Heart Failure Nursing Diagnosis
Several nursing diagnoses could be used when caring for patients with heart failure. Some of the more common ones include
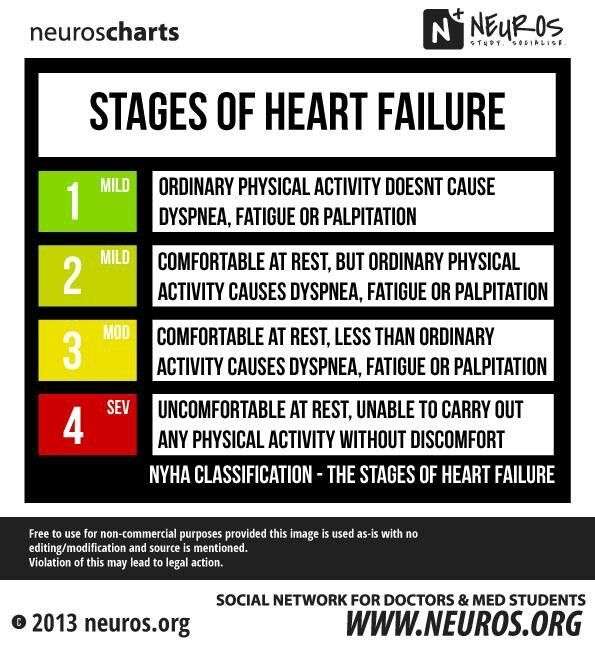
Anxiety occurs because those who suffer from heart failure may have symptoms such as shortness of breath, fatigue, and palpitations, resulting in constant worry about their health. Excessive anxiety may lead to depression and may affect the ability of the individual to carry out daily activities.
Diarrhea because heart failure commonly causes hypoproteinemia, a deficiency of protein in the blood, it can cause an inability to control bowel movements or trouble with defecation. This may prove to be embarrassing for the patient and have a negative impact on their well-being.
like congestive heart failure , restrictive cardiomyopathy is caused by decreased cardiac output due to impaired ventricular function, resulting in insufficient blood flow through the body. Because of this, heart failure patients may develop clinical signs such as peripheral edema and shortness of breath.
Chronic Pain heart failure can be associated with chronic pain due to the stress on the body from the reduced cardiac output and fluid overload .
Activity intolerance those who suffer from heart failure are often limited in the amount of physical activity they can participate in, which may severely impact their quality of life.
Fluid Overload heart failure is commonly related to fluid overload, which can be dangerous and lead to complications such as pulmonary edema.
Chf Nursing Care Plan 7
Nursing Diagnosis: Ineffective Breathing Pattern related to pulmonary congestion secondary to CHF as evidenced by shortness of breath, SpO2 level of 85%, cough, respiratory rate of 25 bpm, and frothy sputum
Desired Outcome: The patient will achieve effective breathing pattern as evidenced by normal respiratory rate, oxygen saturation within target range, and verbalize ease of breathing.
| CHF Nursing Interventions | |
| Assess the patients vital signs and characteristics of respirations at least every 4 hours. | To assist in creating an accurate diagnosis and monitor effectiveness of medical treatment. |
| Administer supplemental oxygen, as prescribed. Discontinue if SpO2 level is above the target range, or as ordered by the physician. | To increase the oxygen level and achieve an SpO2 value within the target range at least 96% |
| Administer the prescribed bronchodilators, steroids, or combination inhalers / nebulizers, as prescribed. | Bronchodilators: To dilate or relax the muscles on the airways. Steroids: To reduce the inflammation in the lungs. Inhalers or nebulizers To facilitate relaxation of the airway. |
| Elevate the head of the bed. Assist the patient to assume semi-Fowlers position. | Head elevation and semi-Fowlers position help improve the expansion of the lungs, enabling the patient to breathe more effectively. |
How To Conduct Electrocardiogram To Diagnose Heart Failure
Step 1: The patient will lie down or sit down if theyre too weak to stand.
Step 2: The doctor will place electrodes on the patients chest to check for electrical activity in the heart. These electrodes are placed over each of the hearts four chambers, and one electrode is also placed on their back .
Step 3: The doctor will apply a small amount of gel to each electrode and also put the back electrode in place.
Step 4: The doctor will turn on the EKG machine and read its printout for irregularities that may indicate heart failure. Depending on what is found, they may refer you to a specialist who can do further tests.
Read Also: Heart And Kidney Failure Symptoms
Impaired Gas Exchange Related To Ventilation/perfusion Imbalance As Evidenced By Breath Sounds Crackling Sounds Coughing Up Mucus And/or Blood Use Of Accessory Muscles Dyspnea
Breathing problems may be a sign of heart failure. As the heart gets weaker, it cant pump blood well enough to support your lungs and other organs. The amount and quality of blood flowing through your lungs may be reduced or cut off entirely because the heart has lost its ability to pump blood effectively.
- Crackling sound : This happens when fluid builds up in the lungs and gets pushed out with each breath you take. The fluid in your lungs produces raspy sounds as it passes through them when you breathe out.
- Coughing up mucus: Mucus buildup in the throat causes coughing as it tries to clear itself out when you swallow or move around too much during sleep this is known as dyspnea .
Study Population And Sample
The population consisted of hospitalized patients with heart failure over a period of 12 months , considering a simple random sampling selection and overall margin of error resulting in a maximum of n = 5%. Total sample size corrected by the size of the N population was calculated using the following formula: n=/1+1111 Callegari-Jacques SSM. BioestatÃstica: princÃpios e aplicações Porto Alegre: Artmed 2003.. The sample selected for this study respecting the inclusion and exclusion criteria included 70 patients. Therefore, the estimated ratios in this study are subject to maximum error of 8.75% and a 95% confidence level.
The sample selection was non-probabilistic with an initial composition of 84 patients, but with four losses due to hospital discharge before the end of data collection, six losses due to death and two losses due to discontinuity by transfers. The final sample consisted of 72 patients followed for three weeks of hospitalization from the time of hospital admission.
Also Check: How Do You Calculate Maximum Heart Rate
Recommended Reading: Symptoms Of Heart Attack Man
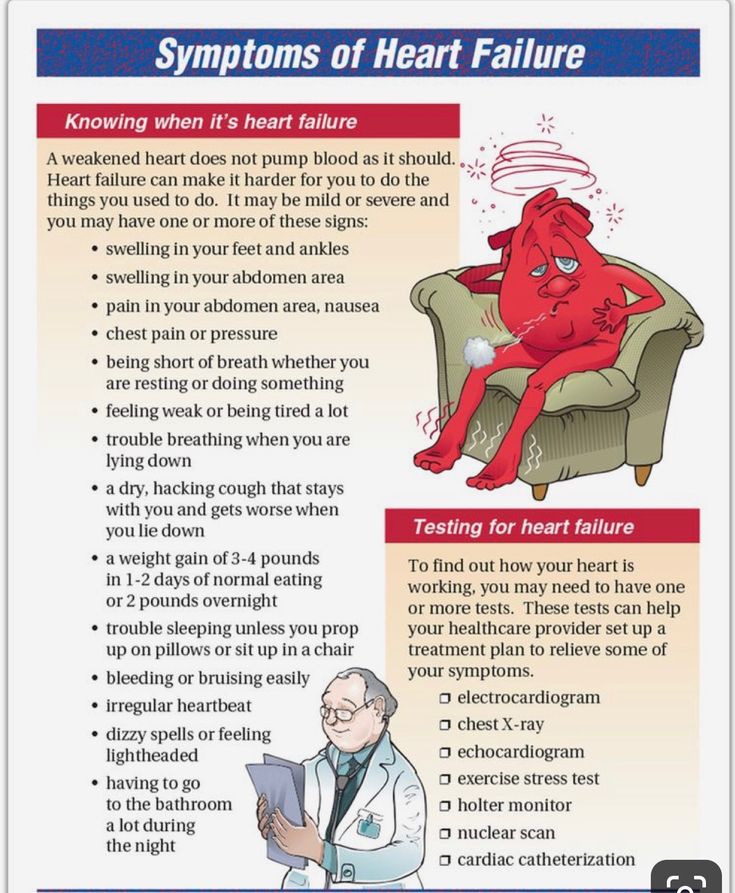
Diagnostic Tests For Heart Failure
Nursing Assessment For Deficient Knowledge
| Assessment | Rationale |
| Assess the patients knowledge regarding causes, treatment, and follow up care to heart failure. | This information provides data regarding knowledge of the patient about heart failure. It helps to plan educational sessions for the patient and family members. |
| Discuss with the patient and relatives about the disease and find out the existing misconceptions regarding treatment and care. | Finding out misconceptions and Clearing them out from the mind also guide future interventions. |
Recommended Reading: Why Does Caffeine Increase Heart Rate
Imbalanced Nutrition: More Than Body Requirements
May be related to:poor dietary habits, lack of exercise, excessive eating compared to nutritional needs, eating in response to emotional cues or external stimuli, poor dietary habits, lack of knowledge about appropriate portion size and food preparation.
As evidenced by:increased BMI, undesirable eating patterns, and sedentary lifestyle.
Ongoing Monitoring And Management
The ongoing monitoring of response to treatment and cardiopulmonary status also necessitates close monitoring of key haemodynamic parameters. In the immediate period of stabilisation, overly aggressive management with diuretics and vasodilators may lead to hypotension. Equally, patients may be undertreated or their underlying condition may deteriorate. Early warning scores allocate and weight points to vital signs outside pre-agreed ranges. These points are then summed to provide a single composite score. An increase in score will identify those patients who will benefit from escalation of monitoring or treatment. For example, they may benefit from an increased frequency of observationor ugent medical review. Escalation of treatment and alterations in management are then made in line with the score. To provide standardisation and limit misunderstanding the UK has adopted the National Early Warning Score for use in routine recording of clinical data, replacing traditional observation charts. Such tools have been reported to improve the ability of ward staff to identify and respond to indicators of clinical change.
Example Observation Chart Using Early Warning Scoring System
Recommended Reading: How Dangerous Is Open Heart Surgery
Chf Nursing Care Plan 2
Nursing Diagnosis: Impaired Gas Exchange related to alveolar edema due to elevated ventricular pressures as evidenced by shortness of breath, SpO2 level of 85%, and crackles upon auscultation.
Desired Outcome: The patient will have improved oxygenation and will not show any signs of respiratory distress.
| CHF Nursing Interventions | |
| Assess the patients vital signs and characteristics of respirations at least every 4 hours. | To assist in creating an accurate diagnosis and monitor effectiveness of medical treatment. |
| Administer supplemental oxygen, as prescribed. Discontinue if SpO2 level is above the target range, or as ordered by the physician. | To increase the oxygen level and achieve an SpO2 value within the target of at least 94%. |
| Encourage small but frequent meals. | To avoid abdominal distention and diaphragm elevation which lead to a decrease in lung capacity. |
| Elevate the head of the bed. Assist the patient to assume semi-Fowlers position. | Head elevation and semi-Fowlers position help improve the expansion of the lungs, enabling the patient to breathe more effectively. |
Ineffective Cerebral Tissue Perfusion
May be related to:tissue ischemia, reduction or interruption of blood flow, vasoconstriction, hypovolemia, shunting, depressed ventricular function, dysrhythmias, conduction defects.
As evidenced by:abnormal hemodynamic readings, dysrhythmias, decreased peripheral pulses, cyanosis, decreased blood pressure, shortness of breath, dyspnea, cold and clammy skin, decreased mental alertness, changes in mental status, oliguria, anuria, sluggish capillary refill, abnormal electrolyte, hypoxia, ABG changes, chest pain, ventilation perfusion imbalances, changes in peripheral resistance, impaired oxygenation of myocardium, ECG changes in S-T segment, T wave, U wave, palpitations.
Recommended Reading: Target Heart Rate For Stress Test
Immediate Assessment And Triage
Key issues in the nurses initial clinical assessment of suspected acute heart failure are summarised in Table 2 and adapted from the most recent recommendations on management. Nurse practitioners generally have an expanded skill set that enables them to also perform clinical examination to identify signs of congestion and refer for chest X-ray. Identifying clinical stability is an important first step in triage and enables the prompt transfer of the patient to the appropriate level of care for safe and effective therapy. This is largely influenced by the local organisation of services and skill sets of ward nurses. However, a patient at high risk of clinical deterioration or one requiring invasive cardiopulmonary support should ideally be transferred to the emergency resuscitation area, or an intensive or coronary care unit offering a lower patient-to-nurse ratio, closer patient monitoring and medical staff more available to support decision making.
Nursing Diagnoses : Heart Failure
- Impaired gas exchange related to increased preload and alveolar-capillary membrane changes
- Excess fluid volume related to increased venous pressure and decreased renal perfusion secondary to heart failure
- Activity intolerance related to imbalance between O2 supply and demand secondary to cardiac insufficiency and pulmonary congestion
Don’t Miss: Can Dehydration Cause Increased Heart Rate
Patient Education About Diuretic Therapy:
- Explain how to monitor intake and output. Encourage the patient to void at least every two to three hours. Tell the patient not to drink excessive amounts of water to avoid frequent urination.
- Advise the patient that he may experience fatigue, weakness, and dizziness with diuretic therapy. Instruct him not to perform any strenuous activity until he has gained strength after being discharged from the hospital.
- Instruct the patient to report signs of kidney dysfunction, including fatigue, nausea, vomiting, excessive thirst, difficulty urinating or feeling drowsy. Encourage him to notify the nurse if these symptoms occur immediately.
- Tell the patient that he may experience a metallic taste in his mouth with diuretic therapy. Advise him to report any changes in mouth odor or if he experiences dry mouth.
- Inform the patient that he will be given fluid and salt supplements as prescribed by the physician until urine output returns to normal levels. Instruct him to take these supplements with his meals and avoid taking excessive amounts of water.
- Instruct the patient to weigh himself daily and report any gain of more than two pounds in a twenty-four-hour period. If he weighs more than two pounds above his baseline weight, tell him to notify the nurse that he may be retaining fluid.
- Monitor fluid intake and output.
Educate the patient about fluid retention, healthy weight, and signs of dehydration:
Briefly explain how the medication works and what results should be expected:
Treatment For Heart Failure
- Angiotensin-converting enzyme inhibitors promotes vasodilation of the blood vessels, lowering the pressure and improving the blood flow .
- Beta blockers reduces heart rate and blood pressure .
- Angiotensin II receptor blockers similar to ACE inhibitors and can be used if the patient does not tolerate ACE inhibitors .
- Digitalis or digoxin improves the contraction of heart muscles, regulate heart rhythm and reduces heartbeat.
- Inotropes to improve the function of the heart to pump blood in severe heart failure.
- Diuretics to facilitate elimination of excess fluid in the body through urination .
- Inotropes. These are intravenous medications used in people with severe heart failure in the hospital to improve heart pumping function and maintain blood pressure.
2. Surgical interventions. These include coronary bypass surgery, heart valve repair or replacement, and heart transplant. It may also involve the insertion of medical devices such as implantable cardioverter-defibrillators , cardiac resynchronization therapy , and ventricular assist devices .
3. Lifestyle changes. A crucial part of the treatment plan for a patient with heart failure is to change several habits that are linked to the disease. These include smoking cessation, blood pressure control, diabetes management, dietary changes, stress management, exercise and increase in physical activity.
You May Like: Miracle Cure For Congestive Heart Failure
Nursing Diagnosis: Acute Cardiac Failure Cardiogenic Shock
Nanda-I Diagnosis Code: Nursing diagnosis code: 10213: NANDA-I code: K33.208
Signs & Symptoms: CHF is a condition where the heart fails to pump blood sufficiently throughout the body leading to vascular congestion and fluid accumulation in the lungs . This can lead to difficulty breathing, shortness of breath, fatigue, and ultimately death if not aggressively treated. Common signs of CHF include shortness of breath , fatigue, swelling, and weight gain in the abdominal region due to fluid retention. Cardiogenic shock signs and symptoms are similar to CHF, but they tend to be more severe, leading to a significantly increased risk for death within days or weeks if left untreated.
Health Teaching And Health Promotion
Nursing care plans for patients with HF must include patient education to improve clinical outcomes and reduce hospital readmissions. Patients need education and guidance on self-monitoring of symptoms at home, medication compliance, daily weight monitoring, dietary sodium restriction to 2 to 3 g/day, and daily fluid restriction to 2 L/day. In addition, patients with HF need aggressive treatment for underlying risk factors and the potential triggers for HF exacerbations. Modifiable risk factors include diabetes mellitus, hypertension, obesity, nicotine use, alcohol use disorder, and recreational drug use, especially cocaine. Patients with sleep apnea and HF should be encouraged to use continuous positive airway pressure therapy as uncontrolled sleep apnea can also increase HF-associated morbidity and mortality.
Don’t Miss: Congestive Heart Failure In Dogs Symptoms
Chf Nursing Care Plan 4
Nursing Diagnosis: Activity intolerance related to imbalance between oxygen supply and demand as evidenced by fatigue, overwhelming lack of energy, verbalization of tiredness, generalized weakness, and shortness of breath upon exertion
Desired Outcome: The patient will demonstration active participation in necessary and desired activities and demonstrate increase in activity levels.
| CHF Nursing Interventions | Rationales |
| Assess the patients activities of daily living, as well as actual and perceived limitations to physical activity. Ask for any form of exercise that he/she used to do or wants to try. | To create a baseline of activity levels and mental status related to fatigue and activity intolerance. |
| Encourage progressive activity through self-care and exercise as tolerated. Explain the need to reduce sedentary activities such as watching television and using social media in long periods. Alternate periods of physical activity with rest and sleep. | To gradually increase the patients tolerance to physical activity. |
| Teach deep breathing exercises and relaxation techniques. Provide adequate ventilation in the room. | To allow the patient to relax while at rest and to facilitate effective stress management. To allow enough oxygenation in the room. |
| Refer the patient to physiotherapy / occupational therapy team as required. | To provide a more specialized care for the patient in terms of helping him/her build confidence in increasing daily physical activity. |
Causes Of Heart Failure
Don’t Miss: How To Find Your Maximum Heart Rate
