides of your heart can be affected and it is caused by the weakening of the heart muscles. When your heart muscles are weak, the ability of your heart to pump blood will definitely be affected.
When this occurs, you might feel tired easily and have shortness of breath, a condition edema occurs in which fluid is collected in your legs, ankles, and feet. Another condition weakening of the hearts pumping ability causes is the accumulation of blood and fluid in the lungs.
What This Study Adds
-
Hypertension, diabetes, smoking history, and previous myocardial infarction conferred a greater relative risk of heart failure in younger than in older people
-
Risk factors had greater discriminatory value in predicting new onset of heart failure in younger than in older people
-
A greater proportion of the overall population attributable risk was explained by diabetes, smoking history, and previous myocardial infarction in younger than in older people
Don’t Miss: Heart Valve Disease Treatment Without Surgery
What Makes Yale Medicines Approach To Treating Congestive Heart Failure Unique
Yale Medicines team comprises heart failure cardiologists and cardiac surgeons, dedicated advanced-practice, registered nurses and nurse coordinators, dietitians, exercise physiologists, financial counselors, immunologists specializing in transplants, psychologists, and specialists in palliative care.
With a multidisciplinary approach, Yale Medicine physicians include the patients desires as well as input from the family to develop a comprehensive treatment plan that’s right for them.
What Are The Complications Of Heart Failure
Some of the complications from heart failure include:
- Irregular heartbeat.
- History of taking drugs that can damage your heart muscle, such as some cancer drugs.
Stage B
Stage B is considered pre-heart failure. It means your healthcare provider has given you a diagnosis of systolic left ventricular dysfunction but youve never had symptoms of heart failure. Most people with Stage B heart failure have an echocardiogram that shows an ejection fraction of 40% or less. This category includes people who have heart failure and reduced EF due to any cause.
Stage C
People with Stage C heart failure have a heart failure diagnosis and currently have or previously had signs and symptoms of the condition.
There are many possible symptoms of heart failure. The most common are:
- Shortness of breath.
- Need to urinate while resting at night.
- Rapid or irregular heartbeats .
- A dry, hacking cough.
- A full or hard stomach, loss of appetite or upset stomach .
There may be times that your symptoms are mild or you may not have any symptoms at all. This doesn’t mean you no longer have heart failure. Symptoms of heart failure can range from mild to severe and may come and go.
Unfortunately, heart failure usually gets worse over time. As it worsens, you may have more or different signs or symptoms.Its important to let your doctor know if you have new symptoms or if your symptoms get worse.
Also Check: How Does Heart Attack Happen
How Is Heart Failure Diagnosed
To find out if you have heart failure, your doctor will:
- Ask about your medical history, including your symptoms
- Ask about your family health history, including relatives who have had heart failure
- Do a physical exam
In some cases, your doctor may refer you to a cardiologist for tests, diagnosis, and care.
Types Of Congestive Heart Failure
Note that congestive heart failure is different from cardiac arrest, a condition that occurs when your heart stops beating. There are two main types of heart failure and they are:
Read Also: Heart Attack In Man
Systolic And Diastolic Failure
Systolic and diastolic heart failure each result in a decrease in stroke volume. This leads to activation of peripheral and central baroreflexes and chemoreflexes that are capable of eliciting marked increases in sympathetic nerve traffic.
Although there are commonalities in the neurohormonal responses to decreased stroke volume, the neurohormone-mediated events that follow have been most clearly elucidated for individuals with systolic heart failure. The ensuing elevation in plasma norepinephrine directly correlates with the degree of cardiac dysfunction and has significant prognostic implications. Norepinephrine, while directly toxic to cardiac myocytes, is also responsible for a variety of signal-transduction abnormalities, such as downregulation of beta1-adrenergic receptors, uncoupling of beta2-adrenergic receptors, and increased activity of inhibitory G-protein. Changes in beta1-adrenergic receptors result in overexpression and promote myocardial hypertrophy.
Age Dependent Associations Of Risk Factors With Heart Failure: Pooled Population Based Cohort Study
Don’t Miss: What Should Your Target Heart Rate Be
How Could I Get It
Certain problems can make your heart work harder than it should and weaken the muscle. Some of these are:
- High blood pressure
- Past heart attack
- Being too overweight
Things like drinking too much alcohol, smoking, and using illegal drugs are all known to damage your heart.
Some things that raise your chances of heart failure are out of your control, including:
- Heart defects you’re born with
Cure For Congestive Heart Failure
There is no cure for congestive heart failure yet but there are some natural therapies that can help you manage the symptoms of this condition and extend your lifespan.
As time goes on, congestive heart failure can get to its end-stage and it is highly important to know the end-of-life signs and symptoms for congestive heart failure.
Some of the signs and symptoms for end-of-life signs are:
Shortness of breath: This is also known as dyspnea and it is common throughout congestive heart failure but it becomes more persistent towards the end of life.
Patients will even experience dyspnea while resting as well.
No appetite: Lack of appetite is usually common in patients experiencing the end-of-life stage in chronic diseases including congestive heart failure.
Edema: These are swellings in different parts of the body and it occurs when the heart has difficulty in supplying sufficient amount of blood. Fluids can accumulate in the body thereby leading to swellings.
In congestive heart failure, these swellings usually happen in the abdomen and legs.
Rapid heartbeat: The heart will begin to beat faster because more pressure is put on it to pump more blood and this, in turn, would make the heart work harder.
Delirium and confusion: Patients with congestive heart failure will experience some disorientation sometimes because the level of sodium in the blood is changing.
Recommended Reading: Types Of Open-heart Surgery
What Is The Importance Of Ejection Fraction
Your ejection fraction is one way to measure the severity of your condition. If its below normal, it can mean that you have heart failure. Your ejection fraction tells your healthcare provider how good of a job your left or right ventricle is doing at pumping blood. Usually, your EF number is talking about how much blood your left ventricle is pumping out because its your heart’s main pumping chamber.
Several non-invasive tests can measure your EF. With this information, your healthcare provider can decide how to treat you or find out if a treatment is working as it should.
A normal left ventricular ejection fraction is 53% to 70%. An LVEF of 65%, for example, means that 65% of the total amount of blood in your left ventricle is pumped out with each heartbeat. Your EF can go up and down, based on your heart condition and how well your treatment works.
Symptoms Of Heart Failure
Symptoms of heart failure include:
- new or worsening shortness of breath
- difficulty lying flat at night
- fainting or passing out
- muscular fatigue, tiredness
- swelling of ankles or legs
- swelling of abdomen
- heart palpitations
- chest pain or discomfort in parts of the upper body
- unexplained coughing and wheezing
Also Check: Chronic Heart Failure Pathophysiology
Congestive Heart Failure: Prevention Treatment And Research
Congestive heart failure is a serious condition in which the heart doesnt pump blood as efficiently as it should. Despite its name, heart failure doesnt mean that the heart has literally failed or is about to stop working. Rather, it means that the heart muscle has become less able to contract over time or has a mechanical problem that limits its ability to fill with blood. As a result, it cant keep up with the bodys demand, and blood returns to the heart faster than it can be pumped outit becomes congested, or backed up. This pumping problem means that not enough oxygen-rich blood can get to the bodys other organs.
The body tries to compensate in different ways. The heart beats faster to take less time for refilling after it contractsbut over the long run, less blood circulates, and the extra effort can cause heart palpitations. The heart also enlarges a bit to make room for the blood. The lungs fill with fluid, causing shortness of breath. The kidneys, when they dont receive enough blood, begin to retain water and sodium, which can lead to kidney failure. With or without treatment, heart failure is often and typically progressive, meaning it gradually gets worse.
More than 5 million people in the United States have congestive heart failure. Its the most common diagnosis in hospitalized patients over age 65. One in nine deaths has heart failure as a contributing cause.
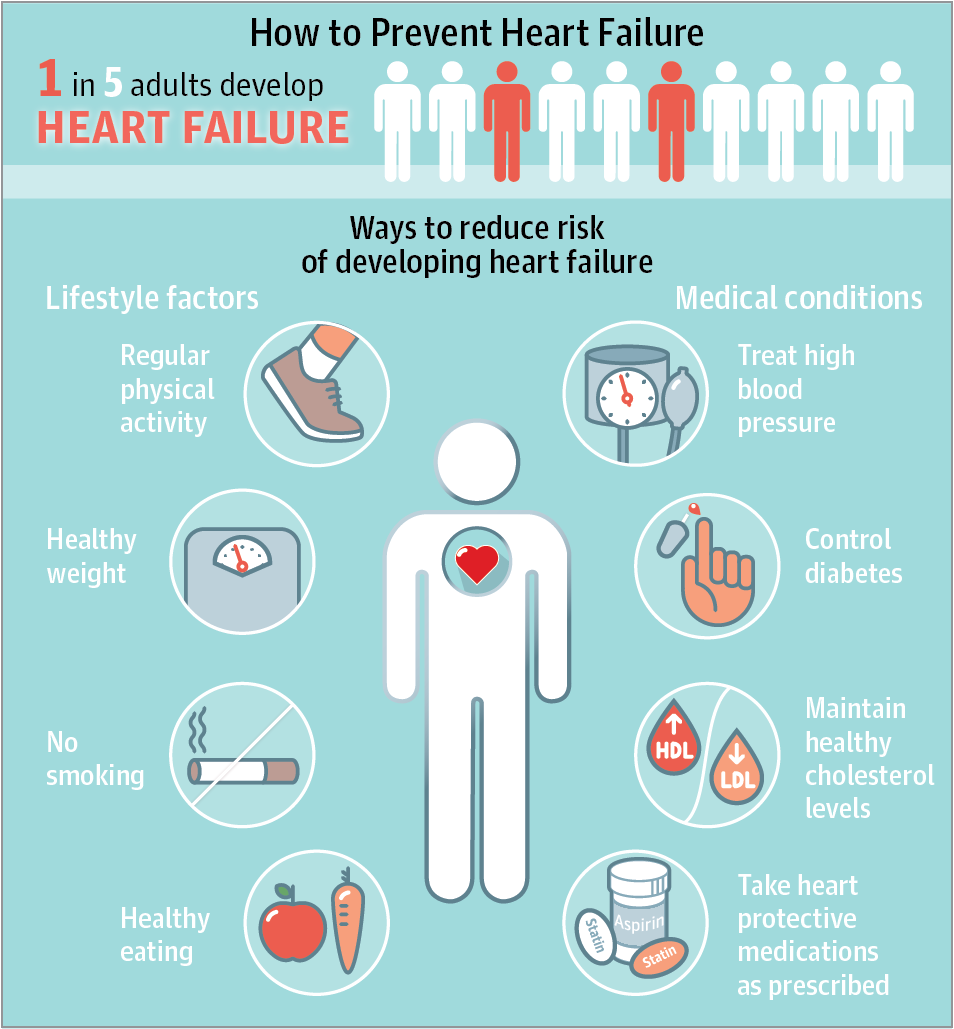
Can I Prevent Heart Failure
You can lower your odds of getting heart failure. And the earlier you start, the better your chances. You can begin with a few of these simple steps:
Show Sources
National Heart, Lung, and Blood Institute: “Who Is at Risk for Heart Failure?” “How Can Heart Failure Be Prevented?” “Physical Activity,” “Quitting Smoking,” “Heart-healthy eating,” “Aiming for a Healthy Weight,” “Managing stress.”
Mayo Clinic: “Heart Failure.”
American Heart Association: “About Heart Failure,” “Exercising more, sitting less helps men prevent heart failure,” “Alcohol and Heart Health,” “Illegal Drugs and Heart Disease,” “Causes of Heart Failure.”
CDC: “Heart Disease and Stroke.â
American Heart Association Go Red For Women: “Middle-Age Fitness: Reduce Heart Failure Risk.”
Pandey, A. American Heart Journal, February 2015.
NIH Senior Health: “Heart Failure.”
Young, D.R., Circulation: Heart Failure, January 2014.
Johns Hopkins Medicine: “Congestive Heart Failure: Prevention, Treatment and Research.”
American Thoracic Society: “Obstructive Sleep Apnea and Heart Disease.”
Gottlieb, D.J. Circulation, July 27, 2010.
Harvard Medical School: “Twelve Simple Tips to Improve Your Sleep.”
Also Check: Which One Of The Following Instructions For Monitoring Your Exercise Heart Rate Is Correct
Heart Failure With Preserved Ejection Fraction
In diastolic heart failure , the same pathophysiologic processes occur that lead to decreased cardiac output in systolic heart failure, but they do so in response to a different set of hemodynamic and circulatory environmental factors that depress cardiac output.
In HFpEF, altered relaxation and increased stiffness of the ventricle occur in response to an increase in ventricular afterload . The impaired relaxation of the ventricle then leads to impaired diastolic filling of the left ventricle .
Morris et al found that right venticular subendocardial systolic dysfunction and diastolic dysfunction, as detected by echocardiographic strain rate imaging, are common in patients with HFpEF. This dysfunction is potentially associated with the same fibrotic processes that affect the subendocardial layer of the LV and, to a lesser extent, with RV pressure overload. It may play a role in the symptomatology of patients with HFpEF.
What Are The Symptoms Of Left
Symptoms may be mild at first or you may think it’s a cold or allergy. You might not even notice them. But as heart functioning worsens, you may experience:
- Constant coughing.
- Shortness of breath with walking or bending over.
- Waking up short of breath or unable to lie flat at night.
- Swelling in your ankles, legs or abdomen.
Over time, the heart works harder to do its job. This causes complications that may include:
- Abnormal heart rates and rhythms .
Also Check: Icd10 Code For Heart Failure
How Is Heart Failure Treated
Your treatment will depend on the type of heart failure you have and, in part, what caused it. Medications and lifestyle behaviors are part of every treatment plan. Your healthcare provider will talk to you about the best treatment plan for you. Treatment is the same, regardless of gender.
As heart failure gets worse, your heart muscle pumps less blood to your organs, and you move toward the next stage of heart failure. Since you cant move backward through the heart failure stages, the goal of treatment is to keep you from moving forward through the stages or to slow down the progression of your heart failure.
Stage A treatment
The usual treatment plan for people with Stage A heart failure includes:
- Regular exercise, being active, walking every day.
- Stopping the use of tobacco products.
- Treatment for high blood pressure .
- Treatment for high cholesterol.
- Not drinking alcohol or using recreational drugs.
- Angiotensin-converting enzyme inhibitor or an angiotensin II receptor blocker if you have coronary artery disease, diabetes, high blood pressure, or other vascular or cardiac conditions.
- Beta-blocker if you have high blood pressure.
Stage B treatment
The usual treatment plan for people with Stage B heart failure includes:
Stage C treatment
The usual treatment plan for people with Stage C HF-rEF includes:
If the treatment causes your symptoms to get better or stop, you still need to continue treatment to slow the progression to Stage D.
Stage D treatment
