New York Heart Association Classification May Be An Incomplete Predictor Of Adverse Cardiovascular Outcomes
1. In this secondary analysis of the PARADIGM-HF trial, the association between the New York Heart Association classification and cardiovascular outcomes was ambiguous among 8326 patients.
2. While higher NYHA classification was associated with worse prognosis, NYHA Class I patients with high natriuretic peptides presented higher event rates than patients with low natriuretic peptides from any NYHA class.
Evidence Rating Level: 2
Relevant Reading: Implications of the New York Heart Association classification
New York Heart Association Class
90 In addition, NYHA class improved for all patients, and most patients also demonstrated an improvement in LVEF, end-diastolic volume, and cardiac index, together with a reduction in sphericity index at the 24-month follow-up assessment.
Randolph R. Resnik, Robert J. Resnik, in, 2018
-
NYHA I: Patients that have no limitation of physical activity.
-
NYHA II: Patients with cardiac disease that results in slight limitation to physical activity with symptoms such as fatigue, palpations, dyspnea, or angina pain.
-
NYHA III: Patients with cardiac disease who are comfortable at rest however, less-than-ordinary activity causes fatigue, palpation, dyspnea, or angina pain.
-
NYHA IV: Patients with cardiac disease that results in the inability to carry on any physical activity.
Reinhard Larsen, in, 2010
Relationship Between Pni Combined With Bmi And Nyha Classification
Three logistic regression models were constructed to evaluate the association between PNI, BMI, and NYHA classification . In the multivariate logistic regression analysis, we observed that malnourished-underweight patients and malnourished-overweight patients were significantly associated with poor NYHA classification, and malnourished-underweight patients were more than malnourished-overweight patients . In the further adjusted Model c , the number of malnourished-underweight patients was still higher than that of malnourished-overweight patients .
|
Table 4 Relationship Between PNI Combined BMI and NYHA Classification |
|
Figure 3 Relationship between PNI combined BMI and NYHA classification, **:P< 0.01. |
Recommended Reading: Can Blood Pressure Show Signs Of Heart Attack
Assessment Of Functional Capacity
The ACCF/AHA indicates the 6-minute walk test may be indicated in patients with heart failure whose adequacy of rate control is in question the HFSA indicates it is a good indicator of functional status and prognosis in patients with heart failure.
The ACCF/AHA and HFSA do not recommend routine maximal exercise stress testing. HFSA guidelines indicate it may be useful in situations such as the following with measurement of gas exchange :
- To assess the disparity between symptomatic limitation and objective indicators of disease severity
- To distinguish non HF-related causes of functional limitation, specifically cardiac versus pulmonary
- To consider whether patients are candidates for cardiac transplantation or mechanical circulatory support
- To determine the prescription for cardiac rehabilitation
ACCF/AHA and ESC guidelines note that values of peak oxygen consumption of less than 50% of predicted or less than 14 mL/kg/min reflect poor cardiac performance and a likelihood of 1-year survival less than 50%, facilitating referral for cardiac transplantation or mechanical circulatory device placement.
Cardiac Resynchronization Therapy/biventricular Pacing
The 2013 ACCF/AHA guidelines recommend CRT for patients in sinus rhythm or atrial fibrillation with a QRS duration of 120 ms or longer and an LVEF of 35% or less with persistent, moderate-to-severe heart failure despite optimal medical therapy. A 2012 update of ACC/AHA/HRS guidelines on CRT expanded class I indications to patients with NYHA class II symptoms and LBBB duration of 150 ms or longer. Additional CRT recommendations include :
- Patients with a reduced LVEF and a QRS of 150 ms or longer who have NYHA I or II symptoms
- Patients with a reduced LVEF who require chronic pacing and in whom frequent ventricular pacing is expected
- CRT is not recommended for patients with NYHA class I or II symptoms and non-LBBB pattern with a QRS duration shorter than 150 ms
- CRT is not indicated in patients who are not expected to survive for more than 1 year due to their comorbidities or frailty
The 2022 ACC/AHA/HFSA guidelines indicate an “upgrade” to CRT should be considered for patients with an LVEF of 35% or less who have received a conventional pacemaker or an ICD and who then develop worsening HF despite optimal medical therapy and who have a signficant proportion of RV pacing.
The ESC guidelines gives class I recommendations for the use of CRT in the following groups :
CRT should be considered for the following groups :
CRT may be considered for the following groups :
CRT is contraindicated in patients with a QRS duration below 130 ms.
Also Check: How Do I Know If Im Having A Heart Attack
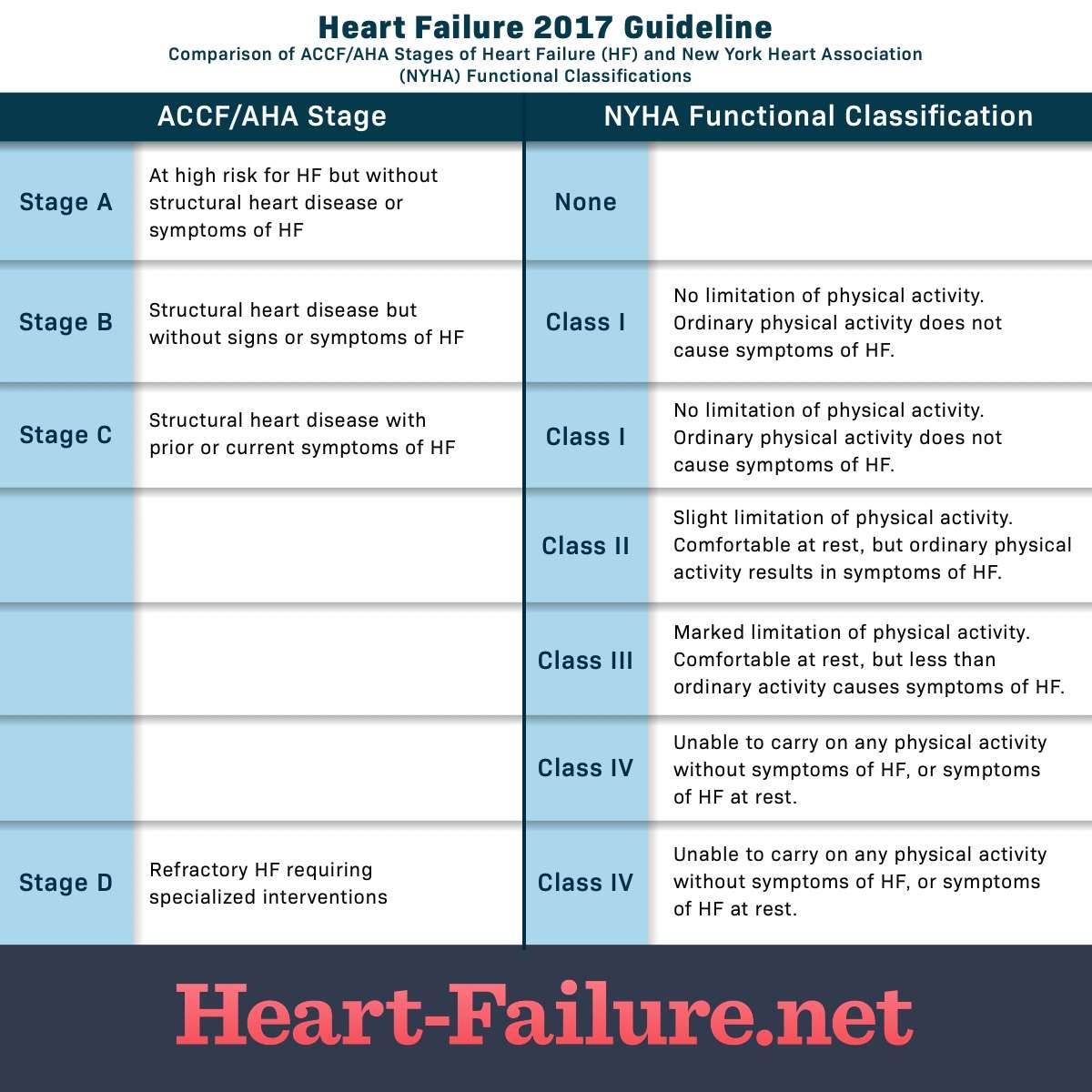
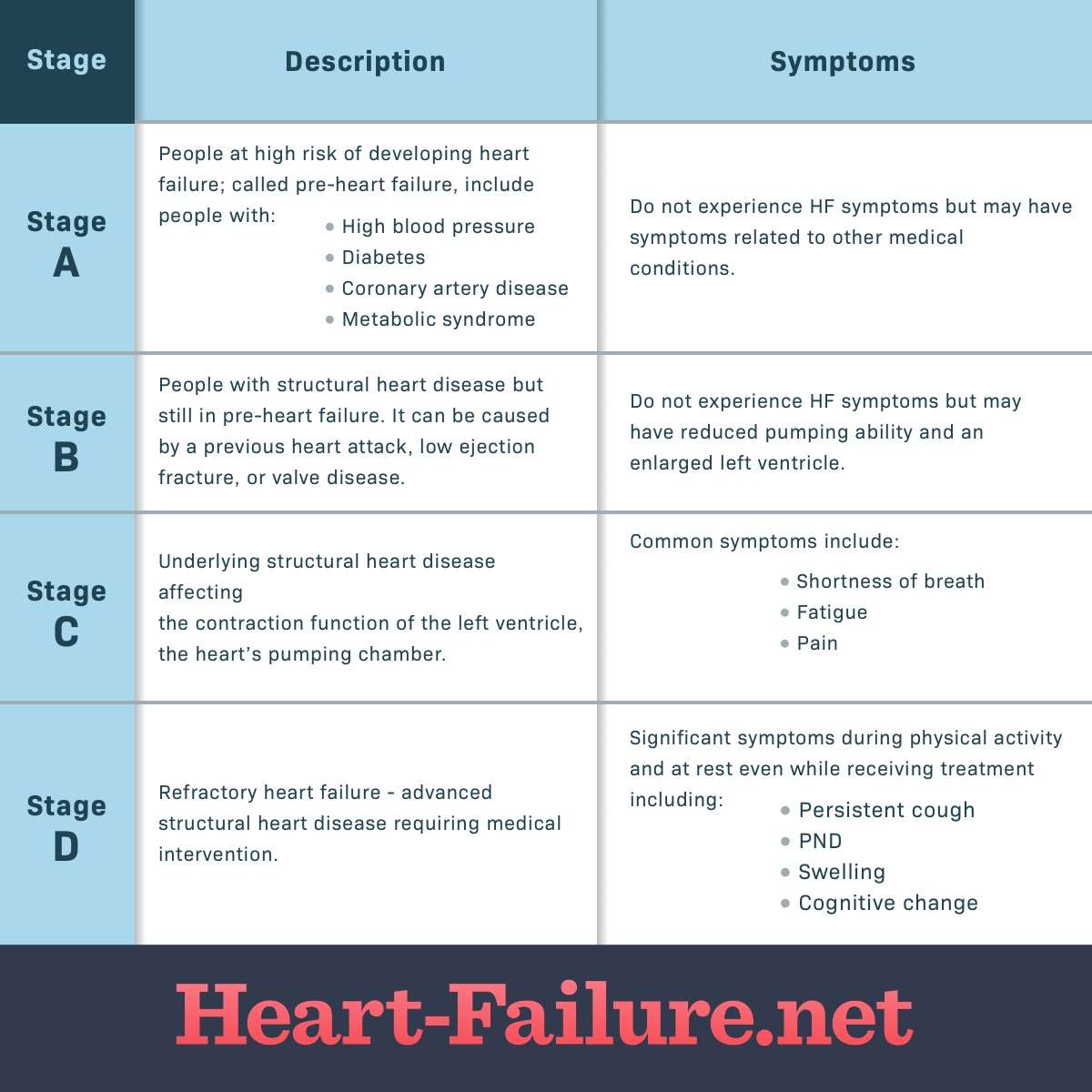
American College Of Cardiology/american Heart Association Classification
The American College of Cardiology/American Heart Association classification of heart failure stages focus more on the condition’s structural impact on the heart, such as the measurement of ejection fraction:
- Stage A: You do not have any structural disorder of the heart, but are at high risk for developing congestive heart failure due to a family history of heart failure or a personal history of hypertension, diabetes, coronary artery disease, alcohol abuse, viral infections, or use of drugs that are toxic to the heart.
- Stage B: You have a structural disorder of the heart, but no symptoms of heart failure .
- Stage C: You have a structural disorder of the heart and you have currently or previously displayed symptoms of heart failure.
- Stage D: People in this final stage of heart failure do not get better with treatment.
American College Of Cardiology/american Heart Association/heart Failure Society Of America Recommendations For Genetic Evaluation And Testing
Genetic screening and counseling are recommended for first-degree relatives of selected individuals with genetic or inherited cardiomyopathies to detect cardiac disease and to encourage review of therapies for lowering HF progression and sudden death.
It is reasonable to refer select patients with nonischemic cardiomyopathy for genetic counseling and testing to identify conditions that could guide treatments for patients and family member.
Read Also: Left Sided Vs Right Sided Heart Failure
Relationship Between Univariate And Nyha Classification
As shown in Table 2, sex, age, SBP, FBG, HbA1c, TC, TG, HDL-C, LDL-C, FIB, D-dimer, LDH, drinking history, current antilipidemic medication, and current antihypertensive medication were all related to NYHA classes II, III, and IV smoking history was related to NYHA classes II and III. Hypertension history was related to NYHA classes II and IV. DBP and diabetes history were related to NYHA class III and IV.
|
Table 2 Relationship Between Univariate and NYHA Classification |
Correlation Between New York Heart Association Functional Class And Mortality
At a median follow-up of 4.7years from index CPET, 99 ACHD patients died. There was a strong relation between NYHA functional class and death, with a 2.5-fold increased mortality risk in class 2 and 8.7-fold in class 3 compared with class 1 and was also true in patients with cyanosis at rest . Furthermore, there was a significant difference in the risk of death between groups 2 and 3 in the overall ACHD population . NYHA class remained a strong predictor of death even when adding age to the model . Indeed, NYHA functional class remained a strong and independent predictor of death, when included in a stepwise multivariate model with age, sex, cyanosis, systemic/sub-pulmonary ventricular function, and Bethesda complexity class . When adding percentage predicted peak VO2, the VE/VCO2 slope and defect complexity to the model with NYHA class, functional class 3 remained a predictor of death with peak VO2 , but not VE/VCO2 slope, functional class 2 or defect complexity. The relation between NYHA class and mortality remained largely unaffected when adjusted for BNP concentration .
KaplanMeier survival curves according to New York Heart Association classification in all adult congenital heart disease and cyanotic patients only .
Recommended Reading: Does Your Heart Rate Go Up When You Eat
European Society Of Cardiology Guidelines For Genetic Counseling And Testing
Arrhythmogenic cardiomyopathy
Offer genetic counseling and testing all patients with suspected ACM and all first-degree adult relatives of patients with ACM and a disease-causing mutation, regardless of their phenotype to preclinically identify genetically affected individuals.
Genetic family screening may also be used for arrhythmic risk stratification.
First-degree relatives with the same definite disease-causing mutation as the patient should undergo clinical evaluation, electrocardiography , echocardiography, and possibly cardiac magnetic resonance imaging . In the setting of no definite identified genetic mutation in the patient or no genetic testing is undertaken, consider clinical evaluation in first-degree adult relatives with ECG and echocardiography, and repeat every 2-5 years or less if nondiagnostic abnormalities are present.
Dilated cardiomyopathy or hypokinetic nondilated cardiomyopathy
All patients with suspected DCM or HNDC and all first-degree adult relatives of such patients and a definite disease-causing mutation, regardless of their phenotype, should undergo genetic counseling and testing to preclinically identify genetically affected individuals. Repeat the evaluation every 5 years or less in first-degree adult relatives when aged younger than 50 years or in the presence of nondiagnostic abnormalities.
All first-degree relatives of patients should undergo clinical evaluation, ECG, echocardiography, and possibly CMRI.
Hypertrophic cardiomyopathy
New York Association Classification Of Heart Failure
Last reviewed 10/2019
New York Heart Association classification is used to grade the severity of functional limitations in a patient with heart failure :
- class I no limitation of physical activity
- ordinary physical activity does not cause fatigue, breathlessness or palpitation
According to a study conducted, the following criteria were used by cardiologists to determine the NYHA class of a patient :
- self reported walking distance – 70%
- difficulty in climbing stairs – 60%
- ability to walk to local landmarks – 30%
- breathlessness interferes with daily activities – 23%
- breathless when walking around the house – 23%
- no specific questions – 13%
This study has also pointed out that NYHA classification system is subjective and poorly reproducible since there are no clear standard criteria for assigning an NYHA class .
Note:
Reference:
Also Check: Signs And Symptoms Of Right Sided Heart Failure
Mechanical Circulatory Support Devices
The following organizations have released guidelines for the utilization of mechanical circulatory support :
- Society for Cardiovascular Angiography and Interventions, American College of Cardiology, Heart Failure Society of America, and Society for Thoracic Surgeons
- International Society of Heart and Lung Transplantation
- American Heart Association
Historically, the intra-aortic balloon bump and extracorporeal membrane oxygenation devices had been the only MCS devices available to clinicians, but axial flow pumps and left atrial to femoral artery bypass pumps have more recently entered clinical practice.
The 2015 SCAI/ACC/HFSA/STS clinical expert consensus-based recommendations include the following :
However, there was insufficient evidence to support or refute routine use of MCS as an adjunct to primary revascularization in the setting of large acute MI to reduce reperfusion injury or infarct size.
In its 2013 guidelines for mechanical circulatory support, the ISHLT recommended long-term MCS for the following patients in acute cardiogenic shock :
Additional recommendations for heart failure therapy include :
The 2012 AHA guidelines on heart device strategies, patient selection, and postoperative care focuses on risk stratification and early referral of high-risk patients with heart failure to centers that can implant MCS. The specific recommendations for MCS include :
What It Means For Heart Failure Patients
It is a common practice to try to classify and compartmentalize conditions in science. If your doctor informs you of your NYHA class, remember that it rarely reflects the bigger picture. If you have class III or IV, it does not necessarily mean you will be there forever, and it certainly does not mean that you have failed as a patient. What is more important is how you feel, and defining objective measures of monitoring with your doctor.
Recommended Reading: Prognosis Of Congestive Heart Failure
Heart Rhythm Society And The European Heart Rhythm Association Select Recommendations For Genetic Testing For Channelopathies And Cardiomyopathies
Long QT syndrome
Comprehensive or LQT1-3 targeted LQTS genetic testing is recommended for the following:
- Individuals with a strong clinical index of suspicion for LQTS based on the patient’s clinical history, family history, and expressed electrocardiographic phenotype
- Asymptomatic individuals with idiopathic QT prolongation on serial 12-lead ECGs defined as QTc over 480 ms or longer than 500 ms may also be considered in asymptomatic individuals with idiopathic QT prolongation on serial 12-lead ECGs for QTc values over 460 ms or longer than 480 ms
Mutation-specific genetic testing is recommended for family members following identification of the LQTS mutation in an index case.
Catecholaminergic polymorphic ventricular tachycardia
- Comprehensive or CPVT1 and CVPT2 targeted CPVT genetic testing is recommended for any individual with a clinical index of suspicion for CPVT based on the patient’s clinical history, family history, and expressed ECG phenotype during provocative stress testing with cycle, treadmill, or catecholamine infusion.
- Mutation-specific genetic testing is recommended for family members following identification of the CPVT mutation in an index case.
Brugada syndrome
Cardiac conduction disease
Short QT syndrome
ACM / arrhythmogenic right ventricular cardiomyopathy
Left ventricular noncompaction
Restrictive cardiomyopathy
Classes Of Heart Failure
Doctors usually classify patients’ heart failure according to the severity of their symptoms. The table below describes the most commonly used classification system, the New York Heart Association Functional Classification1. It places patients in one of four categories based on how much they are limited during physical activity.
| Class | Patient Symptoms |
| I | No limitation of physical activity. Ordinary physical activity does not cause undue fatigue, palpitation, dyspnea . |
| II | Slight limitation of physical activity. Comfortable at rest. Ordinary physical activity results in fatigue, palpitation, dyspnea . |
| III | |
| IV | Unable to carry on any physical activity without discomfort. Symptoms of heart failure at rest. If any physical activity is undertaken, discomfort increases. |
| Class | |
| No objective evidence of cardiovascular disease. No symptoms and no limitation in ordinary physical activity. | |
| B | Objective evidence of minimal cardiovascular disease. Mild symptoms and slight limitation during ordinary activity. Comfortable at rest. |
| C | Objective evidence of moderately severe cardiovascular disease. Marked limitation in activity due to symptoms, even during less-than-ordinary activity. Comfortable only at rest. |
| D | Objective evidence of severe cardiovascular disease. Severe limitations. Experiences symptoms even while at rest. |
For Example:
- A patient with severe anginal syndrome but angiographically normal coronary arteries is classified:
- Functional Capacity IV, Objective Assessment A
Don’t Miss: How Does Advil Cause Heart Attacks
New York Heart Association Functional Classification Of Hf
New York Heart Association functional classification of heart failure based on severity of symptoms and physical activity.
| Class I | No limitation of physical activity. Ordinary physical activity does not cause undue breathlessness, fatigue, or palpitations. |
| Class II | Slight limitation of physical activity. Comfortable at rest, but ordinary physical activity results in undue breathlessness, fatigue, or palpitations. |
| Class III | |
| Class IV | Unable to carry on any physical activity without discomfort. Symptoms at rest can be present. If any physical activity is undertaken, discomfort is increased. |
Register on our website right now to have access to more learning materials!
The Progression Of Heart Failure
Heart failure is a chronic condition that gets worse with time . The stages range from high risk of developing heart failure to advanced heart failure, and provide treatment plans. As the condition gets worse, the heart muscle pumps less blood to the organs, and an individual moves toward the next stage of heart failure. The stages classified by the American Heart Association and American College of Cardiology are different than the New York Heart Association clinical classifications of heart failure that rank patients as class IIIIIIIV, according to the degree of symptoms or functional limits . Treatment at each stage of heart failure may involve changes in medications, lifestyle, and cardiac devices.
NYHA Classification of Heart failure includes the following four classes:
-
Class 1: No limitations in physical activity.
-
Class 2: Mild limitations in physical activity.
-
Class 3: Moderate limitations in physical activity.
-
Class 4: Symptoms occur at rest and any physical activity is not possible without symptoms.
ACC Heart Failure Stages are listed as follows:
-
Stage A: Patients at high risk for heart failure but have no symptoms or structural heart disease.
-
Stage B: Patients have structural heart disease but are asymptomatic.
-
Stage C: Patients have structural heart disease plus symptoms.
-
Stage D: Patients have refractory heart failure that requires modified interventions.
Jennifer Dekerlegand, in, 2007
Read Also: What Is Heart Attack
Cooperative North Scandinavian Enalapril Survival Study
CONSENSUS randomized 253 hospitalized patients with NYHA functional class IV symptoms to either enalapril or placebo in addition to treatment with digoxin, diuretics, and non-ACE vasodilators.37 Based on an interim analysis, enalapril was associated with a highly significant survival benefit compared with placebo , although no difference was reported in the combined risk of death or hospitalization for HF. The CONSENSUS trial was prematurely terminated, because it was deemed unethical to continue a trial in which half of the participants were randomized to placebo.
The Two Sides Of The Heart
The heart is a muscle that is divided into two halves: the left and right side of the heart. Each time the heart beats it transports oxygenated blood out into the circulatory system and refills with blood that needs to be replenished with oxygen by the lungs.8 The left ventricle is the main pumping portion of the heart and plays a key role in normal heart function. HF on the left-side means the heart has to work harder to squeeze out the same amount of blood. This is referred to as left ventricular heart failure. LV, the most common type of HF, is typically diagnosed based on results from an echocardiogram which is used to evaluate the ejection fraction of the left ventricle.8-9
The right ventricle pumps the blood out of the heart into the lungs where it is replenished with oxygen. Right-sided heart failure is usually the result of chronic left-sided failure. As the left ventricle fails, increased fluid flows back through the lungs into the right ventricle, causing blood to back up in the veins leading to swelling and resulting in damage to the right side of the heart.8
Recommended Reading: What Is A Good Heart Rate
