Overall Effect Of The Icd On Survival
Among the 98,946 patients in the cohort, patients who underwent ICD implantation had a 25% lower risk of death after adjustment for the SHFM during follow-up over 5 years compared with control patients. Kaplan-Meier curves for patients with ICDs and control patients are shown in Figure 2A.
Overall Survival by SHFM Score in Control and ICD Cohorts
Kaplan-Meier curves demonstrate survival by SHFM in ICD and control cohorts. In both groups, an increase in the SHFM quintile is associated with decreased survival over 5 years. ICD = Implantable Cardioverter Defibrillator SHFM = Seattle Heart Failure Model SPRM = Seattle Proportional Risk Model.
Derivation Of Modified Shfm Score
During 730 days of the observational period, seven patients died and six patients had heart failure readmissions.
In the univariate analyses, the original SHFM score trended towards though did not reach statistical significance in association with the primary endpoint . Among the hemodynamic data, pulmonary capillary wedge pressure trended towards an association while cardiac index was significantly associated with the primary endpoint . According to the calculated cutoff and hazard ratio obtained in the multivariate analysis, a modified SHFM score was derived: 6 Ã + 5 Ã + 4 Ã .
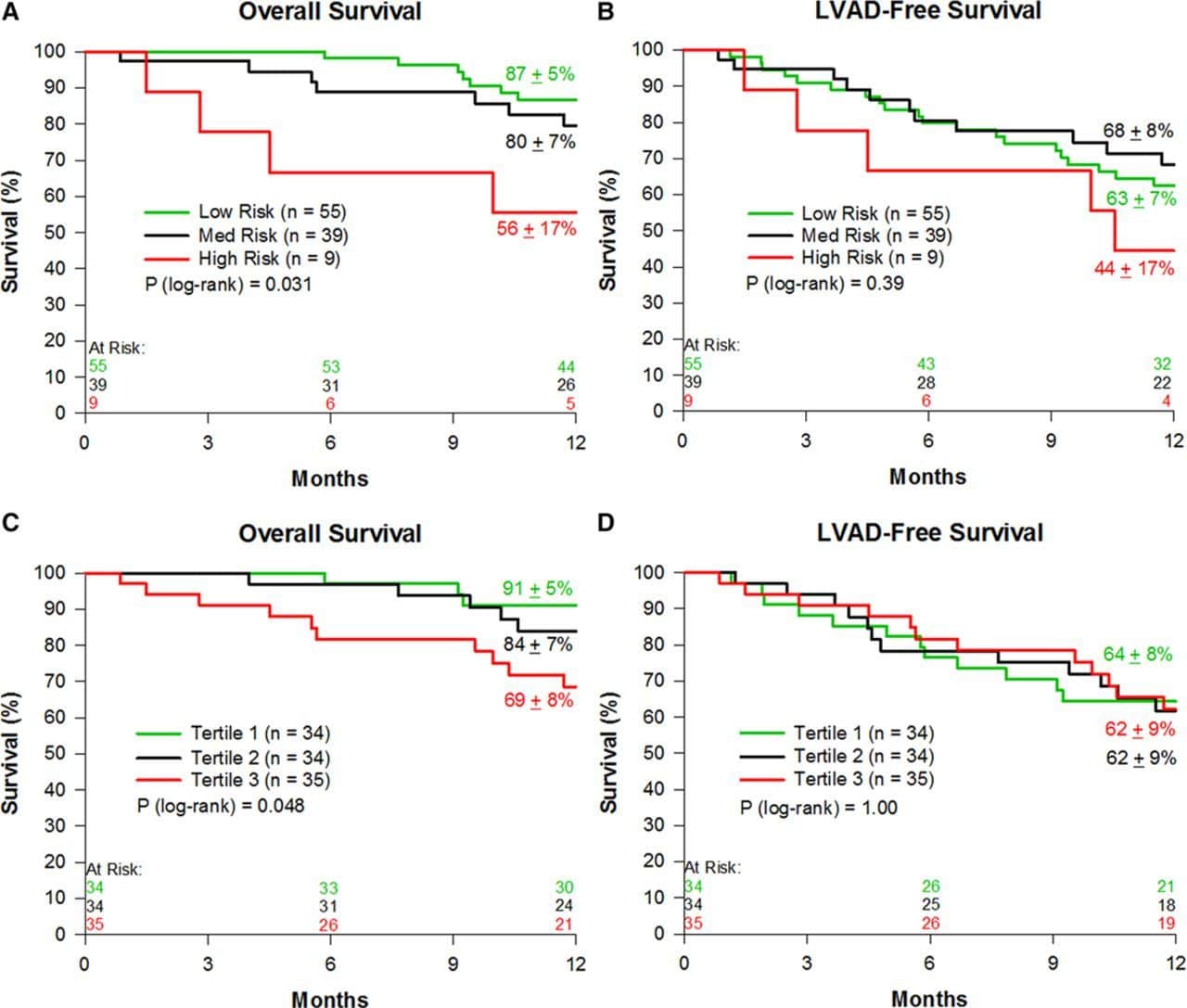
Seattle Heart Failure Model Score And Overall Mortality
An increase in SHFM quintile was associated with increased mortality in both the ICD and non-ICD cohorts . Table 2 demonstrates robust prediction of overall survival with the ICD based on SHFM quintiles. In a multivariable logistic regression models, SHFM was essentially as good as all the covariates combined for prediction of 3-year mortality . The ICD HRs are shown in specific subgroups of interest based on the model covariates in Figure 3. The findings in Figure 3 with respect to subgroups based on ischemic versus nonischemic etiology of cardiomyopathy stratified by age groups of < 59 years old, 59 to 67 years old, and 68 years old show decreased benefit in patients with nonischemic cardiomyopathy and age 68 years old, consistent with the results of the recent DANISH ICD trial . Although both women and men had statistically significant hazard ratios favoring the ICD, the ICD was favored even more strongly in men than in women .
Forest Plot for the Effect of the ICD on Survival in Subgroups of Interest
Also Check: Recovery From Open Heart Surgery
Clinical Implications Of The Modified Shfm Score
The modified SHFM score would be particularly useful as part of shared decision-making for TAVR candidates . In patients who have intrinsic severe diastolic dysfunction that may remain post-TAVR despite valve correction, the estimated residual risk that remains must be considered in light of advanced age or other comorbid conditions that may independently negate a long-term benefit of TAVR. Considering these additive risks as shown in our modified SHFM score, alternative therapies including medication adjustment, palliative care, and balloon aortic valvuloplasty alone might be considered, instead of the standard TAVR procedure .
Given our findings, aggressive interventions to optimize hemodynamics before TAVR might improve the score and clinical outcomes, although further prospective analyses of this unique question are needed.
Linkage And Determination Of Outcomes
Linkage between the ICD Registry and the SSDI was performed based on social security number by the NCDR Analytic Center to determine vital status through October 2011. In the control cohort, survival data were obtained directly from the associated registries and clinical trials. Of note, time to death was available for all patients. While the cause of death was not available for this analysis, the magnitude of the ICD-associated improvement in survival relative to control patients was easily determined and used as the primary outcomes measure to address the study hypotheses. The rationale for this approach is that the mechanism by which ICDs improve survival is through treatment of VA to prevent arrhythmic death .
Don’t Miss: How To Tell If Having Heart Attack
Validation Of The Modified Shfm Score
The modified SHFM score was calculated in all patients in the validation cohort. The distribution of the modified SHFM score in the validation cohort is shown in Figure 3. During a median of 730 days in the observational period, seven patients died and eight patients had heart failure readmissions.
Distribution of modified SHFM score in the validation cohort. Patients were assigned to the low score group , the intermediate score group , and the high score group .
The hazard ratio of the modified SHFM score for the primary endpoint was 1.34 . The area under the curve of the modified SHFM was 0.879 .
Receiver operating characteristics analysis of the modified SHFM score to predict the primary endpoint in the validation cohort.
If patients were assigned to the low score group , the intermediate score group , or the high score group , the 2-year cumulative incidence of the primary endpoint was stratified by these three groups . The hazard ratio of the intermediate score group versus the low score group was 6.31 . The hazard ratio of the high score group versus the low score group was 17.6 . Heart failure readmission rates similarly increased in incidence when stratified by the three groups .
Study Design And Sample
The present study was based on data from 2 Japanese AHF registries: the West Tokyo Heart Failure and National Cerebral And Cardiovascular Center Acute Decompensated Heart Failure registries. The design of the WET-HF and NaDEF registries has been reported previously.14, 15 Briefly, the WET-HF registry is a large, ongoing, prospective, multicenter cohort registry designed to collect data on clinical backgrounds and outcomes of patients hospitalized for AHF.14 From 2006 to 2016,
Recommended Reading: Does Melatonin Lower Heart Rate
Determination Of Shfm And Sprm Scores From Icd Registry
As some variables for the SHFM model were missing in the NCDR registry and could not be used in the SHFM model, the following variables were used to create a slightly revised version of the SHFM with comparable statistical power that could be prospectively applied to both NCDR registry patients and controls: age, gender, NYHA class, ischemic etiology, LVEF, systolic blood pressure, sodium, creatinine, angiotensin converting enzyme inhibitor use or angiotensin receptor blocker use, beta blocker use, digoxin use, diuretic use , statin use, and the new variables of diabetes mellitus, lung disease, and QRS width. The SPRM in this cohort was calculated as previously described using age, gender, NYHA class, LVEF, systolic blood pressure, sodium, creatinine, digoxin use, diabetes mellitus, and the substitution of ischemic etiology of cardiomyopathy for BMI , as both ischemic etiology of cardiomyopathy and BMI had similar statistical power. Both models were derived in the control group and prospectively applied in the NCDR registry. For simplicity, we refer to these slightly revised models as SHFM and SPRM in the present analysis.
The Seattle Heart Failure Model Is A Predictor Of Mortality After Kidney Transplant In Patients With End Stage Renal Disease And Heart Impairment
A. Perez-Gutierrez1, P. J. Bachul2, D. N. Danz3, B. Juengel2, M. Josephson2, J. Fung2, P. Witkowski2, B. Chung4, Y. Becker2
1Surgery, University of Chicago, Chicago, IL, IL, 2Surgery, University of Chicago, Chicago, IL, 3Economics, University of Pittsburgh, Pittsburgh, IL, 4Cardiology, University of Chicago, Chicago, IL
Session Date & Time: None. Available on demand.
Location: Virtual
*Purpose: Cardiovascular disease is the main cause of mortality after kidney transplantation. Many patients with ESRD have heart failure that is attributed to fluid overload. The Seattle heart failure model is a risk model based on clinical status, therapy and laboratory parameters. It includes the following variables: age, gender, NYHA class, ejection fraction , ischemic disease, systolic BP, use of angiotensin-converting enzyme inhibitor, angiotensin receptor blocker, statin, betablocker, diuretics, allopurinol, sodium, hemoglobin, lymphocytes, uric acid, and cholesterol. It predicts survival in patients with heart failure. Our objective was to apply this model to patients with ESRD at the time of their evaluation for kidney transplant and to determine whether the model predicts mortality after transplant.
*Methods: This is a retrospective study of all adult, deceased donor kidney transplants from 2014 to 2017. We used univariate and multivariate logistic regression models .
You May Like: How Blood Flows Through The Heart
Study Population End Point
Prospectively collected clinical, pharmacologic, and laboratory data of 427 consecutive patients referred for CRT from 2004 to 2010 were evaluated. According to guidelines effective during the implantation period, classic indications for CRT were reduced left ventricular ejection fraction of < 35%, left bundle branch block with QRS duration > 120 ms on the surface electrocardiogram, and limited functional capacity . However, in a significant proportion of patients not all of
Enhancing Palliative Care For Patients With Advanced Heart Failure Through Simple Prognostication Tools: A Comparison Of The Surprise Question The Number Of Previous Heart Failure Hospitalizations And The Seattle Heart Failure Model For Predicting 1
- 1Department of Internal Medicine and Cardiology, Charité Universitätsmedizin Berlin, Berlin, Germany
- 2Brookdale Department of Geriatrics and Palliative Medicine, Icahn School of Medicine at Mount Sinai, New York, NY, United States
- 3James J. Peters Veterans Affairs Medical Center, Geriatric Research Education and Clinical Center, Bronx, NY, United States
- 4Department of Medicine, University of Chicago Medicine, Chicago, IL, United States
Background: Score-based survival prediction in patients with advanced heart failure is complicated. Easy-to-use prognostication tools could inform clinical decision-making and palliative care delivery.
Objective: To compare the prognostic utility of the Seattle HF model , the surprise question , and the number of HF hospitalizations within the last 12 months for predicting 1-year survival in patients with advanced HF.
Methods: We retrospectively analyzed data from a cluster-randomized controlled trial of advanced HF patients, predominantly with reduced ejection fraction. Primary outcome was the prognostic discrimination of SHFM, SQ answered by HF cardiologists, and NoH, assessed by receiver operating characteristic curve analysis. Optimal cut-offs were calculated using Youdens index .
SQ and NoH yielded comparable utility to SHFM for 1-year survival prediction among advanced HF patients, are easy-to-use and could inform bedside decision-making.
You May Like: What Is Heart Palpitations Symptoms
Seattle Heart Failure Model
Benbarkat et al reported that the Seattle Heart Failure Model grossly overestimated survival by 4.79 years in patients with heart failure aged > 80 years. As the developer of the SHFM, I would like to correct some errors made by the investigators. The complete formula for the SHFM is available in the original report. The investigators chose to use the interactive model we developed and extrapolated for age > 85 years rather than calculating the individual values. It is uncertain how much error this may have introduced in the reported values.
The SHFM reports estimated survival from 1 to 5 years and mean life expectancy for a patient cohort with similar values. Mean life expectancy is the least accurate of the calculated values. Mean life expectancy is the area under the Kaplan-Meier survival curve and is quite different from median survival as reported by Benbarkat et al . For example, it is possible to estimate that the mean life expectancy in this heart failure cohort is about 3.5 years, compared with the median observed survival of 1.91 years.
Seattle Proportional Risk Model And Overall Mortality
Whereas the SHFM score was strongly associated with all-cause mortality even with the ICD, the SPRM score was strongly associated with the magnitude of benefit from the ICD even after adjustment for SHFM. Figure 4 demonstrates how increasing SPRM score was associated with the effect of the ICD on survival based on the fitted line of the SPRM ICD interaction in the Cox proportional hazards model. For example, patients in SPRM quintiles 1 and 2 had a 19 to 21% reduction in mortality with the ICD, while patients in SPRM quintiles 4 and 5 had a 38 to 40% adjusted reduction in mortality with the ICD . In a multivariable model for survival, the covariates of ICD , SPRM , SHFM , and the interaction terms SPRM*ICD and SHFM*ICD were all significant. The high level of significance for the SPRM*ICD interaction term demonstrated that the benefit of ICD implantation clearly increased as the SPRM estimated proportion of sudden death increased. Of note, the SPRM*ICD interaction term favored the ICD more strongly when the cohort was limited to patients with ischemic cardiomyopathy versus those with nonischemic cardiomyopathy .
SPRM and the Improvement in Survival with ICDs
Read Also: What Chamber Of The Heart Pumps Blood To The Lungs
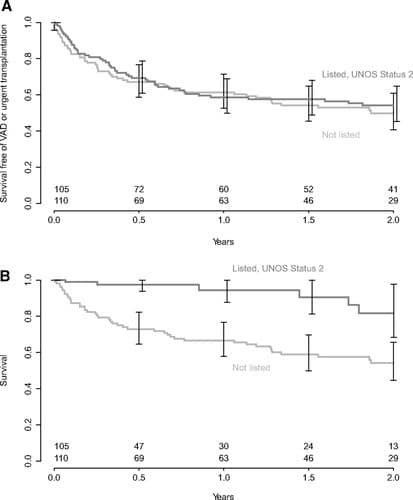
Combined Assessment Of Overall Survival And Effect Of Icd On Survival With Shfm And Sprm
Combined use of the SHFM score and SPRM score for comprehensive risk stratification in ICD candidates is of particular interest. In order to create 4 groups of equal size based on SHFM and SPRM , we used threshold values based on the median SPRM-predicted proportional rate of arrhythmic death and the median SHFM-predicted 1-year mortality rate . Characteristics of the patients in these 4 groups can be found in the Online Table. Kaplan-Meier survival curves for patients in these 4 groups with and without an ICD are shown in Figure 5AD. The ICD had a clear benefit in patients with both SHFM-predicted 1-year mortality 5.7% and a SPRM-predicted proportional risk of sudden death above the median, but not in patients with an SHFM-predicted one year mortality 5.7% and a SPRM-predicted proportional risk of sudden death below the median . Among patients with an SHFM-predicted 1-year mortality rate > 5.7%, patients with a higher SPRM-predicted proportional risk of arrhythmic death above the median had a greater adjusted improvement in survival over 5 years with the ICD compared with patients having a SPRM-predicted proportional risk of arrhythmic death 44.3% . HRs for the ICD versus control patients are shown in more granular fashion in Table 2 in a 5×5 matrix form for specific quintiles of SPRM and SHFM. The SHFM-adjusted mortality rates at 1 and 5 years by quintile of SPRM score and quintile of SHFM score is shown in Figure 6.
