What Is Acute Heart Failure
Heart failure is a life-threatening condition. When it occurs, your heart is still working, but it cannot deliver oxygen-rich blood throughout your body. With acute heart failure, you experience a sudden, rapid decline in heart functioning and the amount of blood your heart can pump to the rest of your body.
Compensated Vs Decompensated Heart Failure
Compensated heart failure is the initial stage of heart failure where different structural and functional changes in the heart compensate for the reduction of cardiac output. Symptoms The patient is either asymptomatic or minimally symptomatic with minor symptoms such as grade I dyspnea and mild ankle swelling.
- Exertional dyspnea
Management Priority is given to the lifestyle modifications such as cessation of smoking, reduction of alcohol intake, avoiding stress and regular exercises in the management of compensated heart failure. Priority is given to the pharmacological interventions along with radiological and surgical therapeutic procedures in the management of compensated heart failure.
Chronic Decompensated Heart Failure
Doctors may prescribe diuretics to eliminate excess fluid buildup in people with chronic decompensated heart failure. Another common name for these drugs is water pills. They can also treat high blood pressure.
A person should inform a doctor of any other medications they are taking. Some medications, including thiazide diuretics or cyclosporine, can interact with heart medications such as digoxin .
Vasodilators are another class of medications that people with chronic decompensated heart failure may take. The explains that these widen the blood vessels and reduce blood pressure.
Read Also: How Long Do Heart Attack Last
Causes Of Acute Heart Failure
Many conditions can weaken or damage the heart over time. This can lead to heart failure.
With chronic heart failure, your heart tries to adapt to the additional strain over time until it just cant adapt anymore. Thats when acute heart failure happens.
Its also possible for acute heart failure to happen even in people who otherwise seem healthy. There are a number of conditions that can put a sudden strain on your heart.
Causes of acute heart failure include:
- coronary artery disease, which can cause a narrowing of the arteries
- heart attack, which causes damage to the heart muscle and is often caused by coronary artery disease
- use of certain illegal drugs, such as cocaine
- chemotherapy and radiation treatments
In the United States, Black and Hispanic people receive heart failure diagnoses more often than people from other racial or ethnic groups. And Black people in the United States are also at the highest risk of dying from heart failure.
These trends are related to racism and inequities in healthcare, according to the American College of Cardiology.
To diagnose acute heart failure, your doctor will run certain tests. Your doctor can then identify your stage of heart failure, to help find the right treatment for you.
Palliative And Hospice Care
Someone living with a serious condition like heart failure can access palliative care at any stage of their condition. Palliative care is intended to support overall wellness and quality of life and can happen alongside other treatments.
With very severe heart failure, people may choose to access hospice care to receive supportive care at the end of life.
You May Like: Congestive Heart Failure Prevention
Factors Associated With 2
Table 2 Comparison of survivors and non-survivors using age-adjusted Cox proportional hazards regression models
Age, sex, creatinine clearance, anaemia, systolic blood pressure, myocardial infarction, weight loss, body mass index, MNA-SF score, ADL score, Timed Get-Up-and-Go score, and MMSE score were available for the multivariable Cox model. Mobility impairment, lower body mass index, and MNA-SF category were not introduced into multivariable models, as they correlated with functional impairment and recent weight loss, respectively . Because of their association with other parameters, anaemia, myocardial infarction, and cognitive impairment were not independently associated with death in the multivariable model . No significant interactions were found between variables associated with 2-year mortality. By multivariable analysis , five factors were independently associated with 2-year mortality, namely, male sex, age older than 85 years, higher number of impaired ADL items, recent weight loss, and lower systolic blood pressure. A trend was noted for renal failure. The final model had good calibration and acceptable discrimination . The HRs estimated after bootstrap resampling were close to those of the original model, suggesting excellent internal validity. All five factors were also independently associated with 1-year mortality .
Table 3 Factors independently associated with 2-year mortality by multivariable analysis
Who Experiences Acute Heart Failure
Acute heart failure occurs in people with or without previous heart issues:
- Acute decompensated heart failure occurs in people with heart conditions, such as coronary artery disease.
- De novo acute heart failure occurs in people with no history of heart disease. They have ongoing health conditions, like diabetes, that damage their heart.
Don’t Miss: What Should My Heart Rate Be When Exercising
Types Of Heart Failure
The chambers where your blood is pumped out of the heart are called ventricles. These may stiffen so that they no longer fill properly. Or, if your heart muscle becomes weak, the ventricles can fail to pump hard enough.
Heart failure can begin on either the left or right side of your heart. Sometimes, both sides may fail at the same time. The different types of heart failure correspond to where the heart is failing:
D Physical Examination Findings
The physical exam should focus on several key features including vital signs, the cardiopulmonary examination, neck veins, and extremities. Patients may be tachycardic and have blood pressure derangements.
Hypertensive patients are more likely to have preserved systolic function, whereas hypotensive patients are more likely to be in a low-cardiac output state carrying a worse prognosis. Pulmonary examination often reveals crackles, consistent with interstitial pulmonary edema, or wheezing.
Examination of the neck veins provides diagnostic and prognostic information. Elevation of jugular venous pressure is indicative of elevated right-sided filling pressures, which in patients with advanced heart failure, predicts elevated left-sided filling pressures in 80% of cases.
Cardiac auscultation may reveal either a third and/or a fourth heart sound suggestive of cavitary dilation or decreased compliance of the left ventricle respectively. A new or changed murmur usually represents valvular abnormalities, which may reflect altered ventricular geometry.
Abdominal examination may reveal hepatomegaly as a result of passive congestion, hepatojugular reflux or ascites. Extremity examination may reveal peripheral edema, particularly in the dependent portions of the body. Perfusion may be assessed by capillary refill time and physicians perception of skin temperature .
Don’t Miss: Why Does My Resting Heart Rate Fluctuate
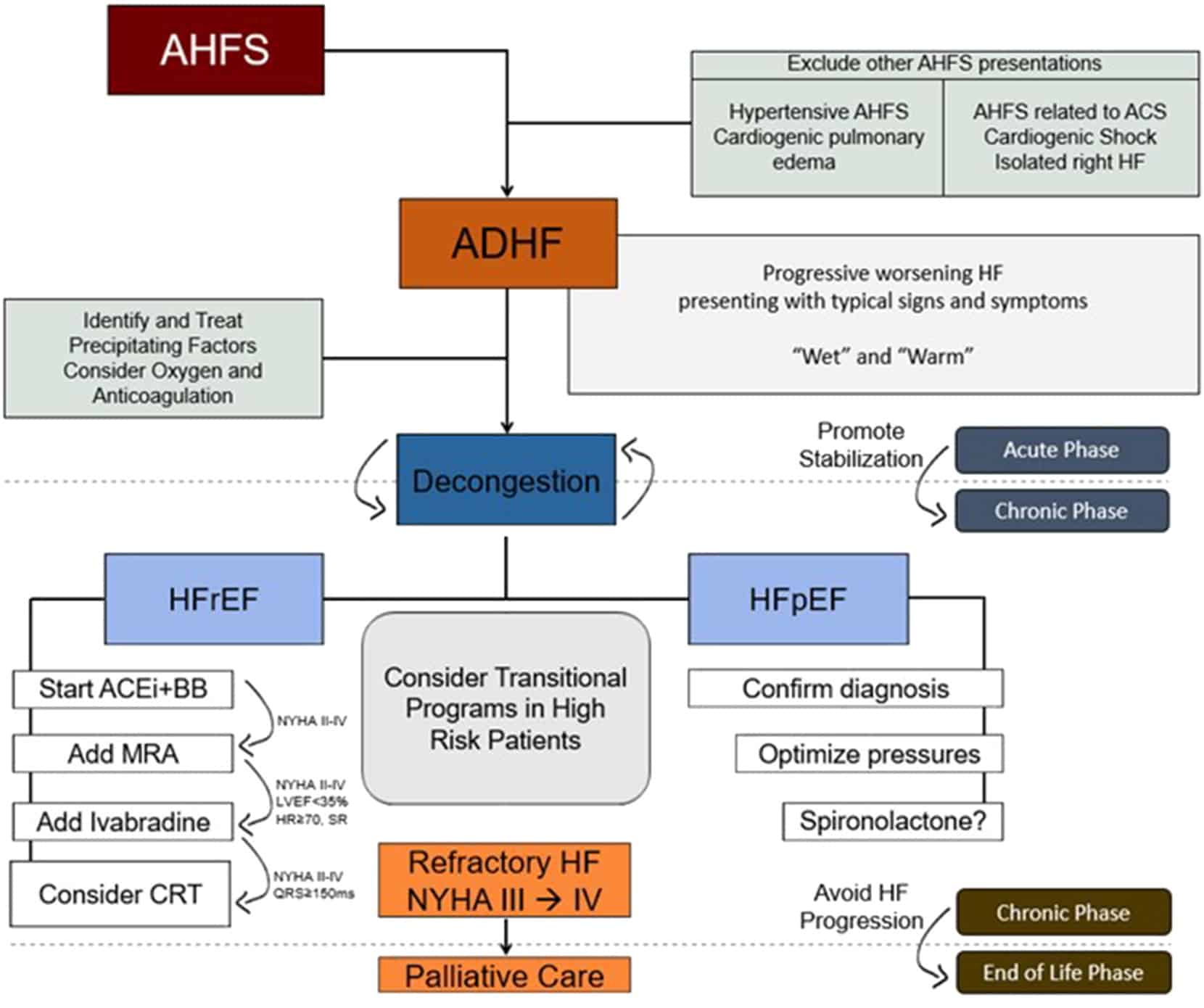
Classification Of Acute Heart Failure
The definition of AHF presented here is broad and there have been many attempts to stratify this further . Although characterised by a distinctive set of signs and symptoms, a major challenge in classifying AHF as a single entity is that the patient population is not uniform. Patients admitted with HF exhibit a wide spectrum of disease and range from those with severe LV systolic dysfunction and low cardiac output to those with severe hypertension and normal or near-normal LV systolic function. The majority of patients with AHF lie between these extremes and therefore also demonstrate a distribution of underlying pathology and precipitants, leading to the common endpoint of fluid overload.
This is a neat classification system and focusses the treating physician towards the management of the underlying cause of AHF. However, given patients often present with a range of co-morbidities, the reasons for decompensation may not be apparent at initial presentation or indeed, there may be multiple contributing factors. Practically speaking, therefore, it may be more prudent to stratify patients with AHF based on their initial clinical presentation. This allows the attending physician to identify those most at risk in order to direct specific interventions such as instituting ionotropic agents and/or mechanical circulatory support.
Acute Heart Failure Diagnostic Workup
The diagnostic workup for acute heart failure begins with a rapid assessment of the patients health history, including a detailed account of any symptoms, history of heart disease in the family, whether the patient smokes, what medications they take, and if they have any other medical conditions.
The physical examination should be comprehensive. Patients with acute decompensated heart failure will present a general appearance that includes anxiety, diaphoresis, and poor nutritional status.6
Physicians often use the Framingham Diagnostic Criteria for Heart Failure, which requires the presence of either two major criteria or one major and two minor criteria to make the diagnosis.5 The criteria are as follows:5
Read Also: What Does Bpm Stand For In Heart Rate
Risk Factors For Elderly Acute Decompensated Heart Failure Patients With Diabetic Nephropathy: A Retrospective Study
Citations:
- MLA style: “Risk factors for elderly acute decompensated heart failure patients with diabetic nephropathy: A retrospective study..” The Free Library. 2022 Knowledge Bylanes 17 Dec. 2022
- Chicago style:The Free Library. S.v. Risk factors for elderly acute decompensated heart failure patients with diabetic nephropathy: A retrospective study..” Retrieved Dec 17 2022 from
- APA style: Risk factors for elderly acute decompensated heart failure patients with diabetic nephropathy: A retrospective study.. > The Free Library. . Retrieved Dec 17 2022 from
What Happens When A Patient Decompensated
In medicine, decompensation is the functional deterioration of a structure or system that had been previously working with the help of allostatic compensation. Decompensation may occur due to fatigue, stress, illness, or old age. When a system is “compensated”, it is able to function despite stressors or defects.
Don’t Miss: Fast Heart Beat Rate
Treatment Options For Acute Heart Failure In Advanced Development Stage
Despite a considerable effort, few clinical trials have demonstrated significant improvements in long-term outcomes for patients with ADHF. Mortality remains high and patients are likely to experience frequent hospital readmissions therefore, the development of new therapies is warranted. Below, we review the currently available data for several promising investigational agents in advanced stages of clinical development for the management of ADHF.
Epidemiology Of Acute Heart Failure
Our knowledge of the epidemiology of AHF is informed by a number of large-scale registries conducted in the USA, including ADHERE and OPTIMIZE-HF , Europe including the European Heart Failure Surveys I and II and the ESC-HF Pilot Registry , as well as the international ALARM-HF registry. This allows for a comprehensive description of patients presenting with AHF however, there are three key demographic details to highlight. Firstly, patients are predominantly male with a mean age at presentation of > 70 years which is consistent with the epidemiology of both ischaemic heart disease and CHF. Secondly, and related to the first point, the majority of patients have a previous history of HF and present with decompensation of their existing disease rather than de novo AHF. Finally, as discussed earlier, these patients exhibited a high burden of co-morbid disease including diabetes mellitus and chronic obstructive pulmonary disease .
Don’t Miss: Congestive Heart Falure
Managing Acute Decompensated Heart Failure
Approximately 5 million Americans have heart failure and at least 550,000 more are newly diagnosed each year. HF is the most common Medicare diagnosis-related group. In 2006, direct costs associated with the condition reached nearly $30 billion.
Although HF incidence hasnt declined in the past 20 years, overall survival has improved. Better risk factor identification, early intervention, and appropriate long-term care management have contributed to improved survival.
Heart failure definedHF is a progressive syndrome diagnosed from both clinical findings and structural and functional cardiac changes. Most people with symptomatic HF have some degree of left ventricular dysfunction, as from hypertension, myocardial infarction, myocardial infection, or genetic abnormalities.
Left ventricular ejection fraction is the percentage of blood pumped by the left ventricle with each heart beat. The Heart Failure Society of America describes two broad types of HFone with reduced LVEF and one with preserved LVEF. Measured by echocardiography, ejection fraction normally is 55% or higher. Patients with an EF of 35% or lower may not have HF signs and symptoms right away and at times may compensate fairly well. In the past, the term congestive heart failure was used to denote EF below 35%.
Also assess for signs and symptoms of:
American Heart Association. Heart Disease and Stroke Statistics2008 Update. www.americaheart.org/presenter.jhtml?identifier=3054076. Accessed December 29, 2008.
What Is Decompensated Heart Failure
- Bookmark for later
Decompensated heart failure, also called Acute Decompensated Heart Failure , occurs in patients with pre-existing heart failure. It refers to a worsening of symptoms due to fluid retention .1 These symptoms can impair the day-to-day quality of your life. For example, developing congestion in the lungs can cause wheezing, coughing, or an inability to sleep laying down at night.2 This can make it more difficult to breathe. ADHF can also cause fatigue, making you feel more tired when doing everyday activities. This can interfere with carrying out household activities or tasks at work.2
Don’t Miss: What Are The Symptoms Of Congestive Heart Failure
A History Part I: Pattern Recognition:
The cardinal manifestations of ADHF are dyspnea, fluid retention, and fatigue. Fluid retention, commonly leads to pulmonary congestion and peripheral edema in patients with ADHF.
Patients may present with progressive weight gain, lower extremity edema, increasing dyspnea on exertion, or dyspnea at rest. Patients may report orthopnea and/or paroxysmal nocturnal dyspnea.
Patients may note abdominal bloating or a decrease in appetite. Some patients may present with fatigue or even altered mental status. Some patients may present with sudden onset of dyspnea.
Common factors that precipitate ADHF may include noncompliance with medical regimen, sodium and/or fluid restriction, acute coronary syndromes, uncorrected high blood pressure, atrial fibrillation and other arrhythmias, pulmonary embolus, use of NSAIDs, excessive alcohol or illicit drug use, endocrine abnormalities, exacerbation of pulmonary diseases, or concurrent infections such as pneumonia.
Common causes of ADHF
Lack of compliance with HF medications
New medication
Substance abuse
Congestion And Organ Dysfunction
In the heart, elevated ventricular filling pressures lead to increased ventricular wall tension, myocardial stretch and remodelling, contributing to a progressive worsening in cardiac contractility, valvular regurgitation and systemic congestion. In response to the increased wall tension, circulating natriuretic peptides are physiologically released by atrial and ventricular cardiomyocytes as a compensatory mechanism, and often high-sensitivity cardiac troponins are detectable in a large proportion of patients with AHF, revealing nonischaemic myocyte injury or necrosis. Increases in left atrial pressure and mitral valve regurgitation will increase the hydrostatic pressure in the pulmonary capillaries, thereby increasing fluid filtration rate from the capillaries to the pulmonary interstitium, causing lung stiffness and dyspnoea. Notably, the relationship between hydrostatic pressure and interstitial fluid content is rather complex, as other mechanisms are involved in fluid homeostasis. For example, the lymphangiogenic factor VEGF-D has been found to regulate and mitigate pulmonary and systemic congestion in patients with HF or renal failure,,. Indeed, in the early stage of lung congestion, the lymphatic system can cope with the large volume of interstitial fluid, but eventually, the drainage capacity is exceeded. Hence, fluid moves to pleural and intra-alveolar spaces causing pleural effusion and pulmonary oedema.
You May Like: Scars From Heart Surgery
Summary Compensated Vs Decompensated Heart Failure
Adaptive changes in the cardiac tissues maintain an optimal cardiac output although the damages to the myocardium in heart failure is known as the compensated heart failure. Failure of these adaptive changes to maintain the cardiac output at the same optimal level with disease progression is known as the decompensated heart failure. In compensated heart failure, the patient remains either asymptomatic or minimally symptomatic whereas in decompensated heart failure the patient becomes severely symptomatic. This is the main difference between compensated and decompensated heart failure.
Reference:
1.Kumar, Parveen J., and Michael L. Clark. Kumar & Clark clinical medicine. Edinburgh: W.B. Saunders, 2009.
Image Courtesy:
1. Heart diagram-en By ZooFari Own work via Commons Wikimedia2. 1846050 via Pexels
Diagnosis And Treatment Of Acute Heart Failure
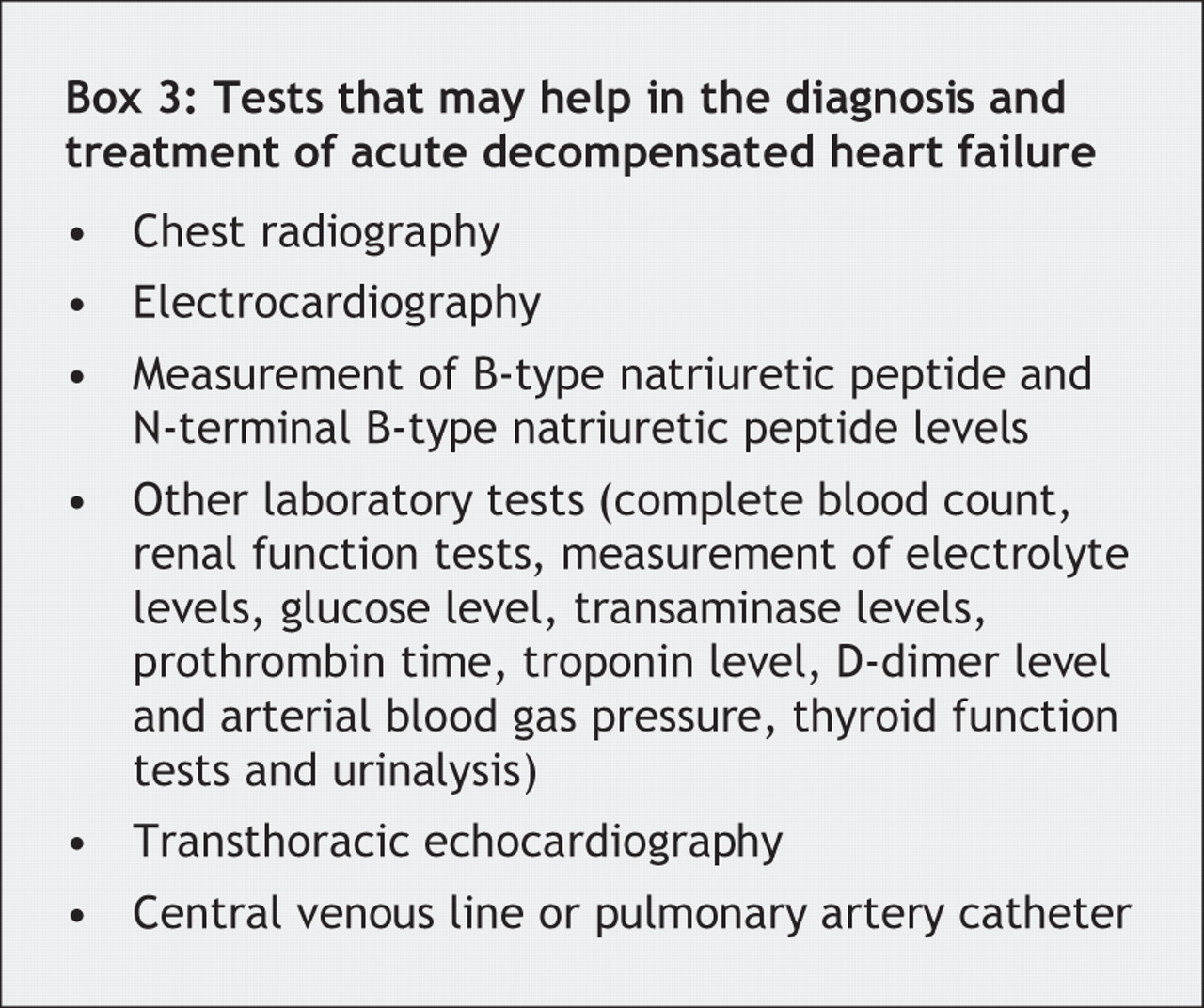
If any signs and symptoms of heart failure develop, especially if there has not been any previous diagnosis of heart failure, it is important to see a healthcare professional quickly. After performing a physical exam and obtaining information about current symptoms and your medical history, your doctor may order the following tests:
Heart Failure Doctor Discussion Guide
Recommended Reading: Congestive Heart Failure Physical Exercise
Minor Acute Heart Failurecriteria
- A decrease in vital capacity by one-third of the maximal value recorded
Diagnostic testing that can also be used to help diagnose acute heart failure, as well as potential underlying etiologies, includes blood tests, chest x-ray, electrocardiogram, echocardiogram, stress tests, cardiac computerized tomography scan, magnetic resonance imaging , coronary angiogram, and myocardial biopsy.7
Dual Serca2 Stimulation And Na
Sarcoplasmic reticulum Ca2+ adenosine triphosphatase-2a has a vital role in the regulation of Ca2+ in the cardiomyocyte and its expression and function is diminished in HF. SERCA2a has therefore been identified as a potential therapeutic target for HF.
Istaroxime is a luso-inotropic, small-molecule, Na-K ATPase inhibitor that stimulates SERCA2a-ATPase activity and accelerates calcium cycling in HF by relieving phospholamban inhibition. In the phase II Hemodynamic Effects of Istaroxime in Patients With Worsening HF and Reduced LV Systolic Function trial , istaroxime significantly reduced PCWP and increased systolic BP vs. placebo in patients with ADHF who had not received IV inotropes and had serum creatinine levels 3.0 mg/dL. Furthermore, istaroxime-treated patients showed significant improvements in several parameters of left ventricular diastolic stiffness, compared with placebo. An additional phase II trial evaluating the efficacy and safety of istaroxime in patients with ADHF is planned.
Recommended Reading: Is Blood Pressure And Heart Rate The Same Thing
Diagnosis Of Acute Heart Failure
The diagnosis of acute heart failure in critically ill patients can be more difficult than is commonly recognised. Although the underlying pathology in most patients with acute heart failure on intensive care will be coronary artery disease, other diagnoses must be considered .
It is also important to reassess critically the patient referred with a diagnosis of acute heart failure to decide whether this is indeed the primary problem. The history, examination and initial investigations with routine blood tests, electrocardiogram and chest X-ray may be compatible with this diagnosis but many such patients are elderly with multiple co-morbidities, and deciding whether the patient is suffering from a primary myocardial pathology as opposed to a pulmonary problem or indeed systemic sepsis6 can be difficult. Equally, patients believed to have a primary respiratory problem may fail to wean from ventilatory support because of a failure to realise that they have left ventricular failure with a high left atrial pressure and incipient pulmonary oedema, causing a reduction in pulmonary compliance, an increased work of breathing and respiratory distress when ventilatory support is withdrawn.
Further investigations that can help to confirm or refute an initial diagnosis of acute heart failure are echocardiography and the measurement of biomarkers such as natriuretic peptides and cardiac troponins.
Peter S. Pang, Marco Metra, in, 2020
