An Understanding Of The Basics
So, there are a couple of ways of determining your oxygen level. Your doctor may choose to do the more invasive ABG test. This will get an accurate PaO2 level for one point in time which can be very helpful.
However, the most common and easiest oxygen level to get is your SpO2. This can be checked at every doctor visit. A neat thing about pulse oximeters is they are easily portable. So, now we have devices that allow us to monitor your SpO2 while you are walking, and even while you are sleeping.
Now you understand the basic oxygen levels. You now know what oxygen levels are safe, or at least what oxygen level goals we are seeking.
Other Causes Of Heart Failure Include:
- abnormal heart rhythms where your heart beats too fast, too slow or irregularly
- amyloidosis – a build-up of abnormal proteins in organs such as your heart and tissues. When it affects the heart it’s called cardiac amyloidosis – stiff heart syndrome – and can lead to heart failure
- anaemia a lack of red blood cells carrying oxygen in your blood
- congenital heart conditions different heart problems that youre born with
- endocarditis – a viral infection affecting the heart muscle
- heart valve disease – where blood struggles to flow through the heart properly, putting extra strain on the muscle
- pulmonary hypertension – raised blood pressure in the blood vessels that supply your lungs. This condition can damage the right side of your heart, leading to heart failure. Find out more about pulmonary hypertension on NHS Choices and PHA UK
- some cancer treatments, such as chemotherapy
- thyroid gland disease an underactive or overactive thyroid gland which produces too few or too many hormones
- too much alcohol .
How Is Hypoxemia Treated
Depending on the underlying cause of hypoxemia, medications or other treatments can help raise your blood oxygen level. To help raise oxygen levels, your provider might use supplemental oxygen via oxygen tanks or oxygen concentrators. These may be needed continuously or only with exertion depending on the severity of the disease.
In the case of severe hypoxemia, especially with acute respiratory distress syndrome, healthcare providers may use a machine that breathes for you . If hypoxemia doesnt resolve, a condition known as refractory hypoxemia, additional medications or therapies may be used.
Treatments, which focus on the underlying cause, may include:
- Inhalers with bronchodilators or steroids to help people with lung disease like COPD.
- Medications that help to get rid of excess fluid in your lungs .
- Continuous positive airways pressure mask to treat sleep apnea.
- Supplemental oxygen may be used to treat an ongoing risk of hypoxemia. Oxygen devices vary, but you can expect to get a machine that delivers extra oxygen through a breathing mask or small tube . You may receive oxygen at home, with a portable machine while you travel, or in the hospital.
Recommended Reading: Do Stimulants Increase Heart Rate
How Is Heart Failure Treated In A Child
Treatment will depend on your childs symptoms, age, and general health. It will also depend on how severe the condition is.
If heart failure is caused by a congenital heart defect, correcting the defect may cure the heart failure. Medicines are often used to treat heart failure in children. They may include:
-
Digoxin. This is a medicine that can help the heart beat stronger with a more regular rhythm.
-
Water pills . These help the kidneys get rid of extra fluid that may build up in the body.
-
ACE inhibitors. These medicines help open the blood vessels and lower blood pressure. This makes it easier for your child’s heart to pump blood to the body.
-
Beta blockers. These help lower the heart rate and blood pressure. This also makes it easier for the heart to pump blood to the body.
Other treatments include:
-
Pacemaker. Some children with heart failure need an artificial pacemaker. The pacemaker may help when the heart is not pumping well because of a slow heartbeat.
-
Cardiac resynchronization therapy. This uses a special type of pacemaker. This treatment may be used in some children with long-term heart failure.
-
Mechanical support devices. Children with severe heart failure may be helped with special devices and tools. Your child may use these while waiting for a heart transplant.
-
Heart transplant. A healthy donor heart replaces your child’s diseased heart.
Bnp Measurement Not Indicated With Nesiritide Therapy
Nesiritide is a synthetic BNP analogue therefore, the measurement of BNP is not indicated in patients who are receiving nesiritide. If BNP is used as a diagnostic marker to rule in heart failure, the level must be determined before nesiritide therapy is started.
In a study by Miller et al, levels of NT-proBNP and BNP decreased in patients with advanced heart failure after therapy with nesiritide, but the majority of the patients did not have biochemically significant decreases in these markers even with a clinical response. The investigators were unable to give a definitive reason for their results, and they indicated that nesiritide therapy should not be guided by the use of levels of both markers. Fitzgerald et al also found decreased levels of both natriuretic peptides following nesiritide therapy in patients with decompensated heart failure.
For more information, see the Medscape Drugs & Diseases article Natriuretic Peptides in Congestive Heart Failure.
You May Like: What Is My Target Heart Rate To Burn Fat
Can Heart Failure Be Prevented
You may be able to prevent or delay heart failure if you:
- Work with your provider to manage any health conditions that increase your risk of developing heart failure
- Make healthy changes in your eating, exercise, and other daily habits to help prevent heart disease
NIH: National Heart, Lung, and Blood Institute
When To Seek Help
Patients with a life expectancy shorter than six months are eligible for hospice care. A hospice provides additional aid and resources to assist the person in living comfortably and with the highest possible quality of life. Hospice caregivers can also help patients and their families plan for future needs and circumstances. They have a unique insight into how to assist those with these difficulties.
Patients with end-stage heart failure need medical continuity throughout outpatient programs. These are just some of the symptoms that hospice care might help with. Positive inotropic drug infusions, anxiolytics, and sleeping medicines are all viable treatments. Its challenging for patients, families, and doctors caring for patients with end-stage heart failure to identify when treatment goals shift from survival to quality of life, allowing for a peaceful and dignified death.
You May Like: Can I Wipe Myself After Open Heart Surgery
Congestive Heart Failure Drugs
There are several medications that can be used to treat CHF, including ACE inhibitors, beta-blockers, and more.
ACE inhibitors
Angiotensin-converting enzyme inhibitors open up narrowed blood vessels to improve blood flow. Vasodilators are another option if you cant tolerate ACE inhibitors.
You may be prescribed one of the following:
voluntary recall of 5 lots of the drug Accupril due to the presence of nitrosamine. Nitrosamine, a known carcinogen with the potential to cause cancer, was found to exist in the drug at levels greater than the Acceptable Daily Intake as determined by the FDA. This recall is specific only to a handful of lot numbers and does not affect all Accupril tablets made by Pfizer. If you take Accupril tablets, talk with your pharmacist or doctor and they will help you determine if your medication has been impacted by the recall.
ACE inhibitors shouldnt be taken with the following medications without consulting a doctor, because they may cause an adverse reaction:
- Potassium-sparing diuretics and potassium supplements. These diuretics can cause potassium buildup in the blood, which may lead to abnormal heart rhythms. Examples include: riamterene , eplerenone , and spironolactone .
- Nonsteroidal anti-inflammatory drugs .NSAIDs such as ibuprofen, aspirin, and naproxen, can cause sodium and water retention. This may reduce the ACE inhibitors effect on your blood pressure.
Beta-blockers
This may be achieved with:
Diuretics
Your doctor may recommend:
What Is An Ejection Fraction
An ejection fraction is a measurement of the blood pumped out of your heart with each beat, expressed in a percentage. It can be measured using an echocardiogram , multigated acquisition scan, nuclear stress test, magnetic resonance imaging , or during a cardiac catheterization. A normal ejection fraction is between 50% and 70%.
Read Also: Can Progesterone Cause Heart Palpitations
Table Of Cutoff Values
Table 2, below, summarizes the evidence-based cutoff values of BNP and NT-proBNP for ruling in and ruling out the diagnosis of heart failure in the dyspneic patient presenting to the emergency department.
Table 2. Evidence-Based BNP and NT-proBNP Cutoff Values for Diagnosing HF
|
Criterion |
|
|
BNP = B-type natriuretic peptide GRF = glomerular filtration rate HF = heart failure LR = likelihood ratio NPV = negative predictive value NT-pro-BNP = N-terminal proBNP PPV = positive predictive value = not specifically defined. * Derived from Breathing Not Properly data . Derived from PRIDE data . Derived from subset of Breathing Not Properly data . |
BNP and NT-proBNP levels are higher in older patients, women, and patients with renal dysfunction or sepsis. Atrial fibrillation has also been associated with increased BNP levels in the absence of acute heart failure. However, BNP levels may be disproportionately lower in patients who are obese due to fat metabolism or who have hypothyroidism or advanced end-stage heart failure . NT-proBNP plasma levels are also lower in obese heart failure patients relative to nonobese patients with heart failure, regardless of whether the etiology is ischemic or nonischaemic.
How Is Hypoxemia Diagnosed
To diagnose hypoxemia, your healthcare provider will do a physical examination to listen to your heart and lungs. Abnormalities in these organs can be a sign of low blood oxygen. Your doctor may also check to see if your skin, lips or fingernails look bluish.
Your provider will use tests to check your oxygen levels, which can include:
- Pulse oximetry: A sensor that slips over your finger measures the amount of oxygen in your blood. Pulse oximetry is painless and noninvasive. Many doctors use it routinely each time you visit.
- Arterial blood gas test: A needle is used to take a blood sample from your wrist, arm or groin to measure the levels of oxygen in your blood.
- Six-minute walk test : You see your oxygen levels with exertion and how far you can walk on a flat surface in six minutes. This test helps evaluate lung and heart function.
Read Also: How Do You Calculate Your Max Heart Rate
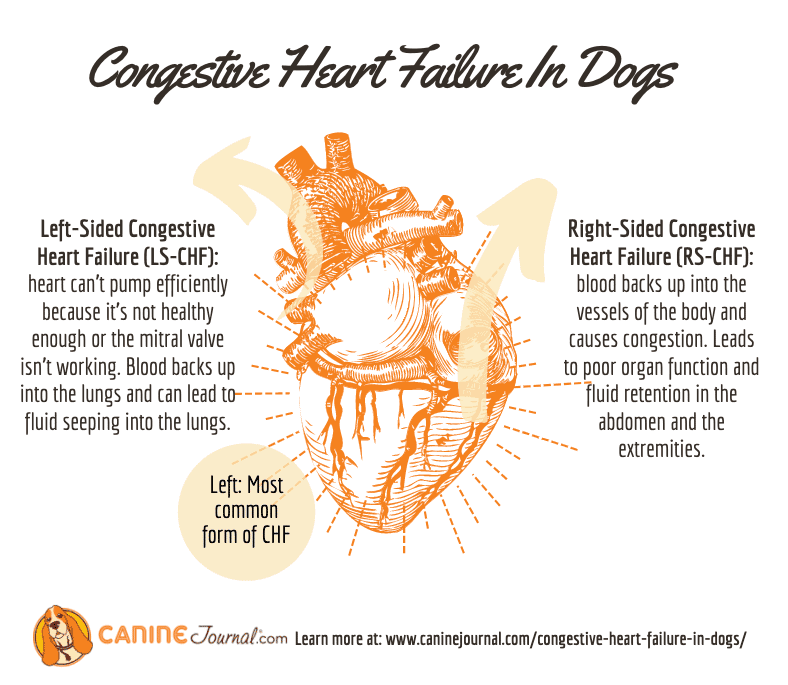
How The Normal Heart Works
The normal healthy heart is a strong, muscular pump a little larger than a fist. It pumps blood continuously through the circulatory system.
The heart has four chambers, two on the right and two on the left:
- Two upper chambers called atria
- Two lower chambers called ventricles
The right atrium takes in oxygen-depleted blood from the rest of the body and sends it through the right ventricle where the blood becomes oxygenated in the lungs.
Oxygen-rich blood travels from the lungs to the left atrium, then on to the left ventricle, which pumps it to the rest of the body.
The heart pumps blood to the lungs and to all the bodys tissues through a sequence of highly organized contractions of the four chambers. For the heart to function properly, the four chambers must beat in an organized way.
What Happens When Your Oxygen Level Drops To 70
When your oxygen level drops below 70%, you may experience a number of problems. These problems can range from mild to life-threatening, so it is important to know what to do if this happens.
The most common symptoms of low oxygen levels are confusion, drowsiness, and impaired coordination. If you experience any of these symptoms, it is important to get medical help as soon as possible.
Low oxygen levels can also lead to heart problems and seizures. If you experience any of these symptoms, it is essential to get medical attention as soon as possible.If you are at risk for low oxygen levels, be sure to talk to your doctor about how you can prevent these conditions. You can also take precautions such as wearing a mask when you are outdoors in cold weather or staying indoors when there is significant air pollution in the area.
also read : Heart disease left arm pain
Don’t Miss: Guideline Directed Medical Therapy Heart Failure
What Are Heart Failure Stages Or Classifications
While doctors define heart failure in stages or classifications, it represents a progression of heart muscle weakness. Sometimes people refer to this process as chronic heart failure but technically that term isn’t correct.
The New York Heart Association puts the stages of heart failure into four classifications:
- Class I: no limitations in activity. Normal activities can be performed.
- Class II: mild limitations and mild symptoms with activity no symptoms at rest
- Class III: noticeable limitations in activity only comfortable at rest
- Class IV: symptoms occur at any level of activity and uncomfortable even resting
The American Heart Association along with the American College of Cardiology grades heart failure in four stages, and takes into account that heart failure can be present even before symptoms appear:
- Stage A: No heart failure, but at high risk due to another medical condition that can lead to heart failure, such as high blood pressure, diabetes, obesity, or coronary artery disease.
- Stage B: The heart has been damaged by the patient’s other medical condition or other factors, but no symptoms are present yet.
- Stage C: The heart is damaged and the patient is experiencing heart failure symptoms.
- Stage D: The patient has severe heart failure that requires specialized care, despite receiving treatment .
What Are The Treatments For Heart Failure
Your treatment will depend on the type of heart failure you have and how serious it is. There’s no cure for heart failure. But treatment can help you live longer with fewer symptoms.
Even with treatment, heart failure usually gets worse over time, so you’ll likely need treatment for the rest of your life.
Most treatment plans include:
You may need heart surgery if:
- You have a congenital heart defect or damage to your heart that can be fixed.
- The left side of your heart is getting weaker and putting a device in your chest could help. Devices include:
- A biventricular pacemaker .
- A mechanical heart pump or a total artificial heart).
As part of your treatment, you’ll need to pay close attention to your symptoms, because heart failure can worsen suddenly. Your provider may suggest a cardiac rehabilitation program to help you learn how to manage your condition.
You May Like: What Happens To The Resting Heart Rate As A Result Of Regular Endurance Exercise
How Much You Need
Your doctor will measure your oxygen level with either a blood test or a device called a pulse oximeter. The pulse oximeter goes on your finger, toe, or earlobe. Itâs quick and painless, but not always as accurate as a blood test.
Your doctor will then give you a prescription for oxygen therapy, just like youâd get for medicine. It tells you how much oxygen you need and when to take it. Follow these directions closely.
How Can I Reduce My Risk Of Hypoxemia
The best way to reduce your risk of hypoxemia is to manage any underlying conditions that can lower your blood oxygen levels. If you’re living with lung or heart conditions, talk to your healthcare provider about your concerns and specific ways to lower your risk.
Even for those without heart or lung conditions, certain medications and situations like traveling to a higher altitude can increase your risk of hypoxemia. Ask your provider about any special precautions you need to take while traveling or taking medication. Allow time to safely adjust to higher altitudes when you travel.
Don’t Miss: Does Tylenol Increase Heart Rate
How Is Heart Failure Diagnosed In A Child
The healthcare provider will ask about your childs symptoms and health history. He or she will do a physical exam on your child. The provider will look for symptoms that may be related to heart failure. If the provider thinks your child has heart failure, your child may need to see a pediatric cardiologist. This is a doctor with special training to diagnose and treat heart problems in children. Tests for heart failure may include:
-
Blood and urine tests. Abnormal results may help find heart failure.
-
Chest X-ray. The X-ray may show heart and lung changes.
-
Electrocardiography . The ECG may show changes in the heart’s rhythm.
-
Echocardiography . Ultrasound waves are used to study the motion of the heart’s chambers and valves. The echo may show changes caused by heart failure such as enlarged chambers.
-
Cardiac catheterization. The doctor puts a small, flexible tube into a blood vessel and moves it to the heart. This measures pressure and oxygen levels inside the heart.
Assessment Of Functional Capacity
Cardiopulmonary stress testing can help in the assessment of a patients chance of survival within the next year, as well as determine the need for referral for either cardiac transplantation or implantation of mechanical circulatory support. A 6-minute walk test evaluates the distance walked, dyspnea index on a Borg scale from 0 to 10, oxygen saturation, and heart rate response to exercise. A normal value is walking more than 1500 feet. Patients who walk less than 600 feet have severe cardiac dysfunction and a worse short- and long-term prognosis.
References
Ho KK, Pinsky JL, Kannel WB, Levy D. The epidemiology of heart failure: the Framingham Study. J Am Coll Cardiol. 1993 Oct. 22:6A-13A. . .
American Heart Association. Classes of heart failure. Available at . Updated: May 8, 2017 Accessed: June 18, 2017.
Yancy CW, Jessup M, Bozkurt B, et al, American College of Cardiology Foundation/American Heart Association Task Force on Practice Guidelines. 2013 ACCF/AHA guideline for the management of heart failure: a report of the American College of Cardiology Foundation/American Heart Association Task Force on practice guidelines. Circulation. 2013 Oct 15. 128:e240-327. . .
Pina IL. Key points from the new heart failure guidelines . TheHeart.org. Available at . May 4, 2022 Accessed: May 6, 2022.
Recommended Reading: Which Of The Following Is Considered A Symptom Of A Heart Attack
