Difficulties Concerning Pediatric Sampling
The position of the patient during blood sampling affects ANP levels substantially. Moving into supine position causes levels of ANP to rise, probably as a consequence of venous return and the following increment in atrial pressure . In severe heart failure, a change from supine to upright position is associated with further increase of supine ANP levels, likely caused by tachycardia or increased sympathetic nervous activity . Therefore also crying, which is common in infants during venipuncture, is most likely influencing levels of ANP and also excitement may play a role. Further the site of blood collection matters because central and peripheral plasma concentrations differ . Thus, a well-standardized protocol is needed and deviations have to be recorded in order to be able to interpret findings adequately.
Meaningful Alternatives To Blood Sampling
The European Medicines Agency demands considering non-invasive alternatives to blood sampling whenever possible for pediatric studies .
Urine
ANP is found in urine as well and was determined in children to assess the possibility of circumventing stressful blood sampling in children . But ANP was not detectable in healthy controls . Urine levels did not correlate with plasma levels in CHD patients . Further, it was not possible to distinguish patients with and without clinical signs by the means of urinary ANP. As the main metabolism of ANP is not organ-specific , measurement of ANP in urine cannot make up as an alternative to plasma measurement. Hence, NT-pro-peptides which are renally excreted could rather be an alternative, but currently there is no data for NT-proANP, NT-proBNP, or also BNP in urine in pediatric heart failure.
Saliva
In healthy men, ANP can be measured in saliva which correlates with plasma levels . So far, no studies evaluated the significance of salivary ANP in heart failure, but for NT-proBNP and BNP first studies were conducted. Those indicate that adult heart failure patients present higher levels than controls . Saliva offers the advantages of being non-invasive, less demanding and easier to handle than blood. Thus, further research should be conducted since it seems to offer a promising alternative approach to the determination of biomarkers in heart failure, an approach which would be especially advantageous in pediatrics.
Collection And Processing Of Blood Samples
ANP has a short half-life and has to be treated carefully after blood sampling . Despite its short half-life, it is proven that ANP with EDTA and aprotinin is stable for 2 months at 20°C and for 2 h at room temperature which allows for analysis . Plasma should be obtained as fast as possible as ANP clearance receptors are located on platelets and therefore concentrations in whole-blood diminish . Hemolyzed samples should be excluded as falsely low concentrations of ANP will be measured . However, hemolytic samples can be used for the determination of NT-proANP .
Recommended Reading: Afrin Heart Palpitations
Prognostic Importance Of Elevated Troponin T And Troponin I
More recently, our study found that cTnT had significant additional value for prognostication beyond the standard clinical, biochemical, dialysis, and echocardiographic measures, including LV mass and ejection fraction, in chronic PD patients. Furthermore, the predictive value of cTnT for mortality, cardiovascular outcomes, and noncardiovascular death was independent of inflammation, residual renal function, LV hypertrophy and dysfunction, and clearing, confirming the additional value of measuring cTnT in early identified high-risk patients with ESRD. Our study also demonstrated superiority of cTnT over hs-CRP in predicting long-term mortality and cardiovascular risk in chronic PD patients however, our results differed from the Netherlands Cooperative Study on the Adequacy of Dialysis study, which found limited additional predictive power of cTnT over other clinical risk factors in a combined cohort of HD and PD patients. The reason for these differences is not clear.
What Is It Used For
A BNP test detects a rise in BNP, which indicates heart failure. Your doctor may recommend this test if you have symptoms of heart failure, such as shortness of breath.
Early diagnosis of heart failure can make sure that you get quick and effective treatment to prevent further complications.
Your doctor may order a BNP blood test if you have symptoms of heart failure, including:
- abnormally high or irregular heart rate
- coughing a lot, and producing white or pink phlegm
- nausea or having no appetite
A BNP test can also help rule out heart failure. Other conditions can cause elevated BNP levels, including lung or kidney conditions and obesity.
Also Check: How Accurate Is Fitbit Charge 2 Heart Rate
Metabolic Effect Of Atrial Natriuretic Peptide In Cardiac Myocytes
Cardiac cells usually use fatty acids as metabolic substrates. However, they revert to glucose consumption during hypoxia to maintain myocardial viability. Clinical and experimental studies have shown that increased glucose uptake during acute myocardial ischaemia is associated with preserved cardiac function and decreased release of myocardial enzymes., In rat neonatal cardiac myocytes, hypoxia significantly increased glucose uptake, and this was stimulated by the addition of ANP, although ANP alone did not significantly affect basal glucose uptake under normoxic conditions. This metabolic effect of ANP may partly contribute to cardioprotection in the ischaemic heart. These findings indicate that ANP has a variety of biological actions that contribute to cardioprotection after ischaemia/reperfusion injury, both as a circulating hormone and local autocrine paracrine factor in the heart. Several studies have revealed that ANP inhibits ischaemia/reperfusion injury in isolated hearts and animal models as discussed in the next section.
Effect Of Atrial Natriuretic Peptide On Sympathetic Nerve Activity
Sympathetic hyperactivity not only increases electrical instability of the myocardium, but also is responsible for an increase in platelet aggregation, coronary vasoconstriction, and higher wall stress. Previous studies have found that increased sympathetic activity is associated with a high risk of malignant ventricular arrhythmias during myocardial ischaemia.,
Abramson et al. investigated the effect of ANP on muscle sympathetic nerve activity in patients with heart failure. Fifteen patients with dilated cardiomyopathy received intravenous ANP or NTG . During each infusion, MSNA, BP, central venous pressure , and HR were recorded before and during lower body negative pressure at 6 and 12 mmHg. NTG and ANP caused similar, significant reductions in CVP and diastolic BP, although resting MSNA did not increase with either infusion. LBNP at 6 mmHg only lowered the CVP but not BP, however, LBNP at 12 mmHg caused significant reductions in both CVP and BP. These effects of non-hypotensive and hypotensive LBNP on CVP and BP were similar during ANP and NTG infusions, yet MSNA was lower both before and during LBNP during ANP infusion . Non-hypotensive LBNP increased MSNA during NTG infusion , but not during ANP infusion . These observations support the concept that ANP exerts a sympatho-inhibitory action.
You May Like: Can Flonase Cause Heart Palpitations
Chronic Heart Failure As A State Of Reduced Effectiveness Of The Natriuretic Peptide System: Implications For Therapy
Program of Cardiovascular Diseases, Centre for Applied Medical Research, and Department of Cardiology and Cardiac Surgery, University of Navarra Clinic, University of Navarra, Pamplona, Spain
Corresponding author
Program of Cardiovascular Diseases, Centre for Applied Medical Research, and Department of Cardiology and Cardiac Surgery, University of Navarra Clinic, University of Navarra, Pamplona, Spain
Corresponding author
What Is The Ratio Of Coronary Capillaries To Cardiac Muscle Cells
1. Question : What is the ratio of coronary capillaries to cardiac muscle cells?
2. Question : What part of the kidney controls renal blood flow, glomerular filtration, and renin secretion?
3. Question : What effect do natriuretic peptides have during heart failure when the heart dilates?
4. Question : What is the primary site for uncomplicated local gonococci infections in men?
5. Question : Which term is used to identify the movement of gas and air into and out of the lungs?
6. Question : Which manifestations of vasoocclusive crisis are associated with sickle cell disease in infants?
7. Question : When a patient has small, vesicular lesions that last between 10 and 20 days, which sexually transmitted infection is suspected?
8. Question : What is the role of collagen in the clotting process?
9. Question : Immunoglobulin E is associated with which type of hypersensitivity reaction?
10. Question : When an individual aspirates food particles, where would the nurse expect to hear decreased or absent breath sounds?
11. Question : Research supports the premise that exercise has a probable impact on reducing the risk of which cancer?
12. Question : In a normal, nonmutant state, an oncogene is referred to as a:
13. Question : What is the trigone?
14. Question : Erythrocyte life span of less than 120 days, ineffective bone marrow response to erythropoietin, and altered iron metabolism describe the pathophysiologic characteristics of which type of anemia?
Recommended Reading: Thrz Calculator
Pathophysiology Of Dilated Cardiomyopathy
, and beriberi Thiamin Deficiency Thiamin deficiency is most common among people subsisting on white rice or highly refined carbohydrates in developing countries and among alcoholics. Symptoms include diffuse… read more . Many toxic substances, particularly alcohol, various organic solvents, iron or heavy metal ions, and certain chemotherapeutic drugs , damage the heart. Frequent ventricular ectopy has been associated with left ventricular systolic dysfunction.
Sudden emotional stress and other hyperadrenergic states can trigger acute dilated cardiomyopathy that is typically reversible . An example is acute apical ballooning cardiomyopathy . In this disorder, usually the apex and occasionally other segments of the left ventricle are affected, causing regional wall dysfunction and sometimes focal dilation .
Genetic factors play a role in 20 to 35% of cases > 60 genes and loci have been implicated.
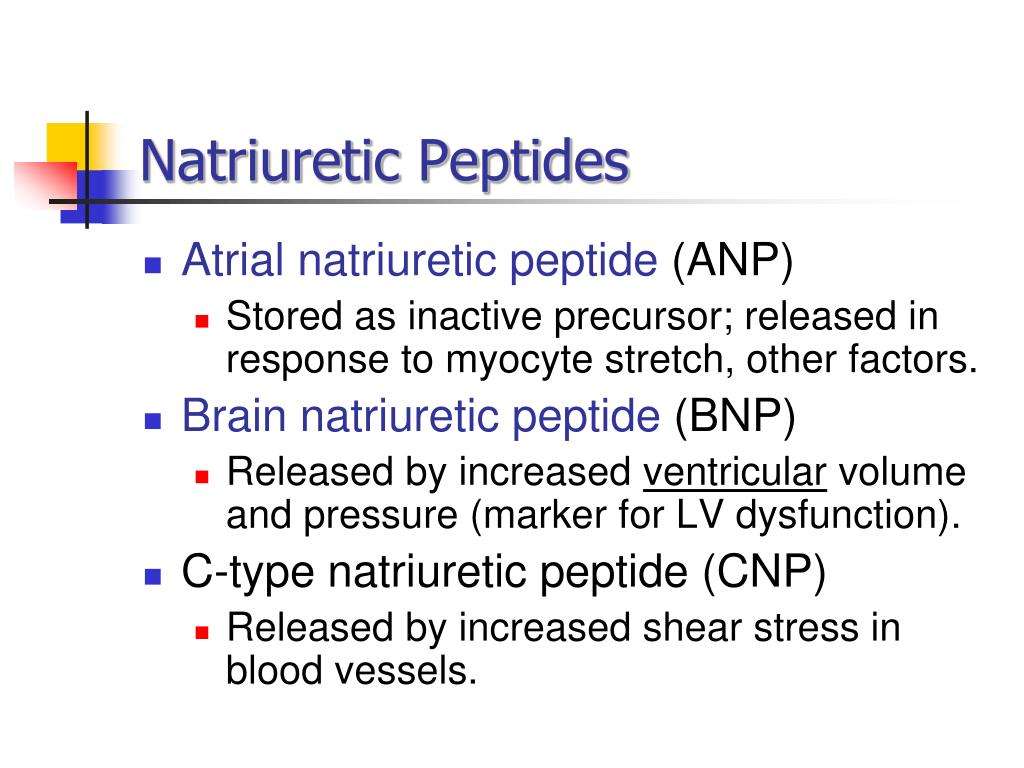
What Is The Role Of Atrial Natriuretic Peptide And B
ANP and BNP are endogenously generated peptides activated in response to atrial and ventricular volume/pressure expansion. ANP and BNP are released from the atria and ventricles, respectively, and both promote vasodilation and natriuresis. Their hemodynamic effects are mediated by decreases in ventricular filling pressures, owing to reductions in cardiac preload and afterload. BNP, in particular, produces selective afferent arteriolar vasodilation and inhibits sodium reabsorption in the proximal convoluted tubule. It also inhibits renin and aldosterone release and, therefore, adrenergic activation. ANP and BNP are elevated in chronic heart failure. BNP especially has potentially important diagnostic, therapeutic, and prognostic implications.
Read Also: Why Do Av Nodal Cells Not Determine The Heart Rate
Ischaemia/reperfusion Model In Isolated Hearts
Sangawa et al. investigated the effect of ANP on cardiac function after ischaemia/reperfusion in isolated rat hearts. Rat hearts were subjected to 15 min of global ischaemia followed by 15 min of reperfusion, and ANP was added at the time of reperfusion. In the ANP treated group, the recovery of cardiac output was significantly better than in the control group with a similar trend towards recovery of coronary flow . Improved cardiac function was closely related to a significant increase in post-ischaemic cGMP release. Similar results were obtained in the isolated rabbit heart. Rabbit hearts were subjected to 30 min of ischaemia followed by 120 min of reperfusion. ANP treatment just before reperfusion significantly reduced infarct size . The effect was mimicked by an activator of cGMP-dependent protein kinase.
Natriuretic Peptides In Heart Failure
1. Question : What physical sign is the result of turbulent blood flow through a vessel?
2. Question : Which organism is a common sexually transmitted bacterial infection?
3. Question : It has been determined that a tumor is in stage 2. What is the meaning of this finding?
4. Question : Erythrocyte life span of less than 120 days, ineffective bone marrow response to erythropoietin, and altered iron metabolism describe the pathophysiologic characteristics of which type of anemia?
5. Question : When an individual aspirates food particles, where would the nurse expect to hear decreased or absent breath sounds?
6. Question : What is the first stage in the infectious process?
7. Question : Causes of hyperkalemia include:
8. Question : Which term is used to describe a muscle cell showing a reduced ability to form new muscle while appearing highly disorganized?
9. Question : The drug heparin acts in hemostasis by which processes?
10. Question : What is the major concern regarding the treatment of gonococci infections?
11. Question : What is the most common cause of insufficient erythropoiesis in children?
12. Question : What is the most abundant class of plasma protein?
13. Question : Decreased lung compliance means that the lungs are demonstrating which characteristic?
14. Question : Which immunoglobulin is present in childhood asthma?
15. Question : What is the functional unit of the kidney called?
17. Question : Why is nasal congestion a serious threat to young infants?
Don’t Miss: Ibs Heart Palpitations
The Natriuretic Peptide System In Heart Failure
Congestive HF is a complex syndrome characterized by sodium and water retention. A decrease in cardiac output and effective intra-arterial volume leads to renal retention of sodium and water despite expansion of the extracellular fluid volume. This phenomenon occurs in the presence of a progressive activation of the NP system . However, this response is apparently insufficient to counteract the activation of vasoconstriction and sodium retention of RAAS and SNS .
Several clinical and experimental studies have implicated both ANP and BNP in the pathophysiology of the deranged cardiorenal axis in HF. Early studies have shown that ANP release in response to acute volume overload or chronic salt loading are impaired in asymptomatic patients with cardiomyopathy and LV dysfunction . This impairment of ANP adaptation to volume challenge in the early stages of HF is associated with blunted natriuretic, vasodilator and reninaldosterone suppressing actions. Therefore, this hormonal abnormality may play a role in the progression of sodium retention and vasoconstriction in HF. It is interesting that pre-treatment with RAAS-inhibiting drugs, such as ACE inhibitors, may partially restore the ANP secretagogue response to volume expansion in HF and that pre-treatment with an ARB may preserve the natriuretic and renal vasodilating capacity of ANP in the same condition .
Practical Application In Ckd
Renal function limits current use of NPs in patients with CKD . Plasma NP levels in patients with CKD are related to CKD severity, and cutoff levels are increased as CKD stages advance. Plasma BNP levels rise to almost 200 pg/ml in patients with CKD but without HF. Compared with plasma BNP levels, plasma NT-proBNP levels may be more strongly correlated with GFR and affected by age-related decrease in GFR, suggesting careful use of NT-proBNP in elderly with CKD . In patients with CKD, plasma NT-proBNP levels > 1200 pg/ml suggest chronic HF in patients < 50 years of age and > 4502 pg/ml in patients between 50 and 75 years old . It remains unclear if elevated NP levels in CKD effectively reflect the activation of NP system and effects on target organ. Elevated NP levels may have reduced ability to activate NP system and affect target organ in CKD. NP resistance in CKD may be caused by downregulated NPR-A expression in renal medulla and upregulated NPR-C expression in renal cortex . NP resistance in CKD results in the invalidity of NP infusion in protecting renal function and treating cardiorenal syndrome in patients with HF .
You May Like: Can Flonase Cause Heart Palpitations
Anp In Pediatric Heart Failure
A literature search using PubMed resulted in 147 studies of which 22 were classified as relevant and included in this review . Publications had to meet the following inclusion criteria: original research papers regarding pediatric population with congenital heart defect and/or heart failure and measurement of ANP, NT-proANP, or MR-proANP in blood or urine. Those criteria were fulfilled by 19 publications which reported pediatric ANP levels and are presented in Tables 1, 2. Another 3 studies determined MR-proANP or NT-proANP. All of them mainly evaluated the association between elevated ANP levels and diagnosis, severity, or etiology of heart failure as well as correlation with hemodynamic parameters, age or medical/surgical intervention.
Figure 1. Literature search strategy.
Table 1. Overview of ANP levels in pediatric heart failure sorted in order of increasing age of diseased children in each section.
Table 2. ANP levels influenced by medical or surgical intervention sorted in order of increasing age.
Therapeutic Implications Of The Reduced Effectiveness Of The Natriuretic Peptide System In Chronic Heart Failure
Recently, several pharmacological approaches have been explored with the aim of enhancing the effectiveness of the NPS in patients with CHF .
| Effects onplasma NPs | |
|---|---|
| Renin PRA, Aldosterone |
- ACE, angiotensin-converting enzyme ANG II, angiotensin II ANP, atrial natriuretic peptide BNP, brain natriuretic peptide cGMP, cyclic guanosine monophosphate NPs, natriuretic peptides PRA, plasma renin activity RAAS, reninangiotensinaldosteronesystem.
You May Like: Benadryl Heart Arrhythmia
Atrial Natriuretic Peptide Treatment After Reperfusion Therapy In Patients With Acute Myocardial Infarctionclinical Findings
In the acute phase of AMI, NTG has been reported to have a favourable effect in preventing LV remodelling. However, NTG may stimulate the RAAS despite its beneficial haemodynamic effect. In contrast, ANP has a wide range of cardioprotective effects, including the inhibition of RAAS and sympathetic nerve activity, as described in the previous sections. We and others have investigated the efficacy of intravenous ANP in patients with AMI.,, These studies are summarized below.
In another study, Kuga et al. evaluated the effects of ANP on myocardial reperfusion injury and LV remodelling. Nineteen patients presenting within 12 h of a first AMI underwent intracoronary injection of 25 µg of ANP immediately after coronary angioplasty, combined with intravenous infusion of 0.025 µg/kg/min of ANP initiated on admission and continued for 1 week . Eighteen similar patients were treated with saline . The incidences of reperfusion injury including premature ventricular contraction, VT and/or fibrillation, in the ANP group were significantly less than in the control group after coronary angioplasty. The incidence of ST-segment elevation in the ANP group was also significantly less than in the control group .
Effect of ANP administration on the number of premature ventricular contractions, the incidence of ventricular tachycardia and/or ventricular fibrillation and the incidence of persistent ST elevation
| . |
|---|
Prevalence And Causes Of Increased Bnp Or Nt
BNP and NT-pro-BNP are frequently elevated in patients with CKD. In a survey of asymptomatic patients who had CKD and did not yet require dialysis, more than half of the patients were noted to have elevated NT-pro-BNP levels. In patients who had ESRD and received hemodialysis or peritoneal dialysis , BNP and NT-pro-BNP levels were almost invariably increased compared with the normal cutoff values. One of the major contributing factors for the markedly elevated BNP and NT-pro-BNP levels in this population is the very high prevalence of LV structural and functional abnormalities. BNP and NT-pro-BNP levels are strongly associated with LV hypertrophy and systolic dysfunction in patients who have ESRD and are on maintenance HD or PD., Similar findings were reported in nondialysis CKD populations., , In the study by Takami et al., plasma BNP was a reliable marker of LV overload and had powerful predictive potential for heart failure in nondialysis patients with CKD. BNP or NT-pro-BNP elevation also reflected the presence of myocardial ischemia in asymptomatic patients with CKD., Likewise, higher BNP and NT-pro-BNP levels were observed in both HD and PD patients with underlying coronary artery disease.,
Recommended Reading: Does Benadryl Lower Heart Rate
