Summary Of Treatment Recommendations
Patients with HFpEF and symptoms of volume overload should be treated with diuretics.31 Hypertension should be treated according to appropriate guidelines.3 Although RCTs of several medications showed fewer heart failure hospitalizations, this benefit was offset by increases in hospitalizations for other reasons. Thus, in the absence of hypertension, the evidence does not support treating patients with HFpEF with any medication except diuretics. Additionally, RCTs of angioten-sin receptor blockers, nitrates, and spironolactone raise concerns about adverse effects, and physicians should avoid using these medications, if possible.18,2325 Similarly, physicians should avoid the use of digoxin in patients 65 years and older.27 Physicians should consider referring patients with HFpEF who can exercise safely for exercise training or cardiac rehabilitation. Comorbid atrial fibrillation or CAD should be treated.
Further Information On Cme
- Participation in the CME certification program is only possible online: cme.aerzteblatt.de. The submission deadline is 21.5.2021. Submissions by letter, e-mail, or fax cannot be considered.
- The completion time for all newly started CME units is 12 months. The results can be accessed 4 weeks following the start of the CME unit. Please note the respective submission deadline at: cme.aerzteblatt.de.
- This article has been certified by the North Rhine Academy for Continuing Medical Education. CME points can be managed using the uniform CME number . The EFN must be stated during registration on www.aerzteblatt.de or entered in Meine Daten and consent must be given for results to be communicated.The 15-digit EFN can be found on the CME card .
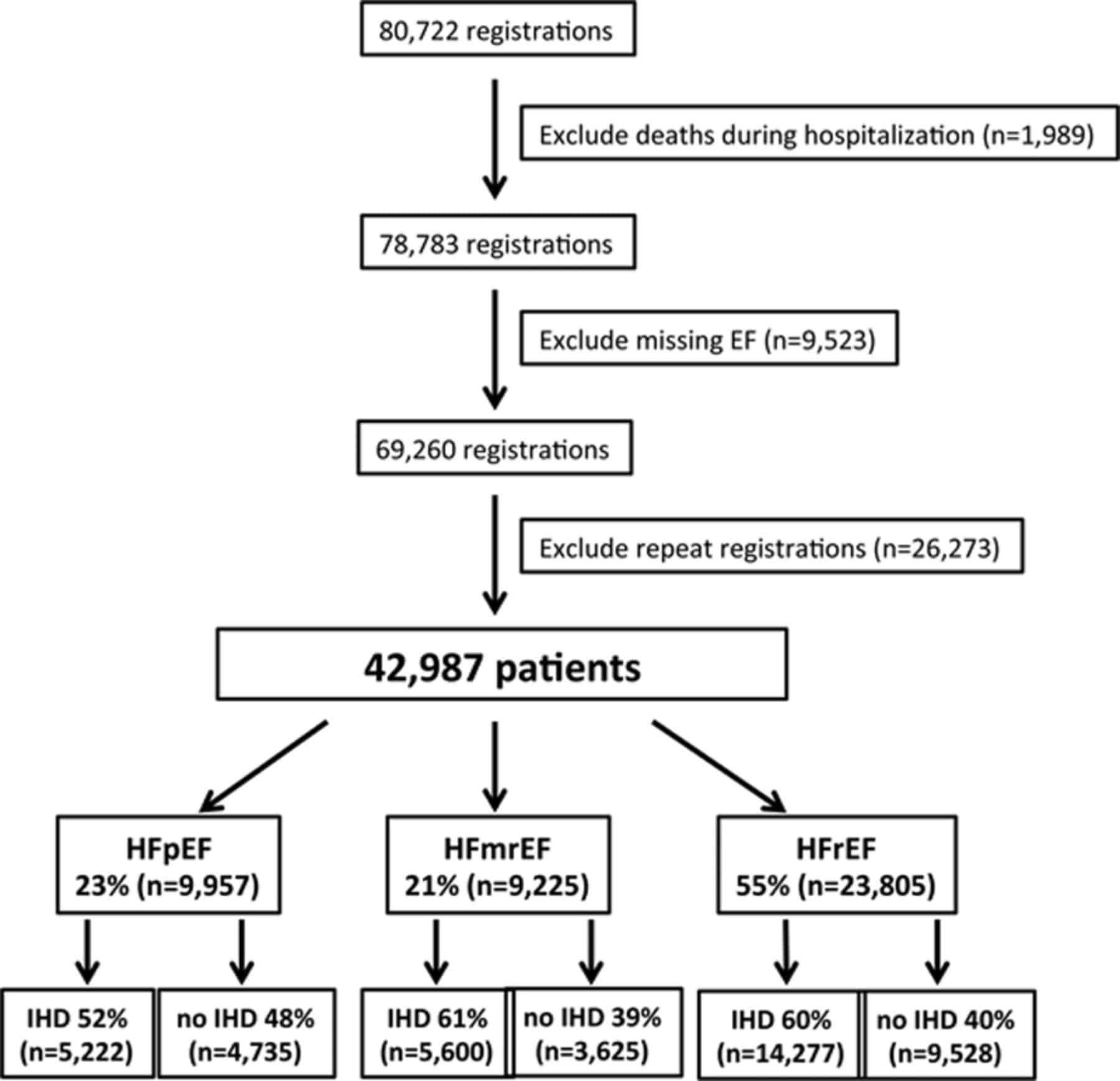
Proposed Prevalence And Etiology Of Hfmref
The prevalence of HFmrEF is estimated to be in the range of 10-20% of all HF patients . HFmrEF seems to have intermediate clinical characteristics and tends to have less clinical manifestations of HF when compared with HFrEF and HFpEF .
The background etiology is similar among the different types of HF. Patients with HFmrEF are more likely to have hypertension than patients with HFrEF and more likely to have ischemic heart disease and diabetes than patients with HFpEF. It has been hypothesized that HFmrEF is actually a subset of HFpEF that acquires coronary artery disease and is transitioning to HFrEF .
A recently published study showed that patients with HFmrEF are older and more likely female when compared with HFrEF , thus resembling HFpEF . Patients with HFmrEF also had a high comorbidity burden , which was higher than in HFrEF, and similar to HFpEF. Conversely, there was a high association with ischemic heart disease in patients with HFmrEF, similar to HFrEF.
Recommended Reading: After Exercise Heart Rate Recovery
Using Ejection Fraction In Diagnosis
When examined using an echocardiogram, a significant number of patients with heart failure are revealed to have normal ventricular ejection fraction. This condition was previously called diastolic heart failure its now referred to as heart failure with preserved ejection fraction.
Your doctor may mention one of these two EF-related scenarios:
Diseases Of The Circulatory Systemtype 2 Excludes
- 20162017201820192020202120222023Non-Billable/Non-Specific Code
Code First
- 20162017201820192020202120222023Non-Billable/Non-Specific Code
Applicable To
- end stage heart failure, if applicable
- combined systolic and diastolic heart failure
- Chronic systolic heart failure
You May Like: What Is Your Target Heart Rate
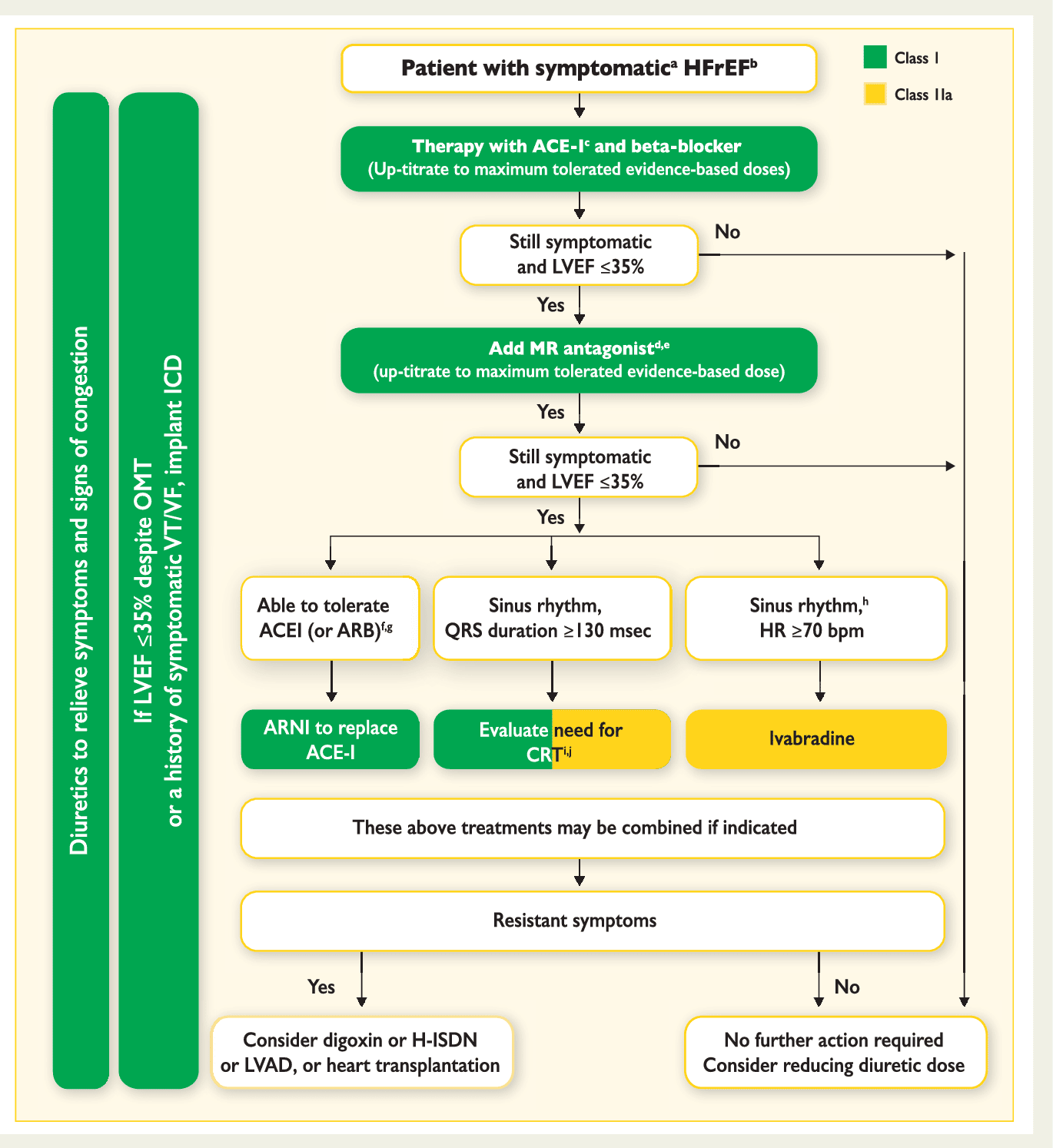
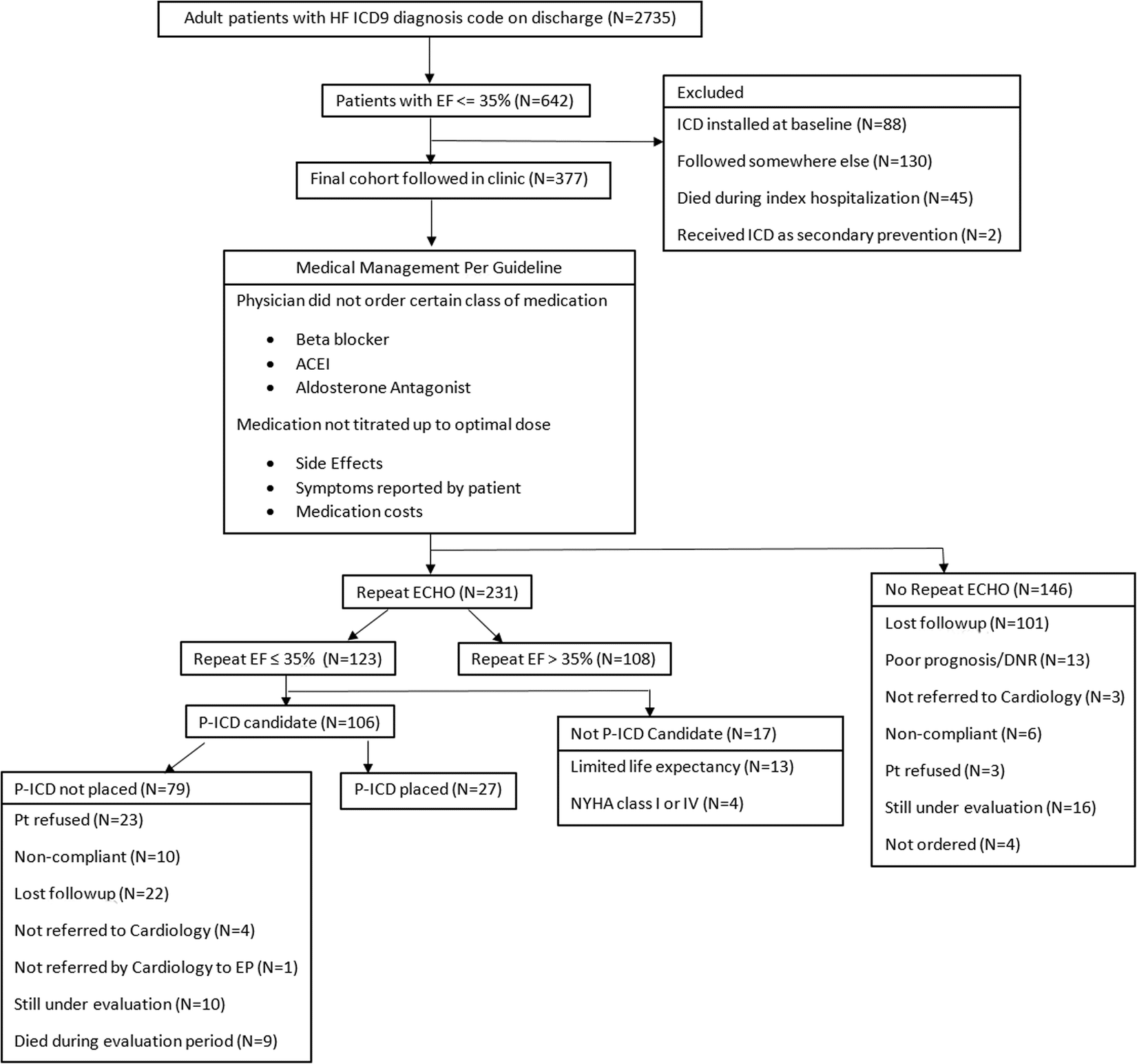
Primary Prevention Defibrillator Implantation
In symptomatic patients with an LVEF 35% defibrillator implantation is recommended in order to prevent sudden cardiac death.
The SGLT2 inhibitors are a highly promising drug group in patients with heart failure with and without diabetes mellitus. The 2016 ESC guideline stated that empagliflozin should be considered in patients with type 2 diabetes in order to prevent or delay the onset of heart failure. This recommendation was recently expanded to include the alternative SGLT2 inhibitors canagliflozin and dapagliflozin . The results of the DAPA-HF study have also been presented, showing a significant reduction in mortality and heart failure-related hospitalizations in HFrEF patients under dapagliflozin treatment irrespective of the presence of diabetes .
Success Of Resynchronization Therapy
A high percentage of LV pacing is crucial to treatment success.
Only around 20% of patients have a QRS duration of > 120 ms , meaning that cardiac resynchronization therapy is not indicated in the majority of HFrEF patients. Since modulation of the autonomic nervous system by means of vagal nerve stimulation was unsuccessful , baroreflex activation therapy and cardiac contractility modulation could represent potential alternative therapies in the future for patients with a narrow QRS complex. Both therapies are relatively new devices for heart failure and could be considered for HFrEF patients with a narrow QRS complex that remain symptomatic despite optimal guideline-compliant drug therapy. The Food and Drug Administration has already approved baroreflex activation therapy and cardiac contractility modulation in the USA to improve HFrEF symptoms. Hard data on improvement of prognosis are currently still pending. The German heart failure treatment guideline deems the available evidence on baroflex activation therapy and cardiac contractility modulation as hitherto insufficient for the purposes of making specific recommendations . Both devices currently play a secondary role in the clinical treatment of heart failure patients and are only used on the basis of individual assessments in specialized centers.
Recommended Reading: Tavr Vs Open Heart Surgery
Chronic Systolic Heart Failure
- 20162017201820192020202120222023Billable/Specific Code
- I50.22 is a billable/specific ICD-10-CM code that can be used to indicate a diagnosis for reimbursement purposes.
- The 2023 edition of ICD-10-CM I50.22 became effective on October 1, 2022.
- This is the American ICD-10-CM version of I50.22 – other international versions of ICD-10 I50.22 may differ.
- Applicable To annotations, or
Chf Icd 10 Codes And Guidelines
Most of the heart failure codes include in chapter 9 of ICD-10 CM manual, diseases of circulatory system, code range I00-I99.
- Combination code If patient has any type of heart failure and hypertension, it should be combined and coded as I11.0 eventhough physician has not linked both. It should not be coded combined if the medical record states the conditions are unrelated.
- Heart failure should be coded additionally when coding I11.0
- Do not code I11.9 when coding I11.0 .
- When coding biventricular heart failure it is necessary to code the type of left heart failure also according to the code also note with I50.82
Go by Failure, Heart to find correct codes for heart failure in ICD-10 CM manual index.
Look at the below scenarios to clearly understand the coding concepts of CHF.
CHF ICD 10 Code Example 1
Elizabeth is a 65 year old female who comes to emergency department for shortness of breath and leg edema from past 2 days. She came to visit doctor as the symptoms are getting worse. She has hypertension and takes Lisinopril for the same. She does not have chest pain or palpitation. She is not a smoker. Her family history includes heart disease for her mother and brother. Vitals showed temperature 97.3 F, heart rate 72 bpm, respiratory rate 25, BP 150/96 mmHg. Physical exam showed pitting edema on both the extremities, shortness of breath and dry skin. Physician ordered for blood tests, EKG and chest X-ray. This case was diagnosed as acute diastolic heart failure.
Don’t Miss: Does An Ekg Show Heart Attack
The Basis Of Drug Therapy
Treatment with ACE inhibitors and beta-blockers has led to a significant improvement in the prognosis of heart failure patients.
What is important is to appropriately increase the dose to the respective target dose. A large European study only recently demonstrated once again the prognostic relevance of appropriate dosing of ACE inhibitors and beta-blockers . ARB represent an alternative for patients unable to tolerate ACE inhibitors due to cough or angioedema. Table 2 provides an overview of the effects of heart failure treatment. The treatment is supported by diuretic therapy tailored to the patients symptoms.
Enhancing Healthcare Team Outcomes
Heart failure is a leading cause of hospitalization and represents a significant clinical and economic burden. The long-term goal of treatment is to avoid exacerbation of HF and decrease hospital readmission rates. It needs an interprofessional approach involving patients, physicians, nurses, pharmacists, families, and caretakers. Those strategies include early identification of high-risk patients, patient education, improving medication and dietary compliance, assuring close follow up, introducing end-of-care issues, and tele-home monitoring if available. Primary care and emergency department providers often are the first to make this diagnosis. Referal to cardiologists is often appropriate. Cardiology, medical/surgical, and critical care nurses administer treatment, provide education, monitor patients, and communicate with the rest of the team so that everyone on the healthcare team operates from the same data set. The managing clinician would do well to consult with a board-certified cardiology pharmacist when initiating pharmaceutical care in HF cases. Pharmacists also review medicines, check the dosages, detect drug-drug interactions, and stress to patients and their families the importance of compliance. In end-stage cases, hospice care and hospice nurses can work with the patient and their family to provide comfort care. These interprofessional collaborations will optimize patient outcomes in HF cases.
Read Also: How Does Smoking Relate To Heart Attack And Atherosclerosis
Angiotensin Receptor Neprilysin Inhibitors
Angiotensin receptor neprilysin inhibitors combine the established inhibition of the reninangiotensinaldosterone system with inhibition of the degradation of endogenously released natriuretic peptides.
Natriuretic peptides are released upon cardiomyocyte hypertrophy and cause an increase in intracellular cyclic guanosine monophosphate , natriuresis, as well as a reduction in renal renin secretion and a weakening of the angiotensin II-induced hypertrophic signal transduction in cardiomyocytes .
The only substance available in this drug group is the combination comprising the angiotensin II receptor blocker valsartan and the neprilysin inhibitor sacubitril. Neprilysin breaks down natriuretic peptides and various other vasoactive substances .
Treatment For Congestive Heart Failure
There are several medications that can be used to treat CHF. The first is ACE inhibitors. Angiotensin-converting enzyme inhibitors open up narrowed blood vessels to improve blood flow. Vasodilators are another option if you cannot tolerate ACE inhibitors. ACE inhibitors shouldnt be taken with the following medications without consulting with a doctor, because they may cause an adverse reaction. The second type of medication is beta-blockers. Beta-blockers can reduce blood pressure and slow rapid heart rhythm. Beta-blockers should be taken with caution with the following medications, as they may cause an adverse reaction. The third type of medication is diuretics. Diuretics reduce your bodys fluid content. CHF can cause your body to retain more fluid than it should. Thiazide diuretics cause blood vessels to widen and help the body remove any extra fluid. Loop diuretics cause the kidneys to produce more urine. This helps remove excess fluid from your body. Potassium-sparing diuretics help get rid of fluids and sodium while still retaining potassium. If medications arent effective on their own, more invasive procedures may be required. Angioplasty, a procedure to open up blocked arteries, is one option. Your cardiologist may also consider heart valve repair surgery to help your valves open and close properly.
The table below includes the most commonly used ICD-10 codes for Congestive Heart Failure:
| ICD-10 Chapter |
|---|
You May Like: Why Is My Resting Heart Rate 100
Study Outcomes And Covariates
Diagnoses documented within 12 months prior to the index date were analyzed if they were documented in at least three percent of the study population. A total of 37 diagnoses were available for analysis, including cancer , iron deficiency anemia , hypothyroidism , hyperthyroidism , diabetes mellitus type 2 , obesity , lipid metabolism disorders , dementia , depression , anxiety disorder , sleep disorders , hearing loss , primary hypertension , hypertensive heart disease , angina pectoris , myocardial infarction , coronary heart disease , nonrheumatic aortic valve disorders , atrial fibrillation and flutter , ischemic stroke , atherosclerosis , venous embolism and thrombosis , chronic bronchitis and COPD , asthma , gastro-esophageal reflux disease , gastritis and duodenitis , diverticular disease , hemorrhoids , NALFD , cholelithiasis , gout , osteoarthritis , spondylopathies , osteoporosis , chronic kidney disease , benign prostatic hyperplasia in men .
Types Of Heart Failure
The types are based on which part of the heart is affected.
Left sided heart failure : This is the most common type of heart failure found in medical record. It is related to the pumping of blood by left ventricle. This can be either Systolic or Diastolic.
Systolic It is also called HFrEF which means heart failure with reduced ejection fraction.
Diastolic Another term for this is HFpEF which means heart failure with preserved ejection fraction.
Right sided heart failure : It is related to the pumping of blood by right ventricle.
Biventricular heart failure : This is a type of heart failure in which ventricles of both the sides are unable to pump enough blood.
Also Check: Congestive Heart Failure Pacemaker
Acute On Chronic Systolic Heart Failure
- 2016201720182019202020212022Billable/Specific Code
- I50.23 is a billable/specific ICD-10-CM code that can be used to indicate a diagnosis for reimbursement purposes.
- The 2022 edition of ICD-10-CM I50.23 became effective on October 1, 2021.
- This is the American ICD-10-CM version of I50.23 – other international versions of ICD-10 I50.23 may differ.
- Applicable To annotations, or
Prognostic Profile Of Hfmref
The outcome of patients with HF with a wide range of LVEF was studied in the Candesartan in Heart failure: Assessment of Reduction in Mortality and morbidity Program. Patients with lower LVEF tended to have higher baseline New York Heart Association class. LVEF was the best predictor of fatal or non-fatal cardiovascular events, with the highest rates of mortality and rehospitalization in the HFrEF subgroup. The discriminatory effect of the LVEF for prediction of adverse outcomes was, however, limited above a LVEF of 45%. Patients with an LVEF over 45% had a much lower risk of adverse cardiovascular outcomes than those with reduced systolic function . This suggests that, in these patients, research should be conducted for the evaluation of additional factors to predict outcome.
In the Cardiovascular Health Study the mortality rate of HFmrEF was intermediate between that of HFrEF and HFpEF .
Among patients with HFmrEF, recovered systolic function was a marker of a more favorable prognosis despite similar clinical characteristics and cardiopulmonary response to exercise. It was also showed that most of the patients with HFmrEF remained with a LVEF between 40% and 55% after a median of 2.8 years of follow-up, suggesting that HFmrEF is not necessarily a transition step of the progression from normal LVEF to HFrEF or vice versa .
Don’t Miss: How To Stop Heart Palpitations From Anxiety
Symptoms Tests And Diagnosis
There may be one or multiple symptoms like shortness of breath, leg edema, fatigue, rapid heartbeat or chest pain. Doctor will verify the patients medical history as conditions like CAD, angina, hypertension, heart valve diseases and diabetes are risk factors for heart failure. After doing a physical examination, physicians may do cholesterol check, BNP blood test, chest X-ray, EKG, stress test, CT scan, MRI or coronary angiogram.
Treatment Of Comorbid Atrial Fibrillation And Cad
Atrial fibrillation is common in patients with HFpEF. The ACC/AHA and ESC guidelines recommend treatment of atrial fibrillation in these patients.3,5 Management includes identification and treatment of underlying causes , anticoagulation guided by appropriate risk stratification, and rate-control strategies using beta blockers, calcium channel blockers, and digoxin. No evidence supports a rhythm-control strategy unless rate control does not control symptoms.3,5 Complete revascularization is associated with improved mortality in patients with HFpEF and CAD who meet criteria for revascularization.3,30
Read Also: Consistently High Heart Rate
Basic Characteristics Of The Study Sample
The present study included 162,246 patients with heart failure and 162,246 patients without heart failure. The basic characteristics of study patients are displayed in Table . Median age of the study population was 76 years 52.6% were women. Table shows 37 diagnoses the proportions of which, with exception of dementia, were higher in HF patients than in controls. The proportions of cancer diagnoses were very similar in patients with and without heart failure. The highest prevalence was primary hypertension followed by lipid metabolism disorders and diabetes mellitus type II . In men, no significant difference was observed between patients with and without heart failure for cancer and hemorrhoids.
Table 1 Age and sex structure of the study sample .
Less Is More: Heart Rate Monitoring
As a result of the reduced cardiac output due to the reduced ejection fraction, the heart rate increases as a reflex. In heart failure patients, an elevated heart rate leads to less economical ventricular function and has been repeatedly associated with a poorer prognosis .
Treatment with the If channel blocker ivabradine is able to achieve a rate reduction in patients in sinus rhythm without the blood pressure-lowering effect of beta-blockers. In the SHIFT study, treatment with ivabradine, in addition to the guideline-based heart failure therapy including beta-blockers, resulted in:
- A significant reduction in heart failure-related hospitalizations and cardiovascular mortality
- An improved quality of life
- An improvement in left ventricular function and a reduction in left ventricular volume .
The combined primary endpoint of the SHIFT study was largely driven by the reduction in hospitalizations .
The current ESC guidelines recommend treatment with ivabradine for HFrEF patients in sinus rhythm with a heart rate of 70 beats/min that remain symptomatic despite therapy with an ACE inhibitor or angiotensin II receptor blocker, a beta-blocker, and a mineralocorticoid receptor antagonist .
Don’t Miss: How Do They Test For Heart Attack
