What Are Cardiovascular Diseases
Cardiovascular diseases are a group of disorders of the heart and blood vessels. They include:
- coronary heart disease a disease of the blood vessels supplying the heart muscle
- cerebrovascular disease a disease of the blood vessels supplying the brain
- peripheral arterial disease a disease of blood vessels supplying the arms and legs
- rheumatic heart disease damage to the heart muscle and heart valves from rheumatic fever, caused by streptococcal bacteria
- congenital heart disease birth defects that affect the normal development and functioning of the heart caused by malformations of the heart structure from birth and
- deep vein thrombosis and pulmonary embolism blood clots in the leg veins, which can dislodge and move to the heart and lungs.
Heart attacks and strokes are usually acute events and are mainly caused by a blockage that prevents blood from flowing to the heart or brain. The most common reason for this is a build-up of fatty deposits on the inner walls of the blood vessels thatsupply the heart or brain. Strokes can be caused by bleeding from a blood vessel in the brain or from blood clots.
Systolic And Diastolic Failure
Systolic and diastolic heart failure each result in a decrease in stroke volume. This leads to activation of peripheral and central baroreflexes and chemoreflexes that are capable of eliciting marked increases in sympathetic nerve traffic.
Although there are commonalities in the neurohormonal responses to decreased stroke volume, the neurohormone-mediated events that follow have been most clearly elucidated for individuals with systolic heart failure. The ensuing elevation in plasma norepinephrine directly correlates with the degree of cardiac dysfunction and has significant prognostic implications. Norepinephrine, while directly toxic to cardiac myocytes, is also responsible for a variety of signal-transduction abnormalities, such as downregulation of beta1-adrenergic receptors, uncoupling of beta2-adrenergic receptors, and increased activity of inhibitory G-protein. Changes in beta1-adrenergic receptors result in overexpression and promote myocardial hypertrophy.
The Percentage Of Heart Failure
- The percentage of heart failure-related deaths that occurred in a hospital decreased 30%, from 42.6% in 2000 to 30.0% in 2014 .
- The percentage of heart failure-related deaths that occurred at a descendants home increased 51%, from 18.3% in 2000 to 27.6% in 2014.
- The percentage of heart failure-related deaths that occurred in nursing homes or long-term care facilities decreased 11%, from 30.1% in 2000 to 26.7% in 2014.
- The percentage of heart failure-related deaths that occurred in other places increased 74%, from 9.0% in 2000 to 15.7% in 2014.
1Increases in the percentage of deaths that occurred at home and other places were statistically significant .2Percentages of heart failure-related deaths that occurred in a hospital, nursing home, and long-term care facilities declined significantly .NOTES: Heart failure-related deaths were identified as those with heart failure reported anywhere on the death certificate . Access data table for Figure 4pdf icon.SOURCE: CDC/NCHS, National Vital Statistics System mortality data, 20002014.
You May Like: Pneumonia And Congestive Heart Failure
Prevalence And Underlying Cause Estimation
The overall prevalence of HF was estimated using DisMod-MR 2.1, a Bayesian meta-regression tool developed for GBD analyses. For inpatient hospital data, we corrected for readmission, primary to any diagnosis, and inpatient to outpatient utilization ratios using adjustment factors derived from individual-level claims data. We included covariates in DisMod-MR 2.1 to adjust US claims data and ICPC-coded data from Norway. The underlying causes of HF were selected based on a review of the literature and expert opinion. To estimate the proportion of HF cases attributable to each cause, the proportion of HF cases attributable to each of the highlevel parent cause groupings was firstly assessed. Then, we estimated the proportion of HF cases attributable to the detailed causes within each of these groupings. Finally, we applied a correction factor to adjust these proportions. Notably, the prevalence of HF attributable to Chagas, degenerative mitral valve disease, and calcific aortic valve disease were estimated separately as part of their respective modelling strategy. Thus, the prevalence of HF due to all other causes was adjusted by subtracting the prevalence of HF due to these causes from the overall HF estimates. More information about the estimation process has been published elsewhere.
How Can I Improve My Quality Of Life With Heart Failure
There are several things you can do to improve your quality of life if you have heart failure. Among them:
- Eat a healthy diet. Limit your consumption of sodium to less than 1,500 milligrams each day. Eat foods high in fiber. Limit foods high in trans fat, cholesterol, and sugar. Reduce total daily intake of calories to lose weight if necessary.
- Exercise regularly. A regular cardiovascular exercise program, prescribed by your doctor, will help improve your strength and make you feel better. It may also decrease heart failure progression.
- Don’t overdo it. Plan your activities and include rest periods during the day. Certain activities, such as pushing or pulling heavy objects and shoveling may worsen heart failure and its symptoms.
- Prevent respiratory infections. Ask your doctor about flu and pneumonia vaccines.
- Take your medications as prescribed. Do not stop taking them without first contacting your doctor.
- Get emotional or psychological support if needed. Heart failure can be difficult for your whole family. If you have questions, ask your doctor or nurse. If you need emotional support, social workers, psychologists, clergy, and heart failure support groups are a phone call away. Ask your doctor or nurse to point you in the right direction.
Also Check: What Is Heart Stent Surgery
Were The Changes In The Rate Of Congestive Heart Failure Hospitalization The Same For Males And Females Under And Over Age 65
- The CHF hospitalization rate for males under age 65 increased by 21% from 2000 to 2010, but rates did not change significantly for males aged 6574, 7584, or 85 and over .
- The CHF hospitalization rate for females under age 65 did not change significantly from 2000 to 2010 however, rates for females decreased by 44% for those aged 6574, 27% for those aged 7584, and 17% for those aged 85 and over.
Figure 3. Percent change in congestive heart failure hospitalization rates, by sex and age: United States, 2000 to 2010
Change from 2000 to 2010 was statistically significant at the 0.05 level using a weighted least squares regression method to measure linear trends over time. Data for every year were included in this test. SOURCE: CDC/NCHS, National Hospital Discharge Survey, 20002010.
Congestive Heart Failure: Insights From Epidemiology Implications For Treatment
- Barry M. MassieCorrespondenceAddress reprint requests to Dr. B. M. Massie, Cardiology Section , Department of Veterans Affairs Medical Center, 4150 Clement Street, San Francisco, CA 94121Affiliations
Mayo Clinic ProceedingsAm J Cardiol.
- National Center for Health Statistics
Vital Health Stat .
N Y State J Med.
You May Like: How Old Do You Have To Be To Have A Heart Attack
Stages Of Heart Failure
In 2001, the American Heart Association and American College of Cardiology described the “Stages of Heart Failure.” These stages, which were updated in 2005, will help you understand that heart failure is often a progressive condition and can worsen over time. They will also help you understand why a new medication was added to your treatment plan and may help you understand why lifestyle changes and other treatments are needed.
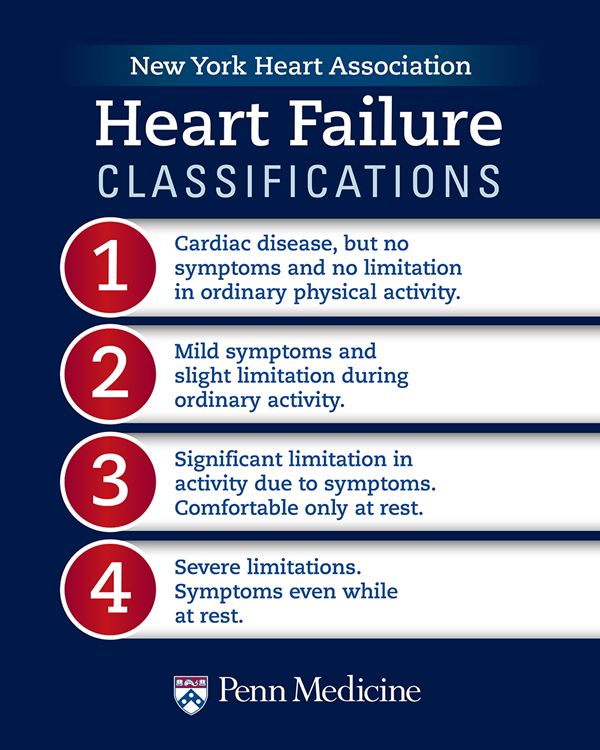
The stages classified by the AHA and ACC are different than the New York Heart Association clinical classifications of heart failure that rank patients as class I-II-III-IV, according to the degree of symptoms or functional limits. Ask your doctor what stage of heart failure you are in.
Check the table below to see if your therapy matches what the AHA and ACC recommend. Note that you cannot go backward in stage, only forward.
The table below outlines a basic plan of care that may or may not apply to you, based on the cause of your heart failure and your special needs. Ask your doctor to explain therapies that are listed if you do not understand why you are or are not receiving them.
The New York Heart Association clinical classifications of heart failure rank people as class I-II-III-IV, according to the degree of symptoms or functional limits. You can ask your doctor if you want to know what stage of heart failure youâre in.
Did Trends In Congestive Heart Failure Hospitalization Rates Differ For Males And Females From 2000 To 2010
- In 2000, the rate of CHF hospitalization among females was one-third higher than the rate among males , but male and female rates converged over time, and by 2010 the male and female rates were similar .
- In 2000, approximately 42% of CHF hospitalizations were for males, compared with 58% for females, but by 2010 there were equal proportions of males and females .
Figure 2. Congestive heart failure hospitalization rates for males and females: United States, 20002010
Change was statistically significant at the 0.05 level using a weighted least squares regression method, including data from all years, to measure linear trends over time from 2000 to 2010. SOURCE: CDC/NCHS, National Hospital Discharge Survey, 20002010.
You May Like: Heart Attack Signs Men
Heart Failure Treatment Is A Team Effort
Heart failure management is a team effort, and you are the key player on the team. Your heart doctor will prescribe your medications and manage other medical problems. Other team members — including nurses, dietitians, pharmacists, exercise specialists, and social workers — will help you achieve success. But it is up to YOU to take your medications, make dietary changes, live a healthy lifestyle, keep your follow-up appointments, and be an active member of the team.
If you notice anything unusual, don’t wait until your next appointment to discuss it with your doctor. Call them right away if you have:
- Unexplained weight gain
- Swelling in your ankles, feet, legs, or belly that gets worse
- Shortness of breath that gets worse or happens more often, especially if you wake up feeling that way
- Bloating with a loss of appetite or nausea
- Extreme fatigue or more trouble finishing your daily activities
- A lung infection or a cough that gets worse
- Fast heart rate
- New irregular heartbeat
Heart Failure With Preserved Ejection Fraction
In diastolic heart failure , the same pathophysiologic processes occur that lead to decreased cardiac output in systolic heart failure, but they do so in response to a different set of hemodynamic and circulatory environmental factors that depress cardiac output.
In HFpEF, altered relaxation and increased stiffness of the ventricle occur in response to an increase in ventricular afterload . The impaired relaxation of the ventricle then leads to impaired diastolic filling of the left ventricle .
Morris et al found that right venticular subendocardial systolic dysfunction and diastolic dysfunction, as detected by echocardiographic strain rate imaging, are common in patients with HFpEF. This dysfunction is potentially associated with the same fibrotic processes that affect the subendocardial layer of the LV and, to a lesser extent, with RV pressure overload. It may play a role in the symptomatology of patients with HFpEF.
Don’t Miss: How To Find Max Heart Rate
How Is Chf Diagnosed
After reporting your symptoms to your doctor, they may refer you to a heart specialist, or cardiologist.
The cardiologist will perform a physical exam, which will involve listening to your heart with a stethoscope to detect abnormal heart rhythms.
To confirm an initial diagnosis, a cardiologist might order certain diagnostic tests to examine your hearts valves, blood vessels, and chambers.
There are a variety of tests used to diagnose heart conditions. Because these tests measure different things, your doctor may recommend a few to get a full picture of your current condition.
Heart Disease: Facts Statistics And You
Heart disease refers to a variety of conditions that affect the heart from infections to genetic defects and blood-vessel diseases.
Most heart disease can be prevented with healthy lifestyle choices, yet its still the number one health threat in the world.
See the numbers behind this condition, learn the risk factors, and find out how to prevent heart disease.
Heart disease is responsible for most deaths worldwide for both men and women of all races.
As of 2018,
, approximately every 40 seconds an American will have a heart attack. Every year, 805,000 Americans have a heart attack, 605,000 of them for the first time.
About 12 percent of people who have a heart attack will die from it.
Coronary artery disease, a blockage of the arteries that supply blood to the heart, is the most common type of heart disease. Coronary heart disease affects about 18.2 million Americans age 20 and older, and it killed nearly 366,000 in 2017.
Heart disease is the number one cause of death for most racial and ethnic groups. In 2015, it was responsible for of deaths in white people and 23.5 percent in Black people.
In 2017, death rates from heart disease in Black men were 202.8 deaths per 100,000 people . That compared to 274.5 deaths per 100,000 for white males. The death rates for Black women were 165.5 per 100,000, and for white women they were 231.4 per 100,000.
Follow these six simple tips to keep your ticker ticking:
You May Like: How Blood Travels Through The Heart
How Can The Burden Of Cardiovascular Diseases Be Reduced
The key to cardiovascular disease reduction lies in the inclusion of cardiovascular disease management interventions in universal health coverage packages, although in a high number of countries health systems require significant investment and reorientationto effectively manage CVDs.
Evidence from 18 countries has shown that hypertension programmes can be implemented efficiently and cost-effectively at the primary care level which will ultimately result in reduced coronary heart disease and stroke. Patients with cardiovascular diseaseshould have access to appropriate technology and medication. Basic medicines that should be available include:
What Is Heart Failure
Heart failure means that your heart can’t pump enough oxygen-rich blood to meet your body’s needs. Heart failure doesn’t mean that your heart has stopped or is about to stop beating. But without enough blood flow, your organs may not work well, which can cause serious problems.
Heart failure can affect one or both sides of your heart:
- With right-sided heart failure, your heart is too weak to pump enough blood to your lungs to get oxygen.
- With left-sided heart failure, your heart can’t pump enough oxygen-rich blood out to your body. This happens when the left side of your heart becomes either:
- Too weak to pump enough blood.
- Too thick or stiff to relax and fill with enough blood.
Left-sided heart failure is more common than right-sided heart failure.
Recommended Reading: Sternum Pain Years After Open Heart Surgery
How Is Congestive Heart Failure Diagnosed
Patients will typically have an intake visit with a heart specialist and nurse or physicians assistant. During this visit, the doctor will review the patients prior records and his or her current health status. This allows the doctor to establish a picture of where the patient is along the spectrum, and make a plan for prognosis and treatment.
The process often takes more than one meeting and involves both the patients local cardiologist or referring physician.
Did The Rate Of Hospitalization For Chf Change From 2000 To 2010
- The overall rate of CHF hospitalization per 10,000 population did not change significantly from 2000 to 2010 , but the trends were different for those under age 65 compared with those aged 65 and over .
- For those under age 65, the rate of CHF hospitalization was low in both 2000 and 2010 compared with older patients, but it increased by 15% over this time periodfrom 9.4 to 10.8 per 10,000 population.
- For those aged 65 and over, the rate of CHF hospitalization was much higher than the rate for those under age 65 but the rate decreased by 19% from 2000 to 2010from 218.6 to 177.7 per 10,000 population.
- The rate of CHF hospitalization per 10,000 population increased with advancing age in both 2000 and 2010.
Table. Rates for congestive heart failure hospitalization, by age in years: United States, 2000 and 2010
| 2000 | |
|---|---|
| 475.9 | 430.7 |
Change from 2000 to 2010 was statistically significant at the 0.05 level using a weighted least squares regression method, including all years of data, to measure linear trends over time. SOURCE: CDC/NCHS, National Hospital Discharge Survey, 20002010.
Recommended Reading: After Open Heart Surgery Recovery
What Are The Types Of Heart Failure
Systolic dysfunction happens when the heart muscle doesn’t contract with enough force, so there is less oxygen-rich blood pumped throughout the body.
Diastolic dysfunction happens when the heart contracts normally, but the ventricles donât relax properly or are stiff, and less blood enters the heart during normal filling.
A calculation done during an echocardiogram, called the ejection fraction , is used to measure how well your heart pumps with each beat to help determine if systolic or diastolic dysfunction is present. Your doctor can discuss which condition you have.
Why Are Cardiovascular Diseases A Development Issue In Low
At least three-quarters of the world’s deaths from CVDs occur in low- and middle-income countries. People living in low- and middle-income countries often do not have the benefit of primary health care programmes for early detection and treatment of peoplewith risk factors for CVDs. People in low- and middle-income countries who suffer from CVDs and other noncommunicable diseases have less access to effective and equitable health care services which respond to their needs. As a result, for many peoplein these countries detection is often late in the course of the disease and people die at a younger age from CVDs and other noncommunicable diseases, often in their most productive years.
The poorest people in low- and middle-income countries are most affected. At the household level, evidence is emerging that CVDs and other noncommunicable diseases contribute to poverty due to catastrophic health spending and high out-of-pocket expenditure.At the macro-economic level, CVDs place a heavy burden on the economies of low- and middle-income countries.
Read Also: Congestive Heart Failure Prevention
