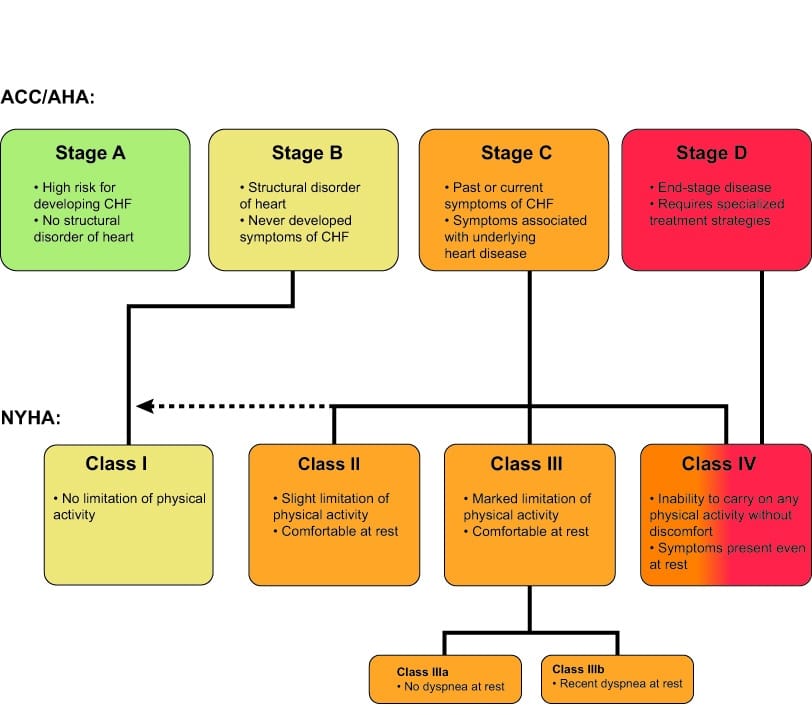
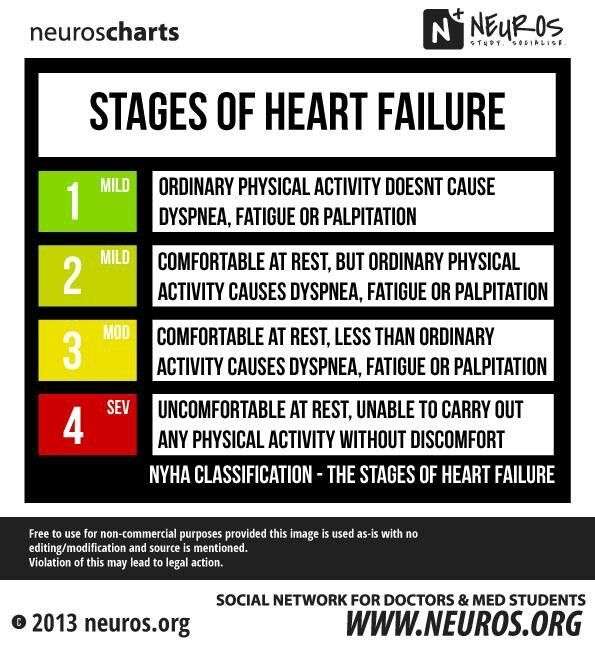
Congestive Heart Failure Is A Type Of Heart Failure Which Requires Seeking Timely Medical Attention Although Sometimes The Two Terms Are Used Interchangeably View An Animation Of Heart Failure This Table Lists The Most Heartfailure Affects People To Varying Degrees The New York Heart Association Has Categorized Each Of The Diagnosis Into Four Classifications Class I And Class Ii Are Considered Mild Class Iii Is Considered Moderate And Class Iv Is Severe The Following Is An Explanation Of The Four Classes Of Heartfailure And The Results Associated With Note: The Stages Classified By The Aha And Acc Are Different From The New York Heart Association Clinical Classifications Of Heart Failure Heartfailure
- Heart failure is a clinical syndrome characterized by symptoms of effort intolerance and/or signs of fluid retention … Atherton J Stage B Heart Failure: Rationale for Screening, Heart Failure
- Stages of Congestive Heart Failure Stage B. Stage two of congestive heart failure will produce symptoms such as fatigue, shortness of breath, or heart palpitations after you participate in physical activity. As with stage one, lifestyle changes and certain medication can help improve your quality of life.
- Congestive heartfailure is a clinical condition in which the heart is unable to pump enough blood to meet the metabolic needs of the body because of Heartfailure : a complex of signs and symptoms caused by structural or functional impairment of ventricular filling and/or ejection of blood .
- During the early stagesofheartfailure, dyspnea usually occurs only during physical activity, but later dyspnea could occur even at rest. Patients with low output heartfailure could present with altered sensorium and this might be one of the foremost complaints offered by the patient or the family.
- Heart failure is a condition in which the heart does not pump enough blood and oxygen to the organs and tissues of the body. As a result, the organs in the body do not get the blood they need and fluids back up in the body. Heart failure does not mean the heart has stopped beating it simply means the heart has failed to work as it should.
Heart Failure Criteria Classification And Staging
Guideline contributor: Henry H Ooi, MD, MRCPI, Director, Advanced Heart Failure and Cardiac Transplant Program, Nashville Veterans Affairs Medical Center Assistant Professor of Medicine, Vanderbilt University School of Medicine.
Heart failure criteria, classification, and staging
Framingham classification
In the Framingham classification, the diagnosis of heart failure is based on the concurrent presence of either two major criteria or one major and two minor criteria.
Major criteria comprise the following:
- Paroxysmal nocturnal dyspnea
- Weight loss of 4.5 kg or more in 5 days in response to treatment
- Neck vein distention
- Central venous pressure greater than 16 cm water
- Circulation time of 25 seconds or longer
- Radiographic cardiomegaly
- Pulmonary edema, visceral congestion, or cardiomegaly at autopsy
Minor criteria are as follows:
- Nocturnal cough
- A decrease in vital capacity by one third the maximal value recorded
- Pleural effusion
- Bilateral ankle edema
New York Heart Association classification
The NYHA functional classification of heart failure is widely used in practice and in clinical studies. It is based on symptom severity and the amount of exertion needed to provoke symptoms. NYHA heart failure classes are as follows :
American College of Cardiology Foundation/American Heart Association staging systems
The 2013 ACCF/AHA staging system complements the NYHA classification to reflect the progression of disease and comprises four stages, as shown in Table 3. below.
Heart Failure Society Of America Recommendations For Genetic Evaluation Of Cardiomyopathy
Note the following :
- For all patients with cardiomyopathy, obtain a detailed family history for at least 3 generations
- Carefully assess the patient’s medical history as well as that of asymptomatic first-degree relatives, with special focus on heart failure symptoms, arrhythmias, presyncope, and syncope.
- Screen asymptomatic first-degree relatives for cardiomyopathy
- Screen for cardiomyopathy at intervals in asymptomatic at-risk relatives who are known to carry the disease-causing mutation 00174-0/fulltext#sec18.1″ rel=”nofollow”> HFSA Guideline Approach to Medical Evidence for Genetic Evaluation of Cardiomyopathy )
- Screen for cardiomyopathy in asymptomatic at-risk first-degree relatives who have not undergone genetic testing or in whom a disease-causing mutation has not been identified.
Note: Due to the complexity of genetic evaluation, testing, and counseling of patients with cardiomyopathy, it is recommended that patients be referred to centers with expertise in these matters and in family-based management.
Recommended Reading: What Is The Closest Thing To A Magic Bullet Against Heart Disease
Areas Of Focus Include:
Management strategies in stage C HF, including:
New treatment strategies in HF, including sodium-glucose cotransporter-2 inhibitors and angiotensin receptor-neprilysin inhibitors .
Management of HF and atrial fibrillation , including ablation of AF.
Management of HF and secondary MR, including MV transcatheter edge-to-edge repair.
Left ventricular assist device use in stage D HF.
The intended primary target audience consists of clinicians who are involved in the care of patients with HF. Recommendations are stated in reference to the patients and their condition. The focus is to provide the most up-to-date evidence to inform the clinician during shared decision-making with the patient. Although the present document is not intended to be a procedural-based manual of recommendations that outlines the best practice for HF, there are certain practices that clinicians might use that are associated with improved clinical outcomes.
In developing the 2022 HF guideline, the writing committee reviewed previously published guidelines and related statements. contains a list of these guidelines and statements deemed pertinent to this writing effort and is intended for use as a resource, thus obviating the need to repeat existing guideline recommendations.
Table 1 Associated Guidelines and Statements
Statements
The full SIHD guideline is from 2012 . A focused update was published in 2014 .
Management Of Acute Decompensated Heart Failure
The Heart Failure Society of America guidelines recommend the following treatment goals for patients with acute decompensated heart failure :
- Symptomatic improvement
- Restoration of normal oxygenation
- Identification of the etiology and addressing precipitating factors
- Optimization of long-term oral therapy
- Minimization of side effects
- Identification of patients in whom revascularization or device therapy may be beneficial
- Risk stratification for venous thromboembolism and potential need for anticoagulation
- Patient education regarding medications and self-management of heart failure
- Initiation of a disease management program, where possible
HFSA indications for hospital admission in patients with ADHF are as follows :
- Evidence of severely decompensated heart failure, including hypotension, worsening renal function, and altered mentation
- Dyspnea at rest
- Hemodynamically significant arrhythmia, including new onset of rapid atrial fibrillation
- Acute coronary syndromes
The American College of Cardiology Foundation/American Heart Association comments regarding adjustment of maintenance heart failure medications in patients admitted with ADHF are as follows:
Recommended Reading: What I Felt Before My Heart Attack
Acc Aha Hfsa 2022 Heart Failure Management Guidelines: A Guideline Topline
The new HF guidelines prioritize primary prevention, revise disease stages to encourage early intervention, and now include SGLT2i as guideline-directed medical therapy.
The new 2022 guidelines on management of heart failure reflect a unique collaboration between the American College of Cardiology, American Heart Association, and the Heart Failure Society of America.
The new recommendations retain and combine elements from guidelines published in 2013 and 2017 and, based on extensive review of new data, include important evidenc-based additions and revisions. Top among the new recommendations is a Class 2a recommendation for use of SGLT-2 inhibitors in HFpEF and revised ACC/AHA stages of heart failure.
For primary care clinicians the revised staging of heart failure reinforces a primary focus of the new guidlines on prevention of heart failure thus the new Stage A: At-risk for heart failure emphasizes early identification of and treatment to reduce risk factors that include a range of cardiometabolic disease.
The Guideline Topline that follows includes the new stages of heart failure and a quick look at the 10 topline guidlines take-home points identified by the writing committe.
ACC/AHA/HFSA Stage A: At risk for heart failure
CVD, cardiovascular disease
Selection Of Writing Committee Members
The Joint Committee strives to ensure that the guideline writing committee contains requisite content expertise and is representative of the broader cardiovascular community by selection of experts across a spectrum of backgrounds, representing different geographic regions, sexes, races, ethnicities, intellectual perspectives/biases, and clinical practice settings. Organizations and professional societies with related interests and expertise are invited to participate as partners or collaborators.
Read Also: Open-heart Surgery Survival Rate 2020
New Hf Definition Stage Updates Outlined In 2022 Acc/aha/hfsa Guidelines
The new guidelines also call for better incorporation and addressing of social determinants of health.
During a panel at the American College of Cardiologys 70th Scientific Session, experts highlighted updates to the 2022 American Heart Association /ACC/Heart Failure Society of America guidelines for the management of heart failure and offered a new definition of the condition.
The syndrome of HF is defined as a complex clinical syndrome with symptoms and signs that result from structural or functional impairment, said Biykem Bozkurt, MD, PhD, guideline writing committee vice-chair and professor of Medicine-Cardiology at Baylor College of Medicine.
With regard to terminologies for HF trajectory, the guidelines emphasized the use of persistent HF as opposed to stable HF, as the term stable creates inertia, while persistent HF requires optimization, Bozkurt added. The phrase HF in remission is also preferred over HF in recovery as the majority of patients who withdraw from therapy will relapse.
Among the updates included are a redefinition of HF stages to emphasize prevention and the addition of sodiumglucose co-transporter 2 inhibitors for the treatment of symptomatic HF.
This latter inclusion comes off the heels of an FDA approval for empagliflozin, for a broader range of patients with HF, including those with preserved ejection fraction a condition with a poor prognosis and very limited treatment options.
What Do The Classifications Really Mean
Heart failure is staged and classified by healthcare providers but what do they really mean. HF exists along a continuum. It can go from non-existent to mild to moderate to advanced, all over a period of time. Managing heart failure depends on the stage and can include the use of medications, lifestyle behaviors, and cardiac devices.
Mild heart failure may be evident when you experience minimal symptoms, such as shortness of breath, when involved in certain kinds of physical activity or maybe present without any symptoms. With early diagnosis, lifestyle changes, and medication, people with mild to moderate heart failure generally lead normal lives. Moderate heart failure is often classified along with mild HF. The same treatment approach is indicated.
Refractory congestive heart failure occurs when symptoms continue to be present even after routine treatment. This is also called advanced heart failure or end-stage heart failure. It occurs when a person is not responding to or getting worse despite treatment.
Read Also: How Many Heart Attacks Did Dick Cheney Have
The New York Heart Association Classifies The Stages Of Heart Failure As Follows: 2
No limitation of physical activity. Ordinary physical activity does not cause undue fatigue, palpitation, dyspnea .
Slight limitation of physical activity. Comfortable at rest. Ordinary physical activity results in fatigue, palpitation, dyspnea .
Unable to carry on any physical activity without discomfort. Symptoms of heart failure at rest. If any physical activity is undertaken, discomfort increases.
Can Heart Failure Progression Be Stopped
Once you move on to the next stage, you cant go back even with treatment. However, if caught early, its possible to delay or stop disease progression with lifestyle changes and medications. If you have risk factors of heart failure, discuss with your doctor how best to prevent developing the condition.
Recommended Reading: How Dangerous Is Open Heart Surgery
Atrial Fibrillation And Sinus Rhythm
New recommendation to 2009 update: It is reasonable to treat patients who have atrial fibrillation and heart failure with strategies to maintain sinus rhythm or to control ventricular rate alone. Four trials evaluated the effectiveness and safety of restoring and maintaining sinus rhythm in patients with atrial fibrillation. There were equivalent outcomes for restoring and maintaining sinus rhythm by electrical or pharmacologic conversion compared with controlling ventricular rate in patients with atrial fibrillation. Most patients quickly relapse to atrial fibrillation unless they are treated with a class I or III antiarrhythmic medication, but patients with heart failure are not likely to respond favorably to class I medications. Class III antiarrhythmic medications can maintain sinus rhythm in some patients, although treatment is associated with an increased risk of organ toxicity and proarrhythmia .
New Acc/aha/hfsa Guideline Redefines Heart Failure Stages To Focus On Prevention Updates Treatment Options And Emphasizes Care Coordination With A Heart Failure Specialty Team
Contact: Sam Roth, [email protected],
WASHINGTON and DALLAS –
A new joint guideline published today from the American College of Cardiology, the American Heart Association, and the Heart Failure Society of America, increases the focus on preventing heart failure in people who are showing early signs of pre-heart failure, and updates treatment strategies for people with symptomatic heart failure to include SGLT-2 inhibitor medicines. The guideline also offers recommendations for managing cardiac amyloidosis, cardio-oncology complications, comorbidities in the setting of heart failure, as well as consideration for implantable devices and advanced therapies for people with stage D heart failure.
Heart failure is a chronic condition that is usually manageable with medication and lifestyle changes. The most common causes of heart failure include narrowed heart arteries, heart attack, high blood pressure and valvular heart disease. Other causes can include, but are not limited to, familial or genetic cardiomyopathies, amyloidosis, metabolic disease, autoimmune disorders or exposure to cardiotoxic agents, such as chemotherapy or other medications. Primary prevention is important for those at risk of HF or pre-HF.
New York Heart Association classification is used when people reach symptomatic or advanced HF, to describe their functional capacity and determine treatment strategies.
Additional Resources:
Don’t Miss: What Is Too High Of A Heart Rate
Acc/aha Heart Failure Staging
- Patients with known heart failure.
- Patients at risk for heart failure.
- Developed jointly by the American College of Cardiology and American Heart Association to complement, but not replace, the more widely-used New York Heart Association functional classification.
- Based on expert consensus.
- Matches stage to treatment options, unlike other classification systems.
- Other heart failure classification systems include Forrester Class and NYHA Class.
- Unlike other classification systems, the ACC/AHA stages include patients at risk for heart failure and corresponding management options.
How Long Can A Person Live With Stage 4 Congestive Heart Failure
Although there have been recent improvements in congestive heart failure treatment, researchers say the prognosis for people with the disease is still bleak, with about 50% having an average life expectancy of less than five years. For those with advanced forms of heart failure, nearly 90% die within one year.
Recommended Reading: What Are Symptoms Of Heart Attack
Ology And Evidence Review
The recommendations listed in this guideline are, whenever possible, evidence based. An initial extensive evidence review, which included literature derived from research involving human subjects, published in English, and indexed in MEDLINE , EMBASE, the Cochrane Collaboration, the Agency for Healthcare Research and Quality, and other selected databases relevant to this guideline, was conducted from May 2020 to December 2020. Key search words included but were not limited to the following: heart failure heart failure with reduced ejection fraction heart failure with preserved ejection fraction heart failure with mildly reduced ejection fraction systolic heart failure heart failure rehabilitation cardiac failure chronic heart failure acute decompensated heart failure cardiogenic shock beta blockers mineralocorticoid receptor antagonists ACE-inhibitors, angiotensin and neprilysin receptor antagonist sacubitril valsartan angiotensin receptor antagonist Sodium glucose co-transporter 2 or SGLT2 inhibitors cardiac amyloidosis atrial fibrillation congestive heart failure guideline-directed medical therapy HFrEF diabetes mellitus cardiomyopathy cardiac amyloidosis valvular heart disease mitral regurgitation cardiomyopathy in pregnancy reduced ejection fraction right heart pressure palliative care.
American College Of Cardiology/american Heart Association/heart Failure Society Of America Recommendations For Genetic Evaluation And Testing
Genetic screening and counseling are recommended for first-degree relatives of selected individuals with genetic or inherited cardiomyopathies to detect cardiac disease and to encourage review of therapies for lowering HF progression and sudden death.
It is reasonable to refer select patients with nonischemic cardiomyopathy for genetic counseling and testing to identify conditions that could guide treatments for patients and family member.
You May Like: Dos And Don’ts After Heart Surgery
Cardiac Resynchronization Therapy/biventricular Pacing
The 2013 ACCF/AHA guidelines recommend CRT for patients in sinus rhythm or atrial fibrillation with a QRS duration of 120 ms or longer and an LVEF of 35% or less with persistent, moderate-to-severe heart failure despite optimal medical therapy. A 2012 update of ACC/AHA/HRS guidelines on CRT expanded class I indications to patients with NYHA class II symptoms and LBBB duration of 150 ms or longer. Additional CRT recommendations include :
- Patients with a reduced LVEF and a QRS of 150 ms or longer who have NYHA I or II symptoms
- Patients with a reduced LVEF who require chronic pacing and in whom frequent ventricular pacing is expected
- CRT is not recommended for patients with NYHA class I or II symptoms and non-LBBB pattern with a QRS duration shorter than 150 ms
- CRT is not indicated in patients who are not expected to survive for more than 1 year due to their comorbidities or frailty
The 2022 ACC/AHA/HFSA guidelines indicate an “upgrade” to CRT should be considered for patients with an LVEF of 35% or less who have received a conventional pacemaker or an ICD and who then develop worsening HF despite optimal medical therapy and who have a signficant proportion of RV pacing.
The ESC guidelines gives class I recommendations for the use of CRT in the following groups :
CRT should be considered for the following groups :
CRT may be considered for the following groups :
CRT is contraindicated in patients with a QRS duration below 130 ms.
