Body Mass And Weight Changes Over Time
Patients in the CHARM programme had regular visits and each patient’s weight was recorded according to each centres usual practice. These were planned to be at baseline, 2, 4, 6 weeks, 6 months, and then every 4 months thereafter until a maximum of 42 months.
Actual timing of visits varied and was assigned to the planned visit when within 1 week of the intended timing , within 1 week before or 5 weeks after or within 2 months of intended timing for the 6 month visit onwards. Height was recorded at baseline, enabling body mass index to be calculated.
How Palliative And Hospice Care Can Help With End
Both palliative and hospice care focus on the whole person, including their physical, emotional, social, and spiritual needs. The main difference is that palliative care can be given at any time during a serious illness, and hospice care is given near the end of life typically when a persons prognosis is six months or less.
Palliative and hospice care can also provide help with making difficult treatment decisions, such as whether to be resuscitated if the persons heart stops, or whether to have a tube placed in their throat to help them breathe.
Similarly, people with end-stage heart failure may need to decide when to disable certain medical devices implanted in their body:
- Implantable cardioverter defibrillator . Patients can have the shock function turned off, or not replace the battery when the current one runs out. Electrical shocks from ICDs can cause unnecessary distress for patients and loved ones at the end of life.
- Left ventricular assist device . Typically, the patient decides when this heart pump will be shut off before it is implanted. The decision can be discussed again as the end of life nears.
How Can I Help My Dog With Congestive Heart Failure
Treatment
What is a high respiration rate for a dog?
A typical healthy dog will take between 15 to 35 breaths per minute while at rest. . So, anything above 40 breaths per minute while your dog is at rest is considered abnormal and certainly worth investigating.
What are the signs of worsening heart failure in dogs?
Coughing when at rest or sleeping, excessive panting, persistent loss of appetite, a swollen belly, and pale or bluish gums are also signs associated with heart failure. The dog will develop generalized weight loss and muscle wasting due to the effects of CHF on other body systems.
Also Check: Why Does My Heart Rate Fluctuate So Much
Support Them To Make Decisions About Treatments
As well as having an advance care plan, patients should be given the chance to discuss the following issues:
- Whether to deactivate an implantable cardioverter defibrillator , if they have one. This can prevent the ICD activating at the end of life, which can be distressing.
- What the patient would want to happen if they had a cardiac arrest. They may decide they do not want to have cardiopulmonary resuscitation .
- When to stop medication that no longer reduces symptoms or improves their quality of life. This can be a difficult conversation and it’s best carried out sooner rather than later. Make sure the patient and the people important to them understand what changes are being made to their medication and why.
What Is The Importance Of Ejection Fraction
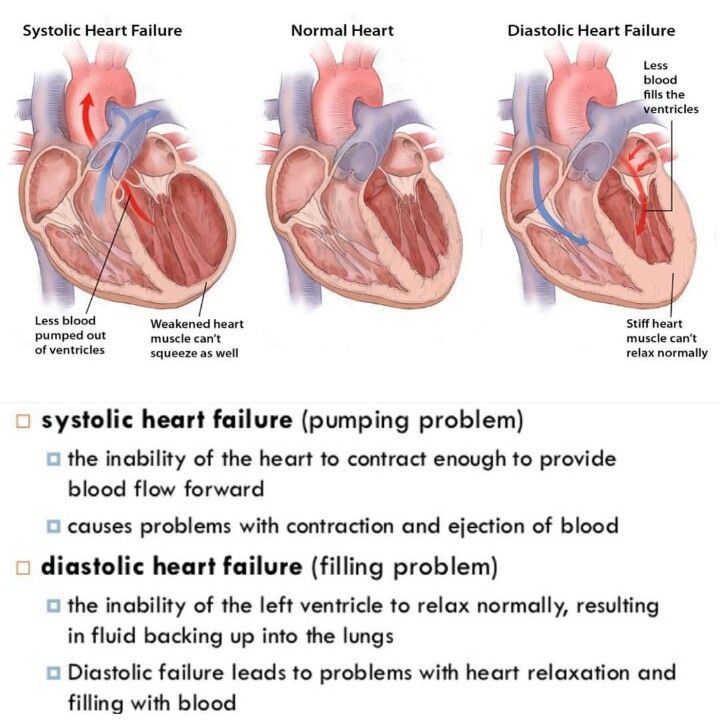
Your ejection fraction is one way to measure the severity of your condition. If its below normal, it can mean that you have heart failure. Your ejection fraction tells your healthcare provider how good of a job your left or right ventricle is doing at pumping blood. Usually, your EF number is talking about how much blood your left ventricle is pumping out because its your heart’s main pumping chamber.
Several non-invasive tests can measure your EF. With this information, your healthcare provider can decide how to treat you or find out if a treatment is working as it should.
A normal left ventricular ejection fraction is 53% to 70%. An LVEF of 65%, for example, means that 65% of the total amount of blood in your left ventricle is pumped out with each heartbeat. Your EF can go up and down, based on your heart condition and how well your treatment works.
Recommended Reading: What Is Heart Valve Disease
Small Changes Make A Big Impact
The influence of body weight on heart disease is not one to be taken casually. Being overweight can have serious and far-reaching consequences for the health of your heart and the likelihood of developing other seriously.
However, even a small weight loss can reduce the risk factors significantly. Losing weight not only involves filling your diet with nutritious foods, but it also means creating a calorie deficit.
This deficit doesnt have to be extreme to see significant weight loss. Reducing daily calorie intake by 500 calories, while increasing the general activity level to at least 90 minutes a day can be an effective way to bring the weight down to a healthier level.
B: Delivery Of Health Care
B1: Perceptions regarding care
B1.a: Appropriateness of care
The interviewed patients assessment of the quality of medical and nursing care varied depending on whether they thought the treatment was appropriate, necessary and met their needs. If decisions about medical treatment, prescriptions and home visits made by the professionals do not meet a patients expectations, they may be perceived as inadequate or wrong. Treatment of pain was particularly highlighted: The fact that patients often perceive pain as an expression of complete suffering not attributable to any particular cause leads to a type of indifference that makes any medical help inconceivable. The following quotation clearly illustrates this perception of ubiquitous suffering, which the patient repeatedly mentioned in every interview.
Patient HD12, T2 : I only want to feel better. But it seems its not to be, nothing good. Being ill, theres nothing wanted, nothing needed, its always the same. I dont need anything, I can be quite alone. Pain everywhere
Patient HD06, T1 : So you know, if a patient is really ill, yes, its good when you have someone who looks after you. I mean, I do not want too much care, it would be too much responsibility for me, you know. But if youre not feeling well, its good to have someone.
B1.b: Continuity of care
B2.a: Interaction in the processes of care
B2.b: Specific aspects in physician-patient interaction
B3: Meaning of family
Don’t Miss: What Can Cause Your Heart Rate To Be High
Can Heart Failure Be Prevented Or Avoided
Heart failure is the result of other diseases or conditions weakening your heart. These can include coronary artery disease, high blood pressure, and diabetes. The best way to avoid heart failure is to prevent those conditions. The following can help you maintain a healthy lifestyle:
If you do have a condition such as high cholesterol, high blood pressure, or diabetes, you need to manage it. Keep levels under control and take any medicines youve been prescribed.
You May Like: How Does Smoking Relate To Heart Attack And Atherosclerosis
Supporting Those Around The Patient
Those close to the patient may also need emotional and practical support. They may need:
- information about heart failure to help them understand the symptoms and treatment options
- support if they’re caring for the patient
- time to relax or look after their own health.
If the patient’s heart failure is due to an inherited heart condition, their family may have concerns about their own health. Talk to them about their worries. It might be appropriate to refer immediate family members to a clinic which specialises in inherited heart conditions. This may have been done when the patient was first diagnosed.
Inherited heart conditions services offer specialist assessment and investigations, genetic counselling and testing. GPs can refer to this service.
Recommended Reading: Heart Valve Disease Treatment Without Surgery
What Can I Do About It
Some people try eating smaller amounts more often. This helps reduce the sensation of feeling full or bloated.3 If your appetite is poor, try selecting foods that you really feel like eating, that provide the most nutrition, or are easy to digest. This can make eating more pleasant or easier to tolerate.2Doctors dont recommend forcing a person with heart failure to eat because it can be uncomfortable. In the later stages, considered advanced heart failure, forcing food will not change the outcome or help people live longer.2
I Decline In Clinical Status Guidelines
These changes in clinical variables are listed in order of their likelihood to predict poor survival, the most predictive first and the least predictive last. No specific number of variables must be met, but fewer of those listed first and more of those listed last would be expected to predict longevity of six months or less.
Don’t Miss: What Time Of Day Are Heart Attacks Most Common
Imaging And Other Tests
Other tests provide pictures of the heart and surrounding structures or show how well the heart is working:
- Electrocardiogram : An electrocardiogram test uses small sensors to measure heart rate , rhythm and electrical impulses.
- Chest X-ray: A chest X-ray is a picture of your lungs, heart and surrounding structures. It can show whether there is fluid in your lungs from heart failure, or if your heart muscle is enlarged.
- Echocardiogram : Echocardiography uses sound waves to create images of your heart. It can show how thick the heart muscle has become, as well as measure ejection fraction.
- MRI: MRI is an advanced imaging test that takes pictures of the heart and surrounding structures. It helps determine your heart function and size and whether there are any changes in the heart muscle. A cardiac MRI may help your doctors identify causes of heart failure.
Our Favorite Apps And Gadgets
This app can help you to keep track of your liquid intake to avoid excess fluid buildup, which can lead to complications. You can also track your weight, since sudden increases in weight can be due to water retention. Another great thing about this app is that it alerts you if your blood pressure or weight gets high enough that you should tell your doctor. It also allows you to send reports on your fluid intake and weight to your healthcare provider.
This app, developed in partnership with the Heart Failure Society of America, is your one-stop shop for recording symptoms, vital signs, and medications to help you manage congestive heart failure. You can also track your information and keep a journal to maintain wellness and emotional health.
You May Like: Can Acid Reflux Cause Heart Palpitations
Should I Put My Dog Down If He Has Congestive Heart Failure
If the pet has a condition like congestive heart failure, or untreatable brain cancer a disease that will, unchecked, lead to a painful death the recommendation may be for euthanasia sooner instead of later.
Are dogs with congestive heart failure in pain?
Q: Is a dog with congestive heart failure in pain? A: No. Heart disease should not be painful for your pet.
Do dogs breathe fast when in pain?
Dogs experiencing pain may have a faster and more shallow breathing pattern than normal. They may also pant. You may even notice a change in the movement of the abdominal muscles and/or those of the chest. Both sets of muscles are involved in the breathing process.
What should my Dog breathing rate be if I have heart disease?
In general, all dogs and cats, with or without heart disease, have a breathing rate of between 15-30 breaths every minute. Lower rates are even possible and are no cause for concern as long as your pet is otherwise healthy. Breathing rates are much higher than this when dogs and cats are hot, stressed or active but that is OK.
What should the respiration rate of a dog with CHF be?
Dogs suffering from CHF and undergoing medical treatment may have a respiration rate of 40 breaths per minute, which is usually considered normal. The problem is when the breathing rate is very low or way over 40. This demands immediate medical attention.
What is a normal resting / sleeping breathing rate for dogs and cats?
When to put down a dog with congestive heart failure?
Why Am I Nauseous
Heart failure may cause a change in your appetite.3 If you are feeling full, bloated or nauseated you probably dont feel like eating. This can happen when there is decreased blood flow to the digestive system resulting in interference with the digestive process.1 This occurs because as the heart has to work harder to pump blood throughout the body, the volume of circulating blood decreases because the chambers of the heart dont fill and empty properly. Blood gets diverted from the digestive system to more vital organs like the brain.3
A poor appetite can also result from the accumulation of fluid in the liver and digestive system.3 Fluid accumulation, edema, is a common symptom of heart failure. We most commonly think of swelling in the legs and ankles, but it can happen anywhere in the body.3 The swelling can cause you to feel sick to your stomach. Nausea can lead to weight loss because it interferes with appetite and the bodys ability to absorb nutrients from the food.4
Swelling in the abdomen, sometimes called ascites, can also contribute to abdominal pain or tenderness.3,5 The accumulation of fluid that is responsible for the abdominal swelling can decrease your appetite and result in nausea as well as discomfort from the weight gain.
Don’t Miss: Does Fever Increase Heart Rate
Surgery For Heart Failure
- Coronary bypass surgery treats blocked arteries by removing healthy arteries from other parts of the body and using them to reroute blood around clogged arteries. This improves blood flow to the heart. If severely blocked arteries are a contributing factor to your heart failure, your physician may suggest bypass surgery.
- Heart valve replacement modifies a faulty heart valve to eliminate backward blood flow. A surgeon will either repair the valve, if possible, or replace it with an artificial valve.
- Ventricular assist devices are mechanical pumps implanted in the abdomen or chest and attached to the weakened heart. The devices help pump blood from the lower heart chamber to the rest of your body.
- Implantable cardioverter-defibrillators are implanted beneath the skin in the chest with wires leading through the veins and into the heart. These devices monitor heart rhythm and will shock the heart back into normal rhythm if it develops a life-threatening arrhythmia. They can also act as pacemakers, speeding up the heart if it begins beating too slowly.
- Cardiac resynchronization therapy, also known as biventricular pacing, sends electrical pulses to the hearts lower chambers to help them pump more efficiently.
- Heart transplant is an option in the most serious heart failure cases, when medication or surgery do not help. The procedure involves removing the damaged heart and replacing it with a healthy one from an organ donor.
How Long Does The End
| Life expectancy and remedies | |
| Left ventricular assist device or a heart transplant | 1 to 3 years |
Normally, when one has end-stage heart failure, their maximum life expectancy is around a year, and the minimum is around 6 to 9 months. When people try methods like left ventricular assist devices or getting a heart transplant to prolong their life, they can live around 1 to 3 years sometimes, but that is only around 50 to 60 percent of the people who get them. Heart failure is technically defined as the weakening of the heart, and this will slow down the heart bit by bit. This will make it hard for the heart to pump blood to all the other parts of the body as it actually should.
Though the heart starts weakening a long time before it shows symptoms, it can change first to try and pump blood like it used to. The heart might enlarge, stretch, or even pump more faster than it should. Normally, the heart beats about 60 to 100 times every minute if its normal.
Since the symptoms dont show themselves until it becomes serious, some people might not even notice they have heart issues until its very late. When the person doesnt know, it tends to get weaker and weaker as days pass by until the symptoms start showing.
You May Like: Who Did The First Open Heart Surgery
What Will Happen Towards The End
Heart failure usually gets gradually worse over time. It may eventually reach a point where it becomes very severe and its unlikely the person will live much longer.
Palliative care will usually begin when heart failure reaches this stage.
This involves treatment to help you feel as comfortable as possible, as well as being offered psychological, spiritual and social support for both you and your family.
You can choose whether you want palliative care and where youd like it to be provided.
Care can be provided:
