Quality Of Life And Depression Assessment
Quality of life and depression were assessed at baseline and at 30 days using the Kansas City Cardiomyopathy Questionnaire and the Depression Scale Health Questionnaire . The KCCQ is a validated, 23-item self-administered questionnaire for the evaluation of multiple aspects of HF patients health status with health domains that include physical functioning, symptom frequency and severity, social function, self-efficacy, social interference and overall quality of life . The KCCQ scales are summarized into a single summary score ranging from 0100, with higher scores reflecting better perceived health status. The PHQ-9 is a clinically validated self-administered 9-item questionnaire for depression . Depression symptoms are stratified and scored as minimal , mild , or moderate-to-severe with a score 10 considered clinically significant for depressive symptoms.
Factor That Are Associated With Diuretic Resistance
Multiple factors can explain non-responsiveness to diuretics, including inadequate doses, lack of adherence, advanced age, high sodium intake, impaired secretion into the tubule lumen, chronic kidney disease , gut edema, use of non-steroidal anti-inflammatory agents, hypoproteinemia, hypotension, nephrotic syndrome, reduced renal blood flow, and neurohormonal activation .
Tolerance at the receptor- or post-receptor points may be associated with diuretic tolerance or resistance . In the circulation, loop diuretics are bound to various proteins and secreted into the tubules by the organic anion transporters located at the basolateral membrane and multidrug resistant protein-4 located at the apical membrane. As diuretics compete with chloride for binding to NKCC2, increased salt absorption in the proximal tubules limits the diuretic-sensitive transport .
In patients with HF, RAAS activation results in sodium retention. These patients may manifet with renal dysfunction assciated with additional activation of neurohormones. As HF progresses, persistent activation of these neurohormonal systems enhances sodium retention and contributes to the development of diuretic resistance . Worsening renal function in HF reduces the usefulness of loop diuretics by reducing their secretion into the renal tubules, a process mediated by increased organic ions competing for organic ion transporter binding .
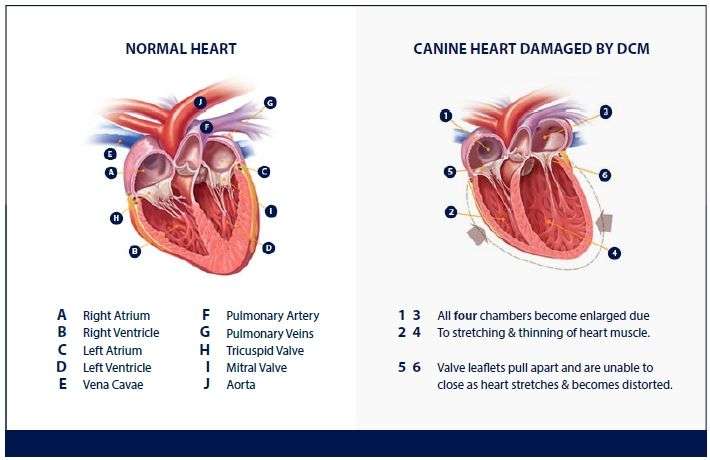
Congestive Heart Failure In Cats And Causes
Congestive heart failure in cats is an abnormality in the shape of the heart or how it functions. The abnormalities affect how much blood the heart pumps blood through a cat’s body. In cats with congestive heart failure, the heart is not able to pump enough blood, causing fluid retention in the lungs, called “pulmonary edema”.
Congestive heart failure has many causes. Some cats are born with the condition, while others may have hypertrophic cardiomyopathy or a disease that damages the lining of the heart . Heartworms, anemia, hyperthyroidism and arrhythmia can also lead to congestive heart failure.
Read Also: How Much Does Open Heart Surgery Cost
When Is A Prescription Drug Error Considered Malpractice
While some prescription drug errors are clear-cut cases of medical malpractice, such as administering the wrong medication or the wrong dose of a medication, prescribing a drug that the patient has previously reported as an allergen or mislabeling a medication, some other drug-related errors are less concrete.
However, prescribing a drug that would interact negatively with other medications, such as prescribing drugs that would interact poorly with Lasix, could also be considered medical malpractice, especially if it resulted in fatal heart and/or lung failure.
Anyone involved in prescribing or administering the medication could be held liable, including physicians, nurses, pharmacists, hospitals and potentially, the pharmaceutical manufacturer.
An experienced personal injury attorney can help determine who would be at fault.
If your loved ones doctor failed to check prescription medications, a move that resulted in heart or lung failure, you may likely have a medical malpractice suit against the physician, hospital or other parties.
Because of prescription drug interactions and other factors, knowing what drugs a patient is taking is a vital part of patient care, and failure to do so is a serious misstep that goes against the doctors oath to first do no harm.
Our team can help in handling the complexities of medical malpractice lawsuits and will address your case with compassion as well as determination.
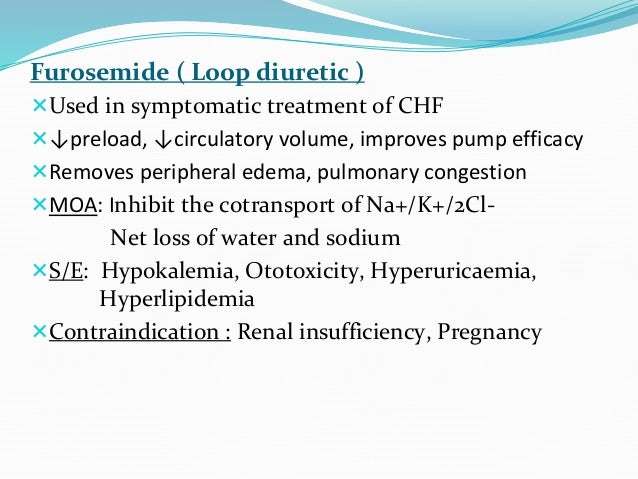
Management Of Recurrent Acute Signs
If decompensated heart failure returns, the patient should be admitted and diuretics given intravenously to regain control. A higher dose of furosemide may be needed and is often achieved by increasing the frequency of administration to 3 times daily or more. If the dose of furosemide starts to exceed 3 to 4 mg/kg q8h, furosemide resistance may be present. At that point, options include adding another diuretic, such as a hydrochlorothiazide, to achieve sequential nephron blockade.
Alternatively, the more potent loop diuretic torsemide can be prescribed. The starting dose is generally obtained by taking the total daily furosemide dose and dividing it by 10 that total daily dose of torsemide is divided to be given PO twice daily. For example, if a dog is receiving a total daily dose of 100 mg furosemide, the dose of torsemide would be 5 mg PO q12h.15
After switching diuretics, renal parameters and electrolytes should be checked in 5 to 7 days.
You May Like: How Long Does A Heart Attack Take
Left Ventricular Assist Devices
Left ventricular assist devices are mechanical pumps that can help if your left ventricle isn’t working properly and medication alone isn’t helping.
They may be used as a permanent treatment if you can’t have a heart transplant, or as a temporary measure while you wait for a transplant.
In addition to the pump, LVADs also include an external battery. A wire connecting this to the pump will need to be placed under your skin during the operation.
Read more about LVADs on the British Heart Foundation website.
Heart Failure: Effects Of Hyperaldosteronism
In animals with heart failure, chronic exposure to high concentrations of aldosterone:
- Results in excessive sodium retention, with expansion of extracellular volume
- Favors potassium and magnesium wasting
- Inhibits myocardial norepinephrine reuptake
- Contributes to endothelial dysfunction and vascular inflammation.
High concentrations of aldosterone are also independently associated with renal, vascular, and cardiac remodeling and heart failure.
An earlier study found that spironolactone had no effect on urinary sodium and water excretion in normal dogs when it was administered at dosages of 1, 2, 4, and 8 mg/kg PO Q 24 H for 8 days.6 Urinary potassium excretion, however, did decrease significantly at dosages of 1 and 2 mg/kg. These resultswhen compared to the results of the study by Guyonnet and colleaguesmay be explained by the lack of hyperaldosteronism and administration of spironolactone to fasted dogs. While differences in timing of blood sampling for one of spironolactones active metabolites does not allow for direct comparison between studies, blood canrenone concentrations were apparently higher in dogs that received spironolactone with food.
Also Check: How To Calculate Your Target Heart Rate Zone
How Is Chf Diagnosed
After reporting your symptoms to your doctor, they may refer you to a heart specialist, or cardiologist.
The cardiologist will perform a physical exam, which will involve listening to your heart with a stethoscope to detect abnormal heart rhythms.
To confirm an initial diagnosis, a cardiologist might order certain diagnostic tests to examine your hearts valves, blood vessels, and chambers.
There are a variety of tests used to diagnose heart conditions. Because these tests measure different things, your doctor may recommend a few to get a full picture of your current condition.
Diuretic Response And Resistance In Heart Failure
In achieving euvolaemia, the degree of volume overload and diuretic response will determine the success of therapy. The capacity of inducing natriuresis or diuresis following diuretic administration is defined as diuretic response. Diuretic resistance is defined as an impaired sensitivity to diuretics resulting in reduced natriuresis and diuresis limiting the possibility to achieve euvolaemia. Diuretic response should always be interpreted in light of the dose and type of the diuretic agent administered and the degree of volume overload, body composition and kidney function. As loop diuretics form the mainstay of diuretic therapy in heart failure, the terms diuretic resistance and loop diuretic resistance are often used interchangeably., – To assess the response to an initiated diuretic regimen, physicians need an indicator of the diuretic response. Currently, net fluid output and changes in body weight are frequently used. While assessment of weight might appear to be a simple measurement, it is technically challenging and fluctuations in weight might not represent changes in volume redistribution. Furthermore, there is a poor correlation between weight loss and fluid output.
Also Check: What Is The Maximum Heart Rate
What Are The Symptoms
One of the most common symptoms of congestive heart failure in dogs is a persistent cough accompanied by a difficult time breathing.
This is due to an accumulation of fluid in the lungs and the irritation produced by the enlarged heart pushing against the trachea.
Dogs that have CHF will tire easily and pant excessively while playing and exercising. Taking walks will become more difficult.
They may also show a persistent lack of appetite with a swollen belly. You should check your dogs gums for signs of paleness or bluishness.
If you see any of these signs consult your veterinarian immediately.
What To Expect At Home
When you have heart failure, your heart does not pump out enough blood. This causes fluids to build up in your body. If you drink too many fluids, you may get symptoms such as swelling, weight gain, and shortness of breath. Limiting how much you drink and how much salt you take in can help prevent these symptoms.
Your family members can help you take care of yourself. They can keep an eye on how much you drink. They can make sure you are taking your medicines the right way. And they can learn to recognize your symptoms early.
Your health care provider may ask you to lower the amount of fluids you drink:
- When your heart failure is not very bad, you may not have to limit your fluids too much.
- As your heart failure gets worse, you may need to limit fluids to 6 to 9 cups a day.
Recommended Reading: How To Fight Heart Disease
What Other Drugs Will Affect Furosemide
Sometimes it is not safe to use certain medications at the same time. Some drugs can affect your blood levels of other drugs you take, which may increase side effects or make the medications less effective.
If you also take sucralfate, take your furosemide dose 2 hours before or 2 hours after you take sucralfate.
Tell your doctor about all your other medicines, especially:
Before Taking This Medicine
You should not use Lasix if you are allergic to furosemide, or:
-
if you are unable to urinate.
To make sure Lasix is safe for you, tell your doctor if you have:
-
kidney disease
-
diabetes or
-
sulfa drug allergy.
Tell your doctor if you have an MRI or any type of scan using a radioactive dye that is injected into your veins. Both contrast dyes and furosemide can harm your kidneys.
It is not known whether Lasix will harm an unborn baby. Tell your doctor if you are pregnant or plan to become pregnant while using this medicine.
Furosemide can pass into breast milk and may harm a nursing baby. This medicine may also slow breast milk production. Tell your doctor if you are breast-feeding a baby.
You May Like: Can Blood Test Detect Heart Attack
Congestive Heart Failure In Dogs
Simon Swift
MA, VetMB, CertSAC, DECVIM-CA , MRCVS
After qualifying from Cambridge University, Dr. Swift spent 2 years in mixed practice before moving to a specialist small animal practice in the Northwest of England. He developed an interest in cardiology, taking the RCVS cardiology certificate in 1990. He became a partner in a large emergency and referral hospital building up the cardiology referral service until he left in 2005 to follow an alternative residency program at Liverpool University. Since becoming a European Diplomate in cardiology, he worked in a private referral hospital before moving to Florida to join the College of Veterinary Medicine as Clinical Associate Professor. He is service chief for cardiology and has recently been appointed medical director. He has been involved in breeding programs and the treatment of degenerative valvular disease especially in the cavalier King Charles spaniel having been adviser to the UK CKCS club for 20 years and more recently has helped develop advanced interventional techniques at the University of Florida.
STAGE
A: A dog at risk of heart disease
B1: Signs of heart disease . The dog is asymptomatic.
B2: Signs of heart disease . The dog is asymptomatic.
C: Congestive heart failure is present or has been present and the dog is receiving treatment.
D: Congestive heart failure is present and refractory to standard therapies. The patient requires hospitalization.
Should I Avoid Certain Food Or Medications While On A Diuretic
Diuretics are sometimes prescribed in combination with an ACE inhibitor, digoxin, and a beta-blocker or angiotensin receptor blocker Entresto. If you have more side effects after taking your medicines together, call your doctor. You may need to change the times you are taking each drug.
Potassium-sparing diuretics increase the effects of digoxin and lithium. They may increase your body’s potassium level if taken with ACE inhibitors.
Before a diuretic is prescribed, tell your doctor if you are taking other drugs for high blood pressure, digoxin, Indocin, lithium, probenecid, or corticosteroids .
Before youâre prescribed a diuretic, tell your doctor if you have diabetes, kidney disease, liver disease, or gout.
Follow your doctor’s advice about your diet. This may include:
- A low-salt diet
- Taking a potassium supplement
- Adding high-potassium foods in your diet.
Note: Some diuretics cause your body to lose potassium. If youâre taking a “potassium-sparing” diuretic, your doctor may want you to avoid potassium-rich foods, salt substitutes, low-salt milk, and other sources of potassium. If you are not sure what type of diuretic you are taking, ask your doctor.
Recommended Reading: What Causes Shortness Of Breath After Heart Attack
Things You Should Do To Manage Chf Symptoms
There are many dogs that live long lives with CHF and another congenital heart disease.
Successful living with heart disease is much like it is with humans, it takes care, medications, quality nutrition, and exercise.
Below is a list of 10 things you should do to manage symptoms of congestive heart failure in dogs to ensure your pet lives a quality life.
1. Coughing
If coughing becomes severe, contact your veterinarian. If already diagnosed with CHF and on furosemide, your vet may recommend an additional dose to alleviate any extra accumulation of fluids.
Watch your dog carefully, time coughing, and take notes for the next visit.
2. Difficulty Breathing
With CHF, difficulty breathing indicates fluid build-up in the lungs. Your vet may prescribe additional diuretics like furosemide.
If the difficulty breathing worsens call your veterinarian immediately.
3. Difficulty Sleeping
Dogs may try to sleep on their chest instead of their sides. You may observe your dog trying to sleep quietly sitting up.
This is due to the fluid build-up in the lungs when your dog lies on its side making it uncomfortable. Its a sign to get a check-up.
4. Exercise
Dogs with CHF should be allowed the amount of exercise they want to enjoy life. If they become tired or weak, it’s best to take a break.
Pushing your dog beyond its limits can cause irregular heartbeats .
5. Expensive Medications
There may also be a less expensive alternative treatment that your vet may be aware of. Call your vet first.
Biochemical And Metabolic Effects Of Diuretics
Loop and thiazide diuretics may lead to deficiency of the main electrolytes, particularly potassium and sodium. Hypokalaemia and hyponatraemia to a lesser degree may secondarily cause other metabolic effects. The degree of potassium wastage and hypokalaemia is directly related to the dose of diuretic. Hypokalaemia may precipitate potentially hazardous ventricular ectopic activity and increase the risk of primary cardiac arrest, even in patients who are not on concomitant digitalis therapy and do not have myocardial irritability. Even mild hypokalaemia caused by these diuretics may result in leg cramps, polyuria, and muscle weakness. In some patients, concomitant diuretic induced magnesium deficiency prevents the restoration of intracellular potassium deficits. Hence, it is important that magnesium levels in patients with heart failure who are treated with diuretics are regularly checked and magnesium corrected if necessary. Magnesium deficiency may also be responsible for some of the arrhythmias ascribed to hypokalaemia.
An increase in the incidence of impotence has been noted in men taking thiazide diuretics. A significant increase in renal cell carcinoma among diuretic users was found in a search of nine case-control and three cohort studies. Although the risk ratio was 1.55, the absolute incidence of renal cell carcinoma was only 0.065%, which was not statistically significant. The overall positive effects of diuretic use therefore far outweigh their hazards.
Recommended Reading: What Does A Heart Attack Look Like
Chronic Treatment Of Congestive Heart Failure In Dogs
Chronic treatment of patients with CHF shifts from trying to control pulmonary edema to trying to negate deleterious effects of neurohormonal stimulation. The aim of chronic CHF treatment is to increase longevity of the patient, as well as improve quality of life. As a result, treatment for chronic CHF generally involves the use of 4 medications: furosemide, pimobendan, an angiotensin-converting enzyme inhibitor, and spironolactone. These drugs are usually continued indefinitely. Other drugs may also be required.
Diuretic Resistance Is A Major Difficulty In The Treatment Of Hf
The effects of loop diuretics on systemic and renal hemodynamics are driven by multiple factors, including the dose, route of administration, concomitant diseases, and medications and chronicity of their use . Furosemide is a potent prototypic loop diuretic that exerts its effect by binding to the translocation pocket at the extracellular surface of sodium-potassium-chloride symporters . It blocks ion transport directly by inhibiting NKCCs at the apical surface of the thick ascending loop of Henle . The half-life of loop diuretics is generally shorter than typical dosing intervals of twice daily. Additionally, as they inhibit solute transport at only a single segment out of the numerous sodium-reabsorbing nephron sections, their impacts on extracellular fluid volume are multifaceted. Loop diuretics cause renal vasodilation through direct vascular dilation of the afferent arterioles and inhibition of the tubuloglomerular feedback .
Don’t Miss: Do Heart Palpitations Go Away
