What Is Acute Decompensated Heart Failure Isnt It Just A Worsening Of Chronic Heart Failure
Acute decompensated heart failure is a clinical syndrome of worsening signs or symptoms of heart failure requiring hospitalization or other unscheduled medical care. For many years, ADHF was viewed as simply an exacerbation of chronic HF as a result of volume overload, with few implications beyond a short-term need to intensify diuretic therapy . Recent decades have seen an explosion of research into the epidemiology, pathophysiology, outcomes, and treatment of ADHF. Although some controversy persists, multiple lines of evidence now support the concept that ADHF is a unique clinical syndrome with its own epidemiology and underlying mechanisms and that there is a need for specific therapies. This viewpoint suggests that ADHF is not just a worsening of chronic HF any more than an acute myocardial infarction is just a worsening of chronic angina.
Outcome data from a variety of studies now support the concept that hospitalization for ADHF can often signal a dramatic change in the natural history of the HF syndrome. Rates of rehospitalization or death are as high as 50% within 6 months of the initial ADHF event, which is a much higher event rate than is seen with acute MI.
A schematic representation of the pathophysiology of acute HF is given in Fig. 26.1.
V. Courtney Broaddus MD, inMurray & Nadel’s Textbook of Respiratory Medicine, 2022
Receive The Best Care For Your Heart And Stay Safe With Dispatchhealth
Anyone with a history of heart disease knows the stress associated with this condition. What seems like minor symptoms for others, such as fatigue, can be especially scary when youre constantly on the lookout for symptoms related to your illness. When it comes to your heart, you should be assessed if you think something is wrong. DispatchHealth offers a better solution than travelling to an urgent care facility for non-life-threating situations. When heart failure exacerbations occur, DispatchHealth will come to you and evaluate the situation. Our experienced medical staff has the ability to use an EKG to assess heart rhythms and develop a treatment plan. To schedule an appointment, you can call, click here, or download our app.
If this is an emergency, please call 911 or go to the nearest emergency department.
Other Ways To Classify Heart Failure
Sometimes, doctors also identify types of heart failure based on whether you have known heart disease. These types are:
Acute decompensated heart failure
most common form of acute heart failure.
People with acute decompensated heart failure can sometimes have several conditions that affect their hearts, so it can be hard to know the exact cause of this type of heart failure.
De novo acute heart failure
De novo acute heart failure is less common. De novo is a medical term that means for the first time. This type describes heart failure when you do not have a previous diagnosis of heart disease.
Also Check: Prognosis Of Congestive Heart Failure
Diagnosis Of Acute Heart Failure
The diagnosis of acute heart failure in critically ill patients can be more difficult than is commonly recognised. Although the underlying pathology in most patients with acute heart failure on intensive care will be coronary artery disease, other diagnoses must be considered .
It is also important to reassess critically the patient referred with a diagnosis of acute heart failure to decide whether this is indeed the primary problem. The history, examination and initial investigations with routine blood tests, electrocardiogram and chest X-ray may be compatible with this diagnosis but many such patients are elderly with multiple co-morbidities, and deciding whether the patient is suffering from a primary myocardial pathology as opposed to a pulmonary problem or indeed systemic sepsis6 can be difficult. Equally, patients believed to have a primary respiratory problem may fail to wean from ventilatory support because of a failure to realise that they have left ventricular failure with a high left atrial pressure and incipient pulmonary oedema, causing a reduction in pulmonary compliance, an increased work of breathing and respiratory distress when ventilatory support is withdrawn.
Further investigations that can help to confirm or refute an initial diagnosis of acute heart failure are echocardiography and the measurement of biomarkers such as natriuretic peptides and cardiac troponins.
Peter S. Pang, Marco Metra, in, 2020
Classification Of Acute Heart Failure
The definition of AHF presented here is broad and there have been many attempts to stratify this further . Although characterised by a distinctive set of signs and symptoms, a major challenge in classifying AHF as a single entity is that the patient population is not uniform. Patients admitted with HF exhibit a wide spectrum of disease and range from those with severe LV systolic dysfunction and low cardiac output to those with severe hypertension and normal or near-normal LV systolic function. The majority of patients with AHF lie between these extremes and therefore also demonstrate a distribution of underlying pathology and precipitants, leading to the common endpoint of fluid overload.
This is a neat classification system and focusses the treating physician towards the management of the underlying cause of AHF. However, given patients often present with a range of co-morbidities, the reasons for decompensation may not be apparent at initial presentation or indeed, there may be multiple contributing factors. Practically speaking, therefore, it may be more prudent to stratify patients with AHF based on their initial clinical presentation. This allows the attending physician to identify those most at risk in order to direct specific interventions such as instituting ionotropic agents and/or mechanical circulatory support.
Also Check: Heart Attack In Young Women
Pathophysiological Mechanisms Of Ahf
An underlying structural or functional cardiac condition is a prerequisite for AHF and includes a multitude of different acute or chronic cardiac pathologies. The underlying cardiac disease leads to the activation of several pathophysiological pathways that counter the negative effects of HF on oxygen delivery to the peripheral tissues, but such pathways can also eventually cause systemic congestion, ventricular remodelling and organ dysfunction. Furthermore, some acute diseases can act as precipitating factors and trigger AHF either by directly impairing cardiac diastolic and/or systolic function or by further promoting systemic congestion. Systemic congestion has a major effect on the clinical presentation in the majority of patients with AHF and is a relevant determinant of multi-organ dysfunction occurring in AHF . The pathophysiology of AHF is heterogeneous, as it is greatly affected by the nature of the underlying cardiac disease. It is perhaps not surprising, therefore, that the responses to treatment may vary and that different patients may respond best to distinct treatment strategies that depend on the underlying pathophysiology.
Fig. 1: Schematic representation of possible pathophysiological mechanisms in AHF.
LV systolic and diastolic dysfunction
Fluid retention
Fluid redistribution
Causes Of Acute Heart Failure
Many conditions can weaken or damage the heart over time. This can lead to heart failure.
With chronic heart failure, your heart tries to adapt to the additional strain over time until it just cant adapt anymore. Thats when acute heart failure happens.
Its also possible for acute heart failure to happen even in people who otherwise seem healthy. There are a number of conditions that can put a sudden strain on your heart.
Causes of acute heart failure include:
- coronary artery disease, which can cause a narrowing of the arteries
- heart attack, which causes damage to the heart muscle and is often caused by coronary artery disease
- use of certain illegal drugs, such as cocaine
- chemotherapy and radiation treatments
In the United States, Black and Hispanic people receive heart failure diagnoses more often than people from other racial or ethnic groups. And Black people in the United States are also at the highest risk of dying from heart failure.
These trends are related to racism and inequities in healthcare, according to the American College of Cardiology.
To diagnose acute heart failure, your doctor will run certain tests. Your doctor can then identify your stage of heart failure, to help find the right treatment for you.
You May Like: Pictures Of Swollen Ankles Due To Congestive Heart Failure
Classes And Stages Of Heart Failure
If you receive a heart failure diagnosis, your doctor may use a classification system to tell you what stage of heart failure you have. This can help guide your treatment.
The is a symptom-based scale. It places heart failure in one of four categories:
- Class 1. You dont experience any symptoms at any time.
- Class 2. You can perform daily activities with ease but feel fatigued or short of breath when you exert yourself.
- Class 3. You have difficulty completing daily activities.
- Class 4. You have heart failure symptoms like shortness of breath even when youre at rest.
The American College of Cardiology/American Heart Association classification is a stage-based system. Its used to identify your risk for or level of heart failure. The letters A to D convey the stage that youre in:
- Stage A: At risk of heart failure. You have one or more risk factors for heart failure, but you arent experiencing any symptoms.
- Stage B: Pre-heart failure. Your test results show signs of heart disease, but you dont have symptoms of heart failure.
- Stage C: Symptomatic heart failure. You have heart disease, and youre experiencing symptoms of heart failure.
- Stage D: Advanced heart failure. You have advanced heart failure that affects your daily life and requires specialized treatments.
Doctors often use these two classification systems together to determine the best treatment or prevention plan for you.
Precipitating Causes Of Heart Failure
A previously stable, compensated patient may develop heart failure that is clinically apparent for the first time when the intrinsic process has advanced to a critical point, such as with further narrowing of a stenotic aortic valve or mitral valve. Alternatively, decompensation may occur as a result of the failure or exhaustion of the compensatory mechanisms but without any change in the load on the heart in patients with persistent, severe pressure or volume overload. In particular, consider whether the patient has underlying coronary artery disease or valvular heart disease.
The most common cause of decompensation in a previously compensated patient with heart failure is inappropriate reduction in the intensity of treatment, such as dietary sodium restriction, physical activity reduction, or drug regimen reduction. Uncontrolled hypertension is the second most common cause of decompensation, followed closely by cardiac arrhythmias . Arrhythmias, particularly ventricular arrhythmias, can be life threatening. Also, patients with one form of underlying heart disease that may be well compensated can develop heart failure when a second form of heart disease ensues. For example, a patient with chronic hypertension and asymptomatic LV hypertrophy may be asymptomatic until an MI develops and precipitates heart failure.
- Profound anemia
- Nutritional deficiencies
Also Check: Which Of The Following Helps Return Blood To The Heart
Precipitating Factors Of Ahf
The onset and increase in systemic congestion that precede AHF may develop over hours up to days, and can be triggered by several factors, either directly through stimulation of pathophysiological mechanisms leading to fluid accumulation or redistribution or indirectly through a worsening of cardiac diastolic or systolic function. The understanding of the pathophysiology involved in the development of AHF is important for providing the appropriate treatment. Although in many patients a progressive increase in body weight and pulmonary pressures may be observed as early as several days before hospital admission, in a relevant proportion of patients AHF is associated with only a minimal increase in body weight,. Several registries, including the North American OPTIMIZE-HF registry and the Euro-Asian registry of the GREAT network, have investigated the presence of precipitants in patients with AHF,. Acute coronary syndromes, arrhythmias , infections , uncontrolled hypertension and non-compliance with dietary recommendations and drug prescriptions are the most common identified precipitants,. Of note, in a relevant proportion of patients , no precipitants could be identified, whereas a combination of multiple factors were present in ~520% of patients,.
Management Of Acute Heart Failure Exacerbation
Heart failure has become the leading public health challenge faced by cardiovascular medicine today. In spite of medical and surgical advances, total mortality continues to rise, particularly in the older population. Although likely responsible for approximately 12 million outpatient visits per year, a more concerning fact is that heart failure now constitutes the most common hospital discharge diagnosis for patients older than age 65. This finding reflects the high incidence of the underlying conditionventricular dysfunctionand more importantly the frequency with which the disease results in clinical decompensation requiring inpatient medical care. As a result, critical care specialists likely will be exposed in the future to an increasing volume of patients with various forms and degrees of heart failure exacerbation. This article focuses primarily on the approach to patients presenting with an acute decompensation of established ventricular dysfunction, because the management of cardiogenic shock and acute myocardial infarction are addressed elsewhere in this issue.
Recommended Reading: Is Heart Rate Normal During Heart Attack
Initial Actions And Primary Survey
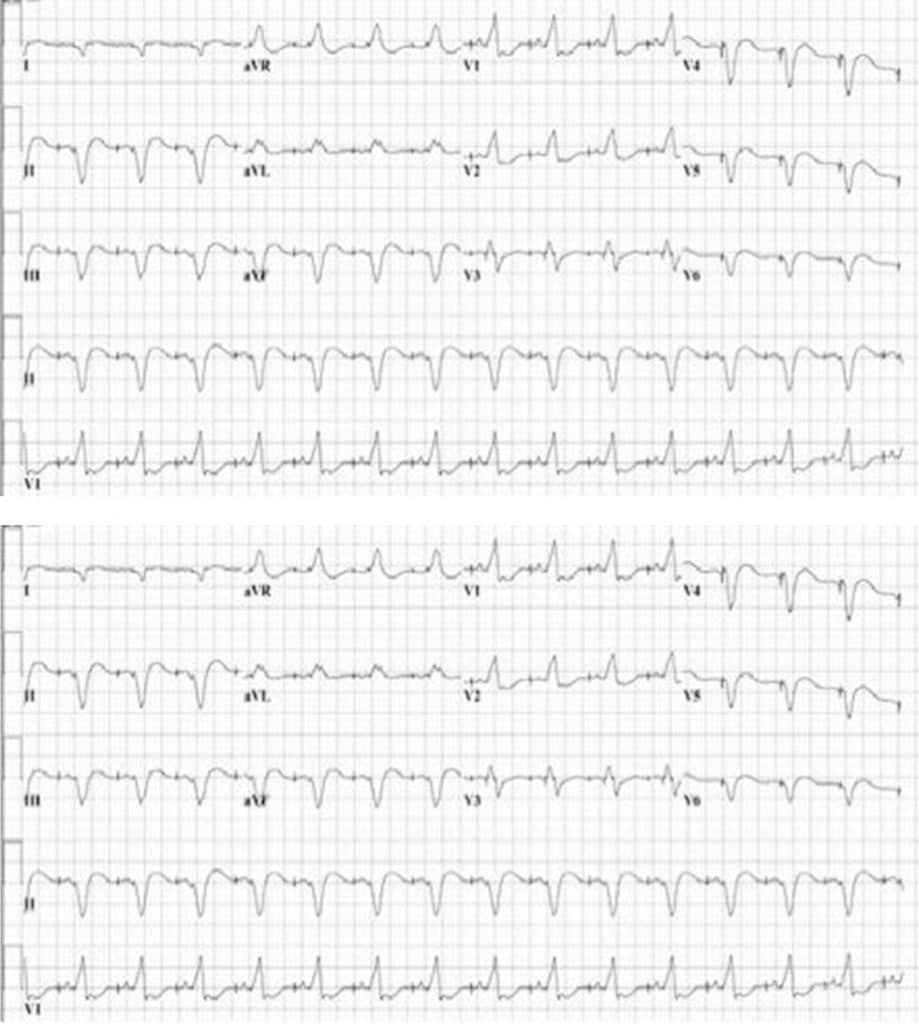
Similar to other patients in the Emergecny Department initial actions include establishing IV access,provding supplimental O2 as needed, and vital sign monitor. These patients may require ECG and CXR
If 100% O2 by non-rebreather fails to increase O2 saturation to at least 95%, noninvasive oxygenation/ventilation such as CPAP or BiPAP may assist in correcting hypoxia. If there is a failure to improve oxygenation, if the patient cannot tolerate the mask, or has a decline in mental status such that they are unable to protect their airway, then endotracheal intubation is required. The use of NIPPV used early can improve work of breathing as well as oxygenation, however caution should be taken as increased intra-thoracic pressure can reduce preload and worsen hypotension.
Hypotension can be difficult to manage in this patient population secondary to existing fluid overload. Early vasopressor support may be needed. Frequently patients with CHF exacerbation with present with significant hypertension. Nitroglycerin can be a useful medication in helping to reduce preload and reduce progression of pulmonary edema.
Myocytes And Myocardial Remodeling

In the failing heart, increased myocardial volume is characterized by larger myocytes approaching the end of their life cycle. As more myocytes drop out, an increased load is placed on the remaining myocardium, and this unfavorable environment is transmitted to the progenitor cells responsible for replacing lost myocytes.
Progenitor cells become progressively less effective as the underlying pathologic process worsens and myocardial failure accelerates. These featuresnamely, the increased myocardial volume and mass, along with a net loss of myocytesare the hallmark of myocardial remodeling. This remodeling process leads to early adaptive mechanisms, such as augmentation of stroke volume and decreased wall stress and, later, to maladaptive mechanisms such as increased myocardial oxygen demand, myocardial ischemia, impaired contractility, and arrhythmogenesis.
As heart failure advances, there is a relative decline in the counterregulatory effects of endogenous vasodilators, including nitric oxide , prostaglandins , bradykinin , atrial natriuretic peptide , and B-type natriuretic peptide . This decline occurs simultaneously with the increase in vasoconstrictor substances from the RAAS and the adrenergic system, which fosters further increases in vasoconstriction and thus preload and afterload. This results in cellular proliferation, adverse myocardial remodeling, and antinatriuresis, with total body fluid excess and worsening of heart failure symptoms.
You May Like: Does Caffeine Increase Heart Rate
Diagnosis And Treatment Of Acute Heart Failure
If any signs and symptoms of heart failure develop, especially if there has not been any previous diagnosis of heart failure, it is important to see a healthcare professional quickly. After performing a physical exam and obtaining information about current symptoms and your medical history, your doctor may order the following tests:
Heart Failure Doctor Discussion Guide
What Is Acute Heart Failure
Heart failure is a life-threatening condition. When it occurs, your heart is still working, but it cannot deliver oxygen-rich blood throughout your body. With acute heart failure, you experience a sudden, rapid decline in heart functioning and the amount of blood your heart can pump to the rest of your body.
You May Like: What Can Cause Heart Attack
Heart Failure Exacerbations: Definition Cause & Effect
A heart failure exacerbation is any abnormality associated with the muscles of the heart and/or its function. As a result, patients can experience a variety of symptoms that indicate the heart is compromised. The most common symptoms include:
- Shortness of breath
- Rapid heartbeat
- Excess coughing
Treatment for heart failure exacerbations includes the use of medications to improve the functionality of the heart. Beta blockers, ACE inhibitors, and vasodilators are common drugs used in the immediate treatment of heart issues. Long-term treatments may include the use of dietary supplements, diet modification, and any combination of vasodilators. Regular exercise may also reduce the risk of heart failure.
B What’s The Evidence For Specific Management And Treatment Recommendations
There are three main guidelines that address the treatment of patients with acute heart failure:
Lindenfeld, J, Albert, NM, Boehmer, JP. âHFSA 2010 comprehensive heart failure practice guidelineâ. J Card Fail. vol. 16. 2010. pp. e1-194. , and is updated.)
Hunt, SA, Abraham, WT, Chin, MH. â2009 focused update incorporated into the ACC/AHA 2005 guidelines for the diagnosis and management of heart failure in adults: A report of the American College of Cardiology Foundation/American Heart Association Task Force on Practice Guidelines developed in collaboration with the International Society for Heart and Lung Transplantationâ. J Am Coll Cardiol. vol. 53. 2009. pp. e1-e90. was a new addition to this set of guidelines.)
McMurray, JJ, Adamopoulos, S, Anker, SD. âESC guidelines for the diagnosis and treatment of acute and chronic heart failure 2012: The task force for the diagnosis and treatment of acute and chronic heart failure 2012 of the European Society of Cardiology. Developed in collaboration with the Heart Failure Association of the ESCâ. Eur Heart J. 2012. (The ESC had an independent set of guidelines for AHF in 2005, which were incorporated into, and updated in, the 2008 and 2012 documents.
It should be noted that there is very limited clinical trial evidence upon which these guidelines are based. However, there are some central articles that inform current practice and perspectives, a brief selection of which follows with annotations:
You May Like: What Kinds Of Heart Attacks Are There
