A History Part I: Pattern Recognition:
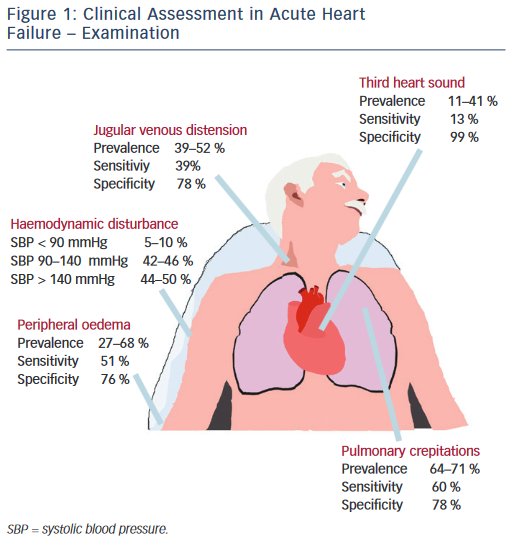
A patient with AHF typically presents with some combination of increased congestion and, less frequently, decreased peripheral perfusion. In addition to disturbances in oxygenation due to pulmonary edema, renal dysfunction is a frequent manifestation of AHF and reflects the multisystem nature of this disease.
The mean age of patients with AHF is in the mid-70s, with about half of each sex and the majority with normal or elevated blood pressure.
Most frequent symptoms at presentation:
-
Dyspnea
-
Fatigue
-
Abdominal discomfort
-
Leg pain
-
Sleep disturbances
The typical patient presents with signs and symptoms of congestion, usually with some combination of lower extremity edema and pulmonary congestion, normal or elevated blood pressure and heart rate, and compromised oxygenation proportional to the extent of the pulmonary edema. A significant minority of patients may manifest worsening of their heart failure with predominantly abdominal congestion symptoms and signs, rather than lower extremity edema.
Other patients, often elderly with hypertension, can present with rapid, if not fulminant, pulmonary edema with no or mild increase in total body fluid. Patients with recurrent heart failure exacerbations tend to recapitulate their clinical presentations in subsequent episodes, so obtaining a history of the time course, triggers, signs and symptoms, and response to therapy of prior events can increase the sensitivity to early decompensation.
What Is Acute Heart Failure Heres What You Need To Know
If ever there were a prize awarded for most misleading name given to a medical condition, heart failure would win hands down.Heart failure is a terrible name which suggests the heart has stopped working completely, says Anthony Steimle, MD, a cardiologist and assistant physician in chief of cardiovascular services at Kaiser Permanente in Santa Clara, California. In fact, the heart has not stopped working. The heart muscle, however, is damaged.Specifically, the heart can become weak and unable to pump blood , or the heart can become stiff and unable to fill with blood adequately .Some people may not even realize they have heart failure, blaming the subtle symptoms on aging or being out of shape. Yet, according to the Heart and Stroke Foundation, about 600,000 Canadians are living with heart failure.Heart disease is the second leading cause of death in Canada. And yet, surprisingly, it is largely preventable.Over time, however, unhealthy lifestyle choices and poorly controlled diseases such as diabetes contribute to heart failure. Heart failure can be progressive, leading to persistent illness, becoming life-threatening, and sometimes requiring advanced therapies including heart transplantation or mechanical device support, says Michele Hamilton, MD, director of the Heart Failure Program in the Smidt Heart Institute at Cedars-Sinai, in Los Angeles.
What is acute heart failure?
Symptoms of acute heart failure
Risks for heart failure
Types of heart failure
What You Can Do
Although some risk factors of heart failure, like age, cant be modified, people with CHF can take actions to improve their long-term prognosis. The first step is to become familiar with any family history of heart disease and learn about all the possible symptoms. Don’t ignore suspicious symptoms: let your doctor know about them. Regular exercise and managing concurrent conditions can also help keep CHF under control.
Also Check: Ibs And Palpitations
What Are Acute Heart Failure Symptoms
Acute heart failure symptoms are very similar to the symptoms of chronic heart failure. Nonetheless, these symptoms may be more severe or pronounced with acute heart failure, though.
The symptoms are the following:
- Shortness of breath: It is the most common symptom of acute heart failure. This can happen while making minimum efforts or while lying in bed.
- Swelling: Legs and abdomen may suddenly swell, and patients can rapidly gain weight from retaining fluid.
- Nausea
- Fatigue to minimum efforts or while resting
- Abnormal heart rhythms or a fast heartbeat
- A decrease in the ability to concentrate
- Spitting up pink phlegm
- Veins in the neck become bigger
- The coolness in hand and feet due to a decrease in the cardiac output
- Fainting
- Blue/colored lips, skin or tongue, also called central cyanosis
- Congestion in the kidneys may lead to renal dysfunction. This causes less urine throughout the day and frequent urination during the night.
Outlook For Heart Failure
Heart failure is a serious long-term condition that’ll usually continue to get slowly worse over time.
It can severely limit the activities you’re able to do and is often eventually fatal.
But it’s very difficult to tell how the condition will progress on an individual basis.
It’s very unpredictable. Lots of people remain stable for many years, while in some cases it may get worse quickly.
Read Also: Does Benadryl Lower Heart Rate
Is Acute Heart Failure Curable
Acute heart failure is the sudden onset or worsening of existing chronic heart failure. Towards this specific condition, there is no definitive cure. However, the doctor may indicate treatment for managing the symptoms and prevent the worsening of the disease.
It is essential to know that this condition is the worsening of previous symptoms. Besides, it is a manageable and preventable condition, but it has no definitive cure.
Nonetheless, HF patients who receive appropriate medical attention quickly may have a very good clinical outcome. The time in this condition plays a significant role, so people should be aware of warning symptoms.
Hospitalized patients will be in observation after managing the symptoms to see how they respond to the treatment. The treatment includes several drugs to compensate for fluid overload like intravenous diuretics. This is a potentially deadly condition, so it must be taken seriously and also takes into consideration the possible outcomes of the disease.
How Can I Improve My Quality Of Life With Heart Failure
There are several things you can do to improve your quality of life if you have heart failure. Among them:
- Eat a healthy diet. Limit your consumption of sodium to less than 1,500 milligrams each day. Eat foods high in fiber. Limit foods high in trans fat, cholesterol, and sugar. Reduce total daily intake of calories to lose weight if necessary.
- Exercise regularly. A regular cardiovascular exercise program, prescribed by your doctor, will help improve your strength and make you feel better. It may also decrease heart failure progression.
- Don’t overdo it. Plan your activities and include rest periods during the day. Certain activities, such as pushing or pulling heavy objects and shoveling may worsen heart failure and its symptoms.
- Prevent respiratory infections. Ask your doctor about flu and pneumonia vaccines.
- Take your medications as prescribed. Do not stop taking them without first contacting your doctor.
- Get emotional or psychological support if needed. Heart failure can be difficult for your whole family. If you have questions, ask your doctor or nurse. If you need emotional support, social workers, psychologists, clergy, and heart failure support groups are a phone call away. Ask your doctor or nurse to point you in the right direction.
Read Also: Benadryl Arrhythmia
When To Get Medical Advice
See a GP if you experience persistent or gradually worsening symptoms of heart failure.
Call 999 for an ambulance or go to your nearest A& E department as soon as possible if you have sudden or very severe symptoms.
A number of tests can be used to help check how well your heart is working, including blood tests, an ECG and an echocardiogram.
A Appropriate Prophylaxis And Other Measures To Prevent Readmission
An episode of AHF often can be seen as representing a failure of outpatient CHF management. It is imperative that this admission be viewed as an opportunity to prevent future decompensations through active education handouts and checklists without individual instruction are rarely effective. This education should include, but not be limited to, instruction on:
-
Low-salt and weight loss diets
-
Daily use of a scale and a mechanism to record body weights, including directions on the specific actions to take in the event of a change in body weight
-
Self-titration of diuretics, in appropriate patients. For example, if weight increases by 3 to 5 lb above baseline, double the diuretic dose for 3 to 5 days. If body weight returns to baseline, resume prior dose of diuretics. If symptoms of hypotension ensue, hold diuretics, and if the symptoms of hypotension do not resolve, call care provider. If weight does not improve or if increasing symptoms of dyspnea or other symptoms of congestion, call a care provider.
-
Chronic heart failure management programs, if available
-
Exercise or rehabilitation program
-
Other health-related issues such as smoking cessation
Also Check: Does Benadryl Increase Heart Rate
What Is The Difference Between Acute Heart Failure And Chronic Heart Failure
As the name says, the difference can be pretty straightforward, one of them is a sudden event, and the other is a progressive condition.
Acute heart failure is when a patient develops suddenly new symptoms or the worsening of previously existing symptoms. On the other hand, chronic heart failure is a progressive condition that affects the heart muscle causing it not to pump blood in an effective way.
Moreover, acute heart failure can happen after a sudden event like a heart attack. And, it is essential to note that chronic heart failure comes after the patient develops acute heart failure for the first time.
Chronic heart failure can also happen when the heart overworks. The latter term occurs when conditions like high blood pressure cause the heart to pump harder than usual. This leads to progressive changes in the left heart, enlarging the muscle, and raising blood and oxygen needs.
Chronic heart failure can happen without previous heart infarction. The heart will go through a process of changes that will ultimately lead to pressure changes within it. Of course, this can lead to life-threatening conditions as well.
Finally, it is important to have in mind that despite both of them having different times of onset, both lead to the same changes in the heart.
Classification Of Acute Heart Failure
The definition of AHF presented here is broad and there have been many attempts to stratify this further . Although characterised by a distinctive set of signs and symptoms, a major challenge in classifying AHF as a single entity is that the patient population is not uniform. Patients admitted with HF exhibit a wide spectrum of disease and range from those with severe LV systolic dysfunction and low cardiac output to those with severe hypertension and normal or near-normal LV systolic function. The majority of patients with AHF lie between these extremes and therefore also demonstrate a distribution of underlying pathology and precipitants, leading to the common endpoint of fluid overload.
This is a neat classification system and focusses the treating physician towards the management of the underlying cause of AHF. However, given patients often present with a range of co-morbidities, the reasons for decompensation may not be apparent at initial presentation or indeed, there may be multiple contributing factors. Practically speaking, therefore, it may be more prudent to stratify patients with AHF based on their initial clinical presentation. This allows the attending physician to identify those most at risk in order to direct specific interventions such as instituting ionotropic agents and/or mechanical circulatory support.
Also Check: What Is A Dangerously High Heart Rate
Financial Burden Of Ahf
HF inflicts a huge financial burden that represents 2% of the total healthcare expenditure , . In USA, the estimated cost for HF in 2012 was $30.7 billion and there is a projected 3-fold increase in 2030, leading to a total of 160 billion annual cost . This enormous financial burden associated with HF results from, the recurrent admissions, the multiple treatment choices from drugs to devices and heart transplantation combined with the fact that HF is the end-stage condition of possibly all types of cardiovascular diseases in an aged population. An interesting way of understanding how huge is the burden of HF, is by approaching the socioeconomic burden of HF comparatively with the burden of cancer . Both the social impact as it is shown by the incidence of cancer and HF and the financial impact as it is reflected on the annual cost , can lead us safely to the conclusion that we should approach HF in multiple ways .
How Is Acute Heart Failure Diagnosed
Healthcare providers perform a rapid assessment that includes:
- Your health history, including your personal or family history of heart disease. Theyll want to know about other health conditions like whether you use tobacco products and any medications you take.
- A physical exam to learn more about your symptoms and how severe they are. This includes listening to your heart and checking for signs of edema.
Read Also: How To Find Thrz
Risks For Heart Failure
Aging is the primary risk factor for heart failure. While you can’t stop aging, you do hold the power to lower and manage most of the other risks.
“It is important to recognize that for much of heart disease, prevention and the motivation to prevent heart disease is critical,” says Manesh Patel, MD, chief of the division of cardiology and co-director of the Duke Heart Center at Duke University School of Medicine in Durham, North Carolina. “For example, patients with hypertension or diabetes may not immediately feel bad. But control of hypertension and/or diabetes will prevent their heart from developing heart failure that is symptomatic and/or potentially worsening.”
Less Common Symptoms Of Acute Heart Failure
Not everyone will experience the following symptoms of acute heart failure. Some of these symptoms are caused by an underlying condition. Less common symptoms of acute heart failure include:
- Palpitations, the feeling that the heart has skipped or added a beat, where the person has arrhythmia
- Fever, which can be caused by underlying infection
- Fainting, also called syncope
- Blue/colored lips, skin or tongue, also called central cyanosis
You May Like: Can Flonase Cause Heart Palpitations
Chronic Obstructive Pulmonary Disease
People with , most commonly or , frequently have chronic shortness of breath and a chronic productive cough. An presents with increased shortness of breath and production. is a risk factor for thus this condition should be ruled out. In an acute exacerbation treatment is with a combination of , , and possibly .
Diagnosis Of Heart Failure Of Acute Onset
|
Data from Ponikowski P, Voors AA, Anker SD, et al: 2016 ESC Guidelines for the diagnosis and treatment of acute and chronic heart failure: The Task Force for the diagnosis and treatment of acute and chronic heart failure of the European Society of Cardiology Developed with the special contribution of the Heart Failure Association of the ESC. European Heart Journal 37:2129-2200, 2016. doi: 10.1093/eurheartj/ehw128 |
Don’t Miss: How Do You Say Heart Attack In Spanish
Heart Failure Treatment Is A Team Effort
Heart failure management is a team effort, and you are the key player on the team. Your heart doctor will prescribe your medications and manage other medical problems. Other team members — including nurses, dietitians, pharmacists, exercise specialists, and social workers — will help you achieve success. But it is up to YOU to take your medications, make dietary changes, live a healthy lifestyle, keep your follow-up appointments, and be an active member of the team.
If you notice anything unusual, don’t wait until your next appointment to discuss it with your doctor. Call them right away if you have:
- Unexplained weight gain
- Swelling in your ankles, feet, legs, or belly that gets worse
- Shortness of breath that gets worse or happens more often, especially if you wake up feeling that way
- Bloating with a loss of appetite or nausea
- Extreme fatigue or more trouble finishing your daily activities
- A lung infection or a cough that gets worse
- Fast heart rate
- New irregular heartbeat
What Are The Possible Complications Of Acute Heart Failure
- Complications may arise in other organs and systems of the body due to acute heart failure.
- In most cases, heart failure reduced blood flow to the kidneys. Without treatment this can cause severe damage and result in kidney failure.
- Fluid buildup in the heart can cause complications within the heart valves. If too much fluid is built up, the valves become stretched and damage resulting in abnormal blood flow to and from the heart.
- Fluid buildup can also cause pressure to build up against the liver, resulting in liver damage. If it becomes excessive, scarring may result that impairs liver functioning.
- Blood clots may also develop as a result of acute heart failure. In people with AHF, blood does not flow through the heart as quickly as it normally would. This increases the likelihood of blood clots forming and may result in a heart attack or stroke.
Don’t Miss: Does Benadryl Lower Heart Rate
De Novo Acute Heart Failure
Acute heart failure is broadly defined as a rapid onset of new or worsening signs and symptoms of HF . It is often a potentially life-threatening condition, requiring hospitalisation, and emergency treatment is aimed predominantly at managing fluid overload and haemodynamic compromise. This umbrella term includes patients presenting for the first time with typical symptoms and signs of heart failure and also those with worsening of their pre-existing cardiomyopathy .
De novo AHF occurs when there is a sudden increase in intracardiac filling pressures and/or acute myocardial dysfunction which can lead to decreased peripheral perfusion and pulmonary oedema. The most common aetiology is cardiac ischaemia where -total coronary occlusion leads to decreased contractility in myocardium subtended by the affected coronary artery. In this case, management is focussed not only on haemodynamic compromise but also on reperfusion with the aim of restoring myocardial contractile function.
In addition to myocardial dysfunction, AHF can be precipitated by acute valvular incompetence. This most commonly occurs in an ischaemic context leading to acute mitral regurgitation but can also occur without ischaemia per se as is the case with infective and non-bacterial thrombotic endocarditis. Extra-cardiac pathologies may also precipitate AHF as is the case with pulmonary embolism or pericardial effusion causing tamponade, both of which reduce LV output and therefore reduce peripheral perfusion
