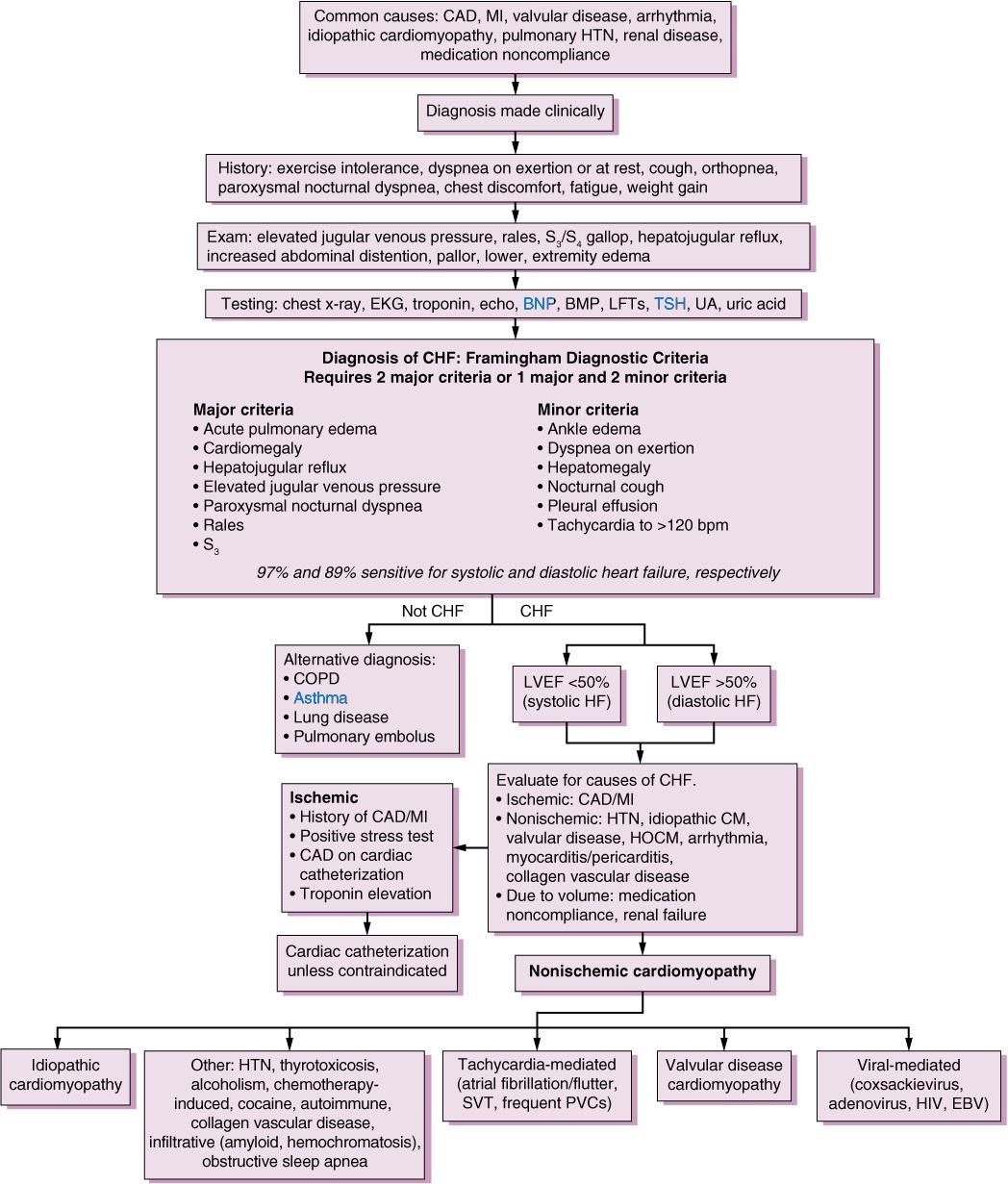
Causes Of Heart Failure
Also Check: Medication For Congestive Heart Failure
Heart Failure Nursing Diagnosis
Several nursing diagnoses could be used when caring for patients with heart failure. Some of the more common ones include
Anxiety occurs because those who suffer from heart failure may have symptoms such as shortness of breath, fatigue, and palpitations, resulting in constant worry about their health. Excessive anxiety may lead to depression and may affect the ability of the individual to carry out daily activities.
Diarrhea because heart failure commonly causes hypoproteinemia, a deficiency of protein in the blood, it can cause an inability to control bowel movements or trouble with defecation. This may prove to be embarrassing for the patient and have a negative impact on their well-being.
like congestive heart failure , restrictive cardiomyopathy is caused by decreased cardiac output due to impaired ventricular function, resulting in insufficient blood flow through the body. Because of this, heart failure patients may develop clinical signs such as peripheral edema and shortness of breath.
Chronic Pain heart failure can be associated with chronic pain due to the stress on the body from the reduced cardiac output and fluid overload .
Activity intolerance those who suffer from heart failure are often limited in the amount of physical activity they can participate in, which may severely impact their quality of life.
Fluid Overload heart failure is commonly related to fluid overload, which can be dangerous and lead to complications such as pulmonary edema.
Impaired Gas Exchange Related To Ventilation/perfusion Imbalance As Evidenced By Breath Sounds Crackling Sounds Coughing Up Mucus And/or Blood Use Of Accessory Muscles Dyspnea
Breathing problems may be a sign of heart failure. As the heart gets weaker, it cant pump blood well enough to support your lungs and other organs. The amount and quality of blood flowing through your lungs may be reduced or cut off entirely because the heart has lost its ability to pump blood effectively.
- Crackling sound : This happens when fluid builds up in the lungs and gets pushed out with each breath you take. The fluid in your lungs produces raspy sounds as it passes through them when you breathe out.
- Coughing up mucus: Mucus buildup in the throat causes coughing as it tries to clear itself out when you swallow or move around too much during sleep this is known as dyspnea .
Recommended Reading: What’s The Difference Between Cardiac Arrest And Heart Attack
Signs And Symptoms Of Atrial Fibrillation
Clinical manifestations of atrial fibrillation comprise of the following:
- Presence of palpitations, characterized by fast and pounding heartbeat
Atrial fibrillation can be classified under these subtypes:
- Occasional Also known as paroxysmal atrial fibrillation, this subtype have symptoms that comes and goes, with durations of a few minutes to hours. In this subtype, manifestations may occur for as long as a week they may occur repeatedly and may alleviate without treatment. However, occasional A-fib would still need therapeutic management.
- Persistent This subtype is characterized as atrial fibrillation with tenacious manifestations that do not revert to normal heart rhythm. Because of this, and its associated life-threatening effects, persistent atrial fibrillation would need cardioversion or other medical therapies in order to reinstate and sustain normal heart rhythm.
- Long-standing persistent Another subtype wherein the patient experiences consistent atrial fibrillation that lasts more than 12 months.
- Permanent In this subtype, the condition is persistent and therefore would need medications to regulate the heart rate and therefore, address the irregular heart rhythm.
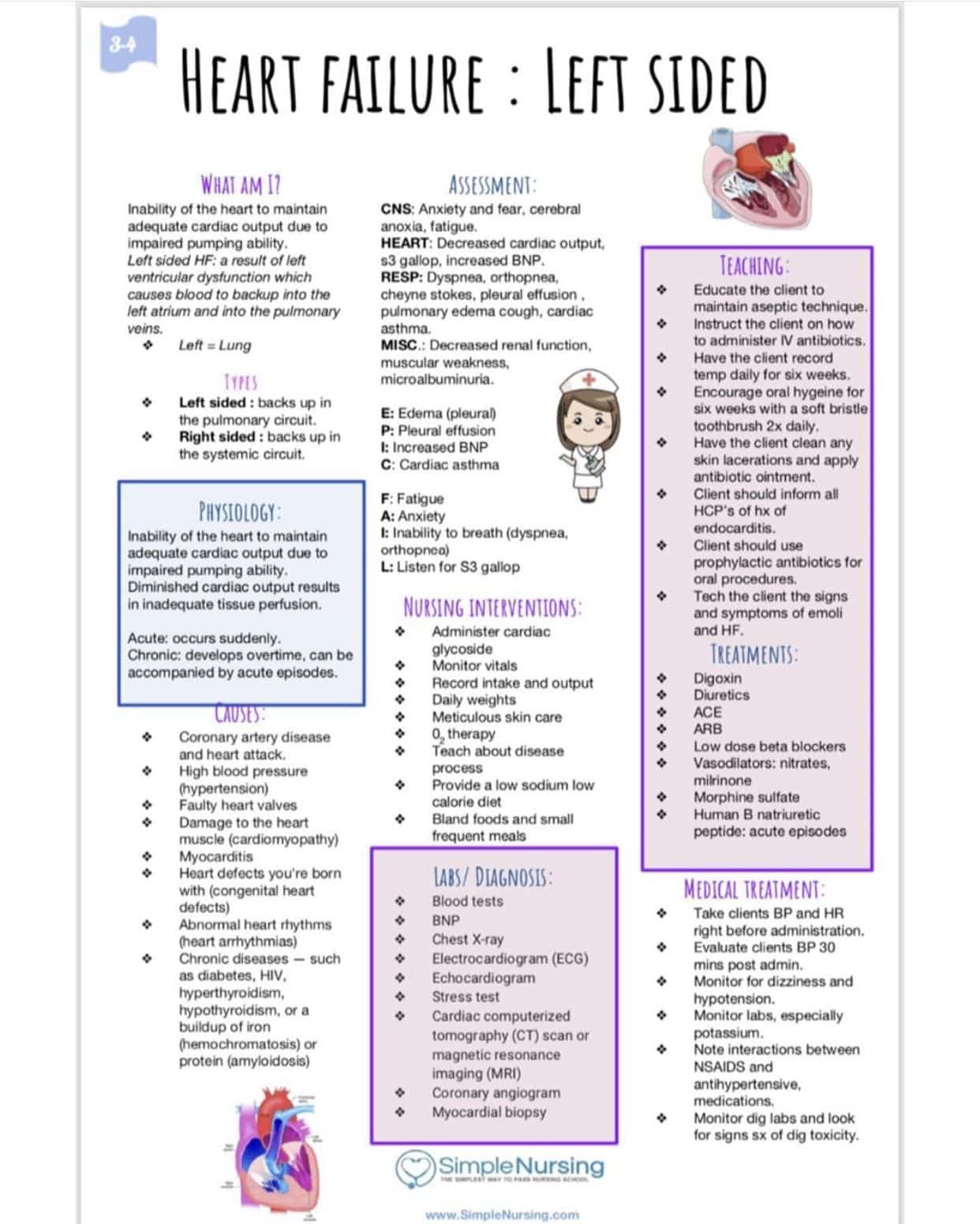
Nursing Assessment Of Heart Failure
- Take the complete history of symptoms, onset and duration of symptoms, the response of the symptom to rest. Assess the neurological status of the patient.
- Auscultate the heart sound, rhythm and measure the blood pressure. Assess for any peripheral edema.
- Assess for any defect in respiratory systems like, respiratory effort, presence of wheezes, crackles. Do percussion to find out any pleural effusion.
- Inspect neck for jugular vein distension and take hemodynamic measurements.
- Check abdomen for ascites and determine any weight change.
- Do laboratory tests to check serum electrolyte levels.
- Identify sleep patterns.
Recommended Reading: How To Find Your Heart Rate
Diagnostic Tests For Heart Failure
Risk Factors To Atrial Fibrillation
Risk factors associated with atrial fibrillation are as follows:
- Age. The risk of atrial fibrillation increase as the patient gets older.
- Heart disease. Patients with heart issues, such as congenital heart disease, congestive heart failure, coronary artery disease, history of heart attack, surgeries on the heart, and heart valve issues, increases the risk for atrial fibrillation.
- Hypertension. Hypertension, especially uncontrolled hypertension not managed with lifestyle modifications or medications, increases the risk for the condition.
- Thyroid disease. Thyroid problems may trigger arrhythmias in some people, including the development of atrial fibrillation.
- Other chronic health conditions. Conditions such as diabetes, metabolic syndrome, long-term kidney disease, lung issues, and apnea predispose a patient in developing atrial fibrillation.
- Alcohol use. Alcohol consumption may trigger episodes of atrial fibrillation in some people. Uncontrolled alcohol consumption further increases the risk.
- Obesity. Patients who are overweight have greater risks for atrial fibrillation.
- Familial history. Atrial fibrillation in the family may be passed down from generation to generation.
Read Also: Heart Failure Nursing Care Plan
Nursing Assessment For Deficient Knowledge
| Assessment | Rationale |
| Assess the patients knowledge regarding causes, treatment, and follow up care to heart failure. | This information provides data regarding knowledge of the patient about heart failure. It helps to plan educational sessions for the patient and family members. |
| Discuss with the patient and relatives about the disease and find out the existing misconceptions regarding treatment and care. | Finding out misconceptions and Clearing them out from the mind also guide future interventions. |
What Is Congestive Heart Failure
Heart failure is a chronic, progressive condition. It occurs when the heart is unable to pump effectively and produce enough cardiac output to successfully perfuse the rest of the bodys tissues and organs. An individual can have right-sided or left-sided heart failure as well as systolic or diastolic heart failure.
Left-sided heart failure is also known as Congestive Heart Failure . In CHF, the heart is either unable to contract completely or fill completely during relaxation. It can lead to an inadequate amount of blood pumping out of the heart. Thereby, backing up into the right side and then ultimately to the lungs and throughout the body causing congestion.
Systolic heart failure means the heart is not able to contract completely and affects its ability to pump blood out of the heart.
Diastolic heart failure means the heart is unable to relax fully between heartbeats and allows the appropriate amount of blood into the ventricle.
In this post, well formulate a sample nursing care plan for a patient with Congestive Heart Failure based on a hypothetical case scenario.
Don’t Miss: High Heart Rate And Low Blood Pressure
Nursing Interventions For Excess Fluid Volume
| Interventions | Rationale |
| Inform the patient and his/her relatives regarding fluid restriction. Advice to take fluid as per order. | Taking a low amount of fluid reduces extracellular volume. In advanced heart failure, fluid restriction is done around 1 litre/day. |
| Instruct the patient to take diuretics as prescribed. | Diuretics facilitates the excretion of excess body fluids. The patient could not maintain normal life due to an increase in the frequency of urination. So compliance with medication becomes difficult. For that, taking diuretics after work, or later in the day can increase compliance. |
| Instruct the patient to avoid a sodium-containing diet or take a low sodium diet. | Sodium retains water in the body. Restriction of sodium reduces excess fluid volume. |
| Instruct the patient to discuss with the physician regarding all the medication he/she is taking. | The patient may have comorbidities for which he/she may have taken some drugs. These drugs may counteract each other. So its better to discuss the medication taken by the patient. |
| Instruct the patient to contact the physician about any symptoms like weight gain, leg swelling, or change in breathing sounds. | Early recognition of symptoms can prevent readmission of the patient in the hospital. The patient can consult a doctor or nurse through telephone. |
| For severe fluid volume, excess considers the patient for hemofiltration or ultrafiltration. | It is an invasive procedure that draws out excess fluid in a short period. |
Nursing Diagnosis For Cardiovascular Diseases
by Daisy Jane Antipuesto RN MN·August 4, 2009
Cardiovascular diseases are a group of disorders of the heart and blood vessels and include:
- Coronary heart disease disease of the blood vessels supplying the heart muscle
- Cerebrovascular disease disease of the blood vessels supplying the brain
- Peripheral arterial disease disease of blood vessels supplying the arms and legs
- Rheumatic heart disease damage to the heart muscle and heart valves from rheumatic fever, caused by streptococcal bacteria
- Congenital heart disease malformations of heart structure existing at birth.
- Deep vein thrombosis and pulmonary embolism blood clots in the leg veins, which can dislodge and move to the heart and lungs.
Heart attacks and strokes are usually acute events and are mainly caused by a blockage that prevents blood from flowing to the heart or brain. The most common reason for this is a build-up of fatty deposits on the inner walls of the blood vessels that supply the heart or brain. Strokes can also be caused by bleeding from a blood vessel in the brain or from blood clots.
FACTS ABOUT CARDIOVASCULAR DISEASES
CAUSES OF CARDIOVASCULAR DISEASES
COMMON SYMPTOMS OF CARDIOVASCULAR DISEASES
POTENTIAL NURSING DIAGNOSIS FOR SEVERE HYPERTENSION:
Read Also: Congestive Heart Failure Exercise
Atrial Fibrillation Nursing Care Plan 3
Nursing Diagnosis: Anxiety related to breathlessness from inadequate oxygenation secondary to atrial fibrillation as evidenced by verbalizations of uncertainty and decreased concentration
Desired Outcome: The patient will be able to identify strategies to reduce anxiety by utilizing coping patterns.
Nursing Care Plan And Diagnosis For Fluid Volume Excess Fluid Overload Congestive Heart Failure Pulmonary Edema Ascites Edema And Fluid And Electrolyte Imbalance
This online nursing care plan below includes the following conditions: Fluid Volume Excess, Fluid Overload, Congestive Heart Failure, Pulmonary Edema, Ascites, Edema, and Fluid and Electrolyte Imbalance. What are nursing care plans? How do you develop a nursing care plan? What nursing care plan book do you recommend helping you develop a nursing care plan? This care plan
Also Check: How To Determine Maximum Heart Rate
Chf Nursing Care Plan 6
Nursing Diagnosis:Acute Pain related to decreased myocardial blood flow as evidenced by pain score of 10 out of 10, verbalization of pressure-like/ squeezing chest pain , guarding sign on the chest, blood pressure level of 180/90, respiratory rate of 29 cpm, and restlessness
Desired Outcome: The patient will demonstrate relief of pain as evidenced by a pain score of 0 out of 10, stable vital signs, and absence of restlessness.
Ongoing Monitoring And Management
The ongoing monitoring of response to treatment and cardiopulmonary status also necessitates close monitoring of key haemodynamic parameters. In the immediate period of stabilisation, overly aggressive management with diuretics and vasodilators may lead to hypotension. Equally, patients may be undertreated or their underlying condition may deteriorate. Early warning scores allocate and weight points to vital signs outside pre-agreed ranges. These points are then summed to provide a single composite score. An increase in score will identify those patients who will benefit from escalation of monitoring or treatment. For example, they may benefit from an increased frequency of observationor ugent medical review. Escalation of treatment and alterations in management are then made in line with the score. To provide standardisation and limit misunderstanding the UK has adopted the National Early Warning Score for use in routine recording of clinical data, replacing traditional observation charts. Such tools have been reported to improve the ability of ward staff to identify and respond to indicators of clinical change.
Example Observation Chart Using Early Warning Scoring System
Recommended Reading: How Dangerous Is Open Heart Surgery
You May Like: What Should My Heart Rate Be During Exercise
Clinical Symptoms Of Heart Failure
Heart failures early signs and symptoms are breathlessness or dyspnea, orthopnea, paroxysmal nocturnal dyspnea, lethargy/fatigue/weakness, oedema, abdominal distension, and right hypochondrial pain. The late stages of heart failure have signs and symptoms like tachycardia, pedal oedema, jugular vein distension, crackle sound of the lungs and S3 gallop sound.
Other symptoms of congestive heart failure are microvascular dysfunction which leads to an inadequate supply of oxygen. In some cases, hepatojugular reflux and ascites are found.
Prevention Of Atrial Fibrillation
Preventing atrial fibrillation involves the following lifestyle modifications:
- Eating healthy foods, specifically a diet rich in fruits, vegetables, and whole grains.
- Exercising regularly and increasing physical activity
- Quitting tobacco smoking
- Ensuring regular check-ups with a healthcare provider.
Recommended Reading: How Long To Recover From Heart Attack
Goals Of The Discharge Plan In Advanced Heart Failure
Planning for discharge is an important component of the HF patients hospital stay, particularly in multimorbid patients or those in the advanced stages of their disease. Studies have shown that effective discharge planning, performed by a multidisciplinary team, can reduce rehospitalization rates and improve mortality through better communication and patient care across disciplines, clinical specialties, and geographical boundaries., Indeed, an earlier discharge can be facilitated when there is a collaborative approach involving the patient, secondary care HF professionals, and social and primary care teams.
The ultimate goal is being to provide a seamless system of care ensuring optimal patient management, no matter where the patient begins or continues their healthcare journey, resulting in better outcomes.
Thus, the development of an effective plan of care for patients with advanced HF should be the responsibility of the multidisciplinary HF team, ideally commenced on diagnosis, be that within the hospital or community setting. Written or electronic recommendations should be tailored to the needs of the patient and family members, the organization and resources available. For example, there is an increasing trend towards the remote monitoring of patients or telemedicine.,
Chf Nursing Care Plan 2
Nursing Diagnosis: Impaired Gas Exchange related to alveolar edema due to elevated ventricular pressures as evidenced by shortness of breath, SpO2 level of 85%, and crackles upon auscultation.
Desired Outcome: The patient will have improved oxygenation and will not show any signs of respiratory distress.
| CHF Nursing Interventions | |
| Assess the patients vital signs and characteristics of respirations at least every 4 hours. | To assist in creating an accurate diagnosis and monitor effectiveness of medical treatment. |
| Administer supplemental oxygen, as prescribed. Discontinue if SpO2 level is above the target range, or as ordered by the physician. | To increase the oxygen level and achieve an SpO2 value within the target of at least 94%. |
| Encourage small but frequent meals. | To avoid abdominal distention and diaphragm elevation which lead to a decrease in lung capacity. |
| Elevate the head of the bed. Assist the patient to assume semi-Fowlers position. | Head elevation and semi-Fowlers position help improve the expansion of the lungs, enabling the patient to breathe more effectively. |
Read Also: What Heart Rate To Burn Fat
Nursing Care Plan Diagnosis Interventions Risk For Aspiration Impaired Swallowing Ineffective Swallowing Difficulty Swallowing Dysphagia Peg Tube Feeding And Difficulty Chewing
This nursing care plan and diagnosis with nursing interventions is for the following condition: Risk For Aspiration, Impaired Swallowing, Ineffective Swallowing, Difficulty Swallowing, Dysphagia, Peg Tube Feeding, and Difficulty Chewing. What are nursing care plans? How do you develop a nursing care plan? What nursing care plan book do you recommend helping you develop a nursing
Atrial Fibrillation Nursing Care Plan 4
Acute Pain
Nursing Diagnosis: Acute pain related to decreased myocardial blood flow and increased cardiac workload or oxygen consumption secondary to atrial fibrillation as evidenced by reports of pain with varying frequency, duration and intensity, narrowed focus, distraction behaviors , and autonomic responses
Desired Outcomes:
- For the patient to report anginal episodes that have decreased in frequency, duration, and severity.
- For the patient to demonstrate pain relief as evidenced by the absence of muscle tension and restlessness, and stable vital signs.
You May Like: How To Slow Down My Heart Rate
