What Medications Are Commonly Given To Patients With Heart Failure
The chart below lists commonly prescribed medications for heart failure. Theyre organized by medication class. A medication class is a group of drugs that are similar in some way. For example, all the drugs in one class might have the same active ingredient or treat the same problem.
Your healthcare provider will explain to you which drugs you need and why you need them. The regimen thats right for you depends on what type of heart failure you have.
| Medication class |
|---|
Heart Failure With Preserved Ejection Fraction
Compared to those with a reduced ejection fraction, patients with heart failure with preserved ejection fraction are older, more likely to be female and to have hypertension, atrial fibrillation, diabetes or obesity. The mechanism probably relates to a combination of pathophysiological processes including increased myocardial stiffness, abnormal myocardial relaxation and increased arterial stiffness.
No drug has been shown to improve survival,35 however recent data suggest that in a subset of patients with heart failure and preserved ejection fraction, aldosterone antagonists may improve clinical outcomes.36 Sacubitril with valsartan was found to be beneficial in a phase II study.37 The combination is therefore currently under evaluation for heart failure with preserved ejection fraction.
Diuretics should be used judiciously and over-diuresis avoided. Treatment should focus on aggressive control of concurrent conditions particularly hypertension. Atrial fibrillation should be managed according to guidelines, using a rate control strategy and anticoagulation initially, with a trial of rhythm control for persistent symptoms. Myocardial ischaemia, obesity and anaemia should be addressed. Exercise training can improve quality of life.
Classification And Staging Of Heart Failure
Classifying heart failure on the basis of severity and clinical manifestations helps clarify what kinds of interventions may be necessary and what the prognosis may be. The New York Heart Association Functional Classification classifies patients with cardiac disease into one of four classes, based on symptoms and their degree of comfort at different levels of physical activity.
Read Also: Is Angioplasty Considered Heart Surgery
What Natural Interventions May Be Beneficial For Heart Failure
- Coenzyme Q10. Coenzyme Q10 is essential for energy production in the mitochondria and is concentrated in heart muscle. CoQ10 deficiency is associated with heart failure. Several clinical studies have shown benefits from CoQ10 supplementation in heart failure, including lower risk of adverse cardiac events or death.
- Hawthorn. Extracts from hawthorn contain many beneficial phytochemicals, including oligomeric procyanidins. Hawthorn has been shown to improve left ventricle ejection fraction, cardiac efficiency, and blood pressure in patients with heart failure.
- Pyrroloquinoline quinone . PQQ, like CoQ10, is involved in generating energy in the mitochondria. Preclinical studies suggest PQQ may benefit the heart muscle.
- Fish oil. Omega-3 fatty acids are well known for their positive impact on heart health. Clinical studies indicate supplementation with fish oil may improve certain parameters in patients with heart failure.
- Carnitine. Carnitine is important for cardiac energy metabolism. Clinical trials have shown that carnitine supplementation improved cardiac efficiency, left ventricle ejection fraction, and 3-year survival rates in heart failure patients.
- Many other ingredients may be beneficial for patients with heart failure, including creatine, taurine, D-ribose, and more.
Coenzyme Q10 For Sams
SAMS is a condition that occurs in people who are using statins to lower their cholesterol.
People who have SAMS may have symptoms such as muscle aches, cramps, muscle weakness, and, rarely, rhabdomyolysis .
Clinical trials dealing with the use of coenzyme Q10 for SAMS have given conflicting results.
However, the largest and most recent study dealing with this topic does suggest its effective in preventing and treating SAMS.
Numerous anecdotal reports from patients also supports its use.
Theres no established dose for coenzyme Q10, although, on average, 200 mg taken twice daily with meals will give a therapeutic blood level of > 2.5 mcg/mL.
In most heart-related clinical trials, doses between 100 and 400 mg have been used.
Recommended Reading: What Is A Good Resting Heart Rate For Women
Why They Worsen Heart Failure
For people with congestive heart failure, even short-term use of NSAIDs can increase blood pressure and interfere with blood-pressure-lowering drugs. When blood pressure is high, the heart must work harder to pump blood which can contribute to weakening of the heart muscle over time.
Many over-the-counter cough and cold medications contain an NSAID and so it’s important to read labels before taking one if you’ve also recently taken a multi-symptom drug .
Angiotensin Ii Receptor Blockers
These drugs are not demonstrably superior to ACE inhibitors but are less likely to cause cough and angioedema they may be used when these adverse effects prohibit ACE inhibitor use.
In chronic HFrEF, ACE inhibitors and ARBs are likely equally effective. Usual oral target doses are valsartan 160 mg twice a day, candesartan 32 mg once a day, and losartan 50 to 100 mg once a day. Introduction, upward dose adjustment, and monitoring of ARBs and ACE inhibitors are similar. Like ACE inhibitors, ARBs can cause reversible renal dysfunction, and the dose may need to be reduced or stopped temporarily during an acute dehydrating illness.
In HFpEF, a large randomized controlled trial of candesartan is a syndrome of ventricular dysfunction . Drug treatment of heart failure involves symptom relief with Diuretics Nitrates Digoxin read more ) demonstrated reduced number of hospitalizations for recurrent HF however, hospitalization was a secondary endpoint. In another trial is a syndrome of ventricular dysfunction . Drug treatment of heart failure involves symptom relief with Diuretics Nitrates Digoxin read more ), irbesartan was not associated with any improvement in outcomes in HFpEF. Therefore, ARBs should be used in HFpEF only if they are already being used to treat hypertension, diabetic kidney disease, or microalbuminuria.
ARBs are contraindicated in pregnancy.
Recommended Reading: Congestive Heart Failure Feeling Cold
Independent Variable: Exposure To A Potentially Inappropriate Drug
For each of the potentially inappropriate drug class examined , we classified patients as user or nonuser. Among dihydropyridine CCBs, only nifedipine was considered as there is evidence of contra-indications in heart failure only for that drug. We searched for a claim for a contra-indicated drug class in the 365 days before HF diagnosis and between HF diagnosis and the event date. We selected the claim closest to the event date and then determined the exposure time period by adding 1.5 times the number of days supply to this last claim date. If the event date occurred in the exposure time period, we deemed the patient as being a user. We repeated the process for each medication class.
Diclofenac: New Contraindications And Warnings
New recommendations after a Europe-wide review of cardiovascular safety.
- From:
Article date: June 2013
An increased risk of heart attack and stroke with some non-selective non-steroidal anti-inflammatory drugs such as diclofenacis well recognised, particularly with long-term use of high doses and in patients who are already at high risk. Warnings for healthcare professionals and patients have been included in the product information and in the British National Formulary for some years.
The European Medicines Agencys Pharmacovigilance Risk Assessment Committee has recently recommended updates to the treatment advice for diclofenac in light of the findings of a Europe-wide review of the cardiovascular safety of NSAIDs. The review found further evidence that the arterial thrombotic risk with diclofenac is similar to that for the selective COX-2 inhibitors.
The new treatment advice applies to systemic formulations it does not apply to topical formulations of diclofenac.
A recently published meta-analysis of clinical trial data provides further evidence that the arterial thrombotic risk with diclofenac is similar to that of COX-2 inhibitors. This analysis found that of 1000 patients allocated to diclofenac for a year, three more had major vascular events, compared with placebo.
Also Check: What Artery Supplies Blood To The Heart
Medicines For Heart Failure
Most people with heart failure are treated with medication. Often you’ll need to take 2 or 3 different medicines.
Some of the main medicines for heart failure include:
- SGLT2 inhibitors
You may need to try a few different medicines before you find a combination that controls your symptoms but doesn’t cause unpleasant side effects.
What Are The Common Symptoms Of Cardiovascular Problems
Cardiovascular diseases refer to the group of medical disorders that impact the functioning of the heart and blood vessels. The symptoms of cardiovascular disease depend on the specific type of disease you have. Some of the most common cardiovascular problems are listed below, with descriptions of their symptoms.
Also Check: What Are The Symptoms Of Heart Failure
What Causes Congestive Heart Failure In Dogs
Heart disease, which can develop into heart failure, is commonly seen in older dogs. According to veterinary cardiologist Dr. Bonnie Lefbom, Dipl. ACVIM, incidence of heart disease varies from between 15% to 30% of older, small dogs and 5% to 15% of giant breed dogs.
Congestive heart failure, which can occur as heart disease progresses, is less common thanks to the veterinary treatments available today, but some dogs with heart disease will go on to develop heart failure. Dr. Lefbom says small breed dogs with a long-standing heart murmur are the most common patients with CHF. Large and giant breed dogs more commonly develop a weakened heart muscle.
One of the most common causes of heart failure in dogs is chronic degenerative valve disease . Just like in older people, the heart valves can start to break down and leak, causing backflow in the heart and a heart murmur, says Dr. Lefbom, who practices at the Regional Veterinary Referral Center in Springfield, Virginia. Over time, with continued backflow through the valves, the heart enlarges. When the heart gets too big, fluid backs up in the lungs.
Some breeds at higher risk for developing CVD include:
- Cocker Spaniels
Studies Have Shown That Several Classes Of Drugs Are Best To Treat Heart Failure
Heart failure patients may need multiple medications. Each one treats a different symptom or contributing factor and comes with its own instructions and rules.
You and your caregivers should work with your healthcare team to understand the medications and when, how often and in what dosage to take them.
Its important to discuss all of the drugs you take with your doctor and understand their desired effects and possible side effects. Your doctor and your pharmacist are your best sources of information. Dont hesitate to ask them questions about your medicines.
It’s critical that people with heart failure take their medications exactly as directed by their healthcare provider, to optimize the benefits. The use of these drugs has saved lives, prolonged life and improved the hearts function.
The following list gives you a quick look at many typical medications to treat heart failure at different stages. Your prescription may have a different name from the ones listed here. Brand names commonly available in the United States are shown in parentheses after the generic name for each drug.
Read Also: Drugs To Lower Heart Rate
Lower Fat And Cholesterol
Studies have shown that the rate of heart failure is lower in people who follow a DASH diet , which centers on consuming polyunsaturated fats, complex carbohydrates like brown rice, low amounts of saturated fats, and fruits and vegetables.
Saturated fat and cholesterol can lead to other cardiovascular issues like atherosclerosis, which is the buildup of plaque on the walls of the arteries. To reduce that risk, eliminate butter, shortening, and margarine, and consume limited amounts of olive, peanut, and canola oils.
To lower your fat intake, avoid fatty cuts of meat, remove the skin from poultry, and consume more fish. Replace high-fat dairy with low-fat or nonfat options, eat whole grains for their high fiber content, and limit condiments and salad dressings that are high in fat and sodium. When preparing your food, avoid frying, and choose to bake, broil, poach, boil, or steam instead.
Recommended Reading: What Heart Rate Burns Fat
Ace Inhibitors And Angiotensin Receptor Antagonists
ACE inhibitors are first-line therapy in heart failure with reduced ejection fraction and asymptomatic left-ventricular dysfunction. Their use results in a 3.8% absolute reduction in death, with reductions in myocardial infarction and hospitalisation for heart failure.13 Beneficial effects occur early and continue long term, in all age groups. ACE inhibitors reduce the maladaptive effects of chronic renin angiotensinaldosterone system activation, including sodium and water retention, vasoconstriction, and cardiac hypertrophy and fibrosis. Studies of angiotensin receptor antagonists have not shown a consistent reduction in mortality.14,15 Sartans are therefore considered as a second choice, indicated only in patients intolerant of ACE inhibitors.
Treatment should begin soon after diagnosis, at the lowest dose. Up-titration is recommended if the blood pressure is 90 mmHg systolic or above, and is limited by symptoms rather than the measured blood pressure. If symptomatic hypotension occurs, other vasodilators should be reduced or stopped first and, provided the patient is not congested, diuretics should be reduced or ceased before reducing the ACE inhibitor dose.
Don’t Miss: Fat Burning Heart Rate Calculator
Treatments Recommended In Selected Symptomatic Patients With Hfref
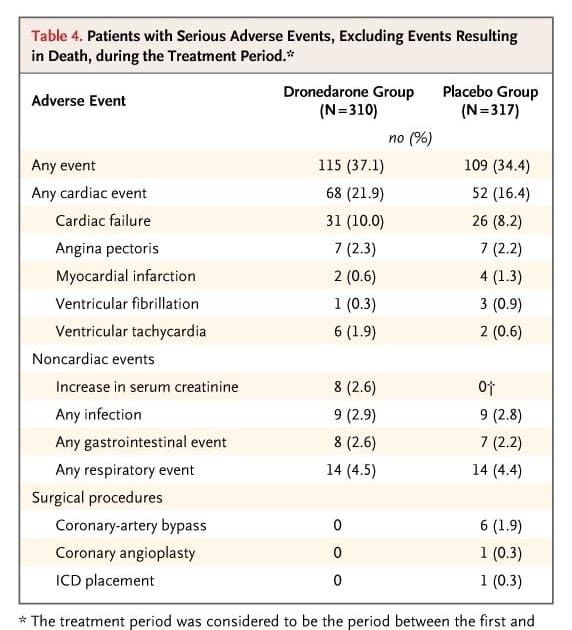
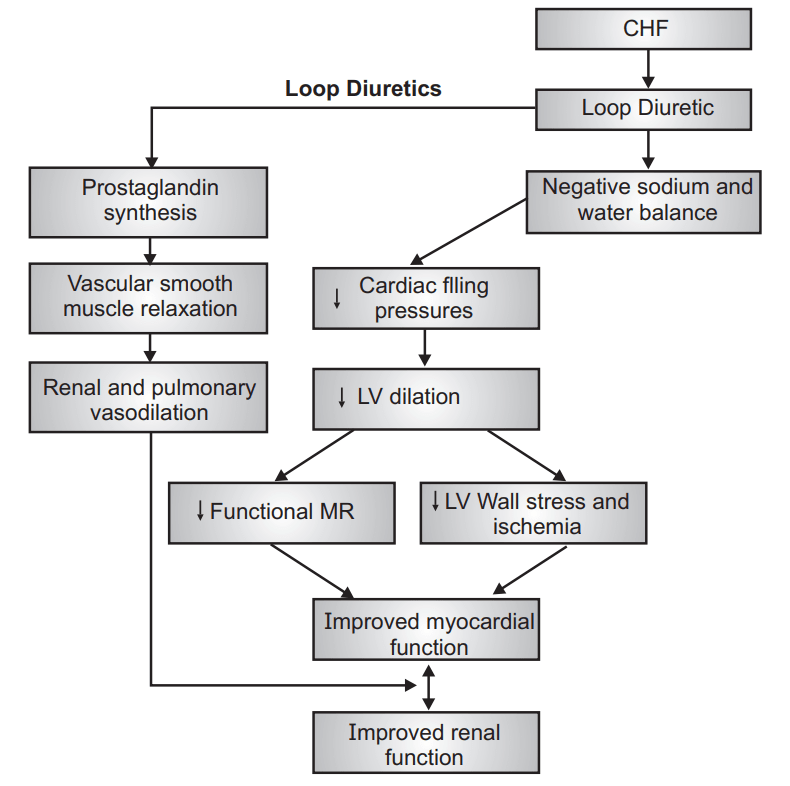
Diuretics
Diuretics are recommended to reduce the signs and symptoms of congestion in patients with HFrEF, but their effects on mortality and morbidity have not been studied in randomised controlled trials . Loop diuretics produce a more intense and shorter diuresis than thiazides, although they act synergistically and the combination may be used to treat resistant oedema. However, adverse effects are more likely and these combinations should only be used with care. The aim of diuretic therapy is to achieve and maintain euvolaemia with the lowest achievable dose. The dose of the diuretic must be adjusted according to individual needs over time. In selected asymptomatic euvolaemic/hypovolaemic patients, the use of a diuretic drug might be discontinued.
Angiotensin receptor neprilysininhibitor
Background
Currently, blockade of the RAAS is the cornerstone of the treatment of HF. However, the combination of RAAS blockade with inhibition of neprilysin, an enzyme that degrades natriuretic peptides , has recently emerged as a potentially superior treatment strategy . In July 2015, the Food and Drug Administration approved sacubitril/valsartan for use in patients who have chronic and stable but symptomatic HF and who have an LVEF of less than 40%. The drug should be used in conjunction with other HF therapies but in place of ACE inhibitors or ARBs, and is contraindicated in patients with a history of ACE inhibitor or ARB-induced angioedema.
Mechanism of action
Clinical efficacy
Is It Best To Avoid Grain
Though no definitive conclusions have been made, veterinary researchers, nutritionists and the FDA continue to investigate the cause of diet-induced heart muscle disease . This leaves many pet owners wondering if they should avoid feeding grain-free diets, especially for dogs with heart disease or at risk for heart disease.
Feeding a grain-free diet may have less to do with the problem, and the bigger concern seems to be dog foods with high levels of peas, lentils and chickpeas , Dr. Lefbom says. With so many diets on the market, there is no easy answer to what to feed each individual dog.
Your best bet is to talk to your veterinarian about the best food to feed your dog, and what types of formulations or ingredients to avoid.
You May Like: Is Blood Pressure The Same As Heart Rate
Also Check: How Does Diabetes Cause Heart Disease
Study Design And Data Sources
We conducted a nested case-control study using the databases of the Quebec Health Insurance Board , the Institut de la statistique du Québec , and the Quebec Registry of Hospitalizations. These databases include information on patient demographics, vital status, in-hospital and outpatient medical diagnoses, and the medical services used by all permanent residents of Quebec province. The RAMQ drug plan database contains information on prescription drugs for Quebec residents not covered by a private drug insurance group plan, welfare recipients and all seniors, except those living in long-term care facilities.
Medications To Avoid In Patients With Heart Failure
The number of patients being diagnosed with heart failure is increasing worldwide, and thus we need to know which medications to avoid or be cautious with prescribing that may cause or exacerbate this medical condition. So, we decided to talk about these medications, how they cause these adverse events in these patients, and their mechanism of action.
How these medications cause adverse events in HF patients?
Overall, these medications might cause these adverse effects by one of the following mechanisms: 1) causing direct myocardial toxicity 2) by negative inotropic effect 3) chronotropic effects 4) by exacerbating hypertension 5) by delivering a high sodium load or 6) by drug-drug interactions that limit the beneficial effects of HF medications.
Here, we will talk briefly about the common medication classes that should be avoided in heart failure and their mechanism of causing these adverse events.
Recommended Reading: How To Figure Maximum Heart Rate
Connect With A Barostim Ambassador
Barostim Ambassadors are real patients who volunteer to have conversations with potential patients about their experience.
The patient testimonials & heart failure treatment reviews above relate to accounts of an individuals response to treatment. The accounts are genuine, typical & documented. Responses to the treatment can & do vary. Not every response is the same. Patients were not compensated. Please review the safety information provided on this site& note that this therapy is not for everyone. Furthermore, the information on this site should not be used as a substitute for talking with your doctor. Always talk with your doctor about diagnosis and treatment information.
Stages Of Heart Failure
In 2001, the American Heart Association and American College of Cardiology described the Stages of Heart Failure. These stages, which were updated in 2005, will help you understand that heart failure is often a progressive condition and can worsen over time. They will also help you understand why a new medication was added to your treatment plan and may help you understand why lifestyle changes and other treatments are needed.
The stages classified by the AHA and ACC are different than the New York Heart Association clinical classifications of heart failure that rank patients as class I-II-III-IV, according to the degree of symptoms or functional limits. Ask your doctor what stage of heart failure you are in.
Check the table below to see if your therapy matches what the AHA and ACC recommend. Note that you cannot go backward in stage, only forward.
The table below outlines a basic plan of care that may or may not apply to you, based on the cause of your heart failure and your special needs. Ask your doctor to explain therapies that are listed if you do not understand why you are or are not receiving them.
The New York Heart Association clinical classifications of heart failure rank people as class I-II-III-IV, according to the degree of symptoms or functional limits. You can ask your doctor if you want to know what stage of heart failure youâre in.
Also Check: How Low Should Your Heart Rate Be When Sleeping
