Acute Heart Failure Vs Chronic Heart Failure
Acute heart failure has a sudden onset and symptoms can appear without warning.
In chronic heart failure, that difficulty is ongoing and long-term. More people develop chronic heart failure than acute heart failure, and around 80 percent of acute heart failure cases are people with chronic heart failure whose symptoms rapidly become worse.
Don’t Delay If Heart Failure Symptoms Worsen
A phone call to a nurse or doctor could keep you out of the hospital.
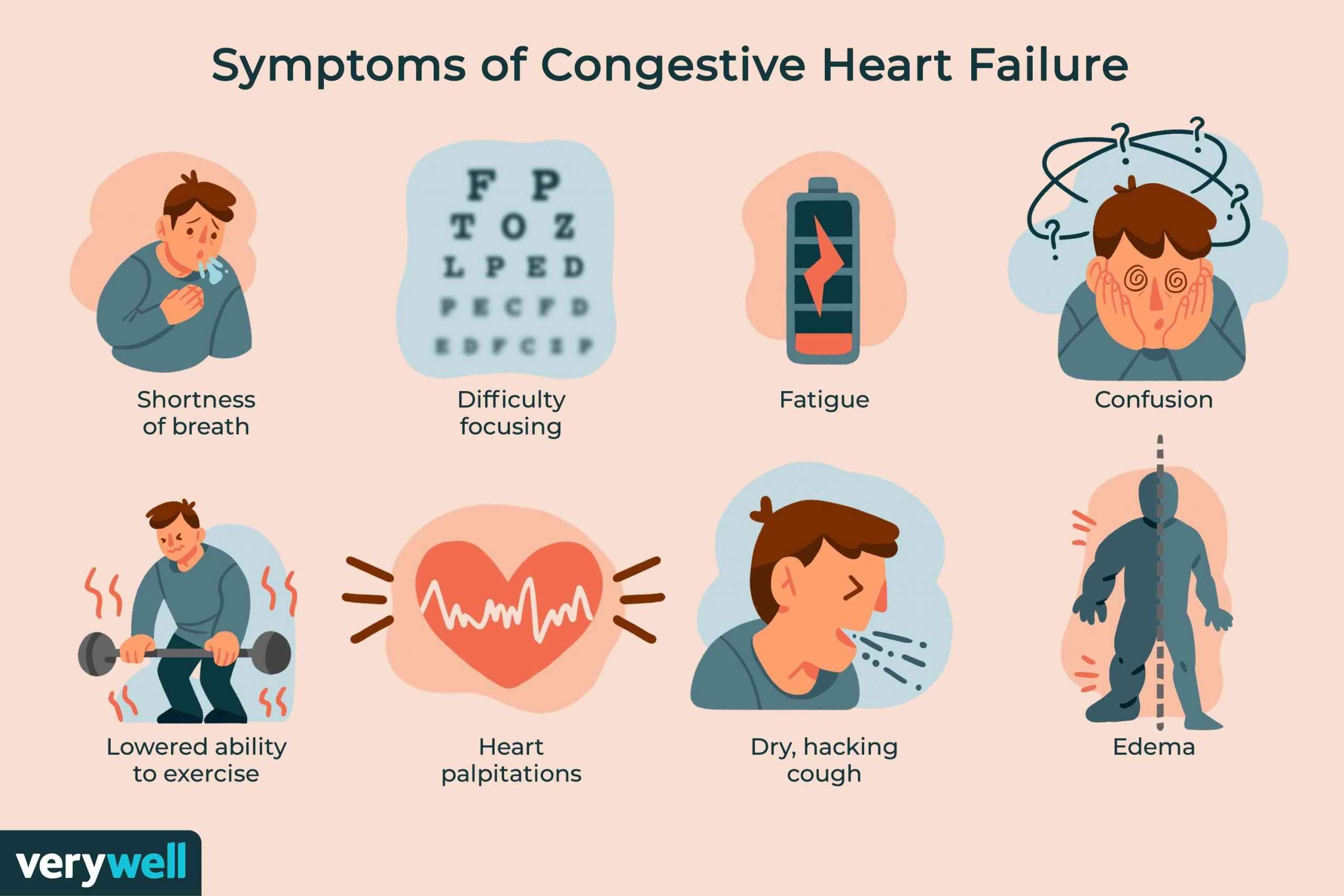
The term “heart failure” conjures up the image of a heart on the verge of beating for the last time. Not so. In this context, failure means that the heart isn’t able to pump enough blood to meet the body’s needs. Common consequences include fatigue, shortness of breath, and swelling in the legs.
To continue reading this article, you must log in.
- Research health conditions
- Prepare for a doctor’s visit or test
- Find the best treatments and procedures for you
- Explore options for better nutrition and exercise
Signs And Symptoms Of Worsening Heart Failure
In this article, youve read about the signs and symptoms of worsening heart failure. The symptoms mentioned in this brief article are progressive as the condition deteriorates.
Heart Failure does not have to equal death and unhappiness. Poor health is often the result of a poor routine. The opposite is also true, so be willing to make adjustments to your lifestyle and embed them in your daily life and you should still be able to enjoy life to the full.
Check out other practical health-related articles on our site that can help put you on track for a long and satisfying life.
- TAGS
Recommended Reading: Is The Heart Attack Grill Still Open
Less Common Symptoms Of Acute Heart Failure
Not everyone will experience the following symptoms of acute heart failure. Some of these symptoms are caused by an underlying condition. Less common symptoms of acute heart failure include:
- Palpitations, the feeling that the heart has skipped or added a beat, where the person has arrhythmia
- Fever, which can be caused by underlying infection
- Fainting, also called syncope
- Blue/colored lips, skin or tongue, also called central cyanosis
Causes Of Heart Failure
Heart failure is often the result of a number of problems affecting the heart at the same time.
Conditions that can lead to heart failure include:
- coronary heart disease where the arteries that supply blood to the heart become clogged up with fatty substances , which may cause angina or a heart attack
- high blood pressure this can put extra strain on the heart, which over time can lead to heart failure
- cardiomyopathy conditions affecting the heart muscle
- heart rhythm problems , such as atrial fibrillation
- damage or other problems with the heart valves
- congenital heart disease birth defects that affect the normal workings of the heart
Sometimes anaemia, drinking too much alcohol, an overactive thyroid or high pressure in the lungs can also lead to heart failure.
Read Also: Flonase Chest Pain
What Is Ejection Fraction
Ejection fraction refers to how well your left ventricle pumps blood with each heart beat. Most times, EF refers to the amount of blood being pumped out of the left ventricle each time it contracts. The left ventricle is the heart’s main pumping chamber.
Your EF is expressed as a percentage. An EF that is below normal can be a sign of heart failure. If you have heart failure and a lower-than-normal EF , your EF helps your doctor know how severe your condition is.
Stages C And D With Preserved Ef
Treatment for patients with Stage C and Stage D heart failure and reserved EF includes:
- Treatments listed in Stages A and B.
- Medications for the treatment of medical conditions that can cause heart failure or make the condition worse, such as atrial fibrillation, high blood pressure, diabetes, obesity, coronary artery disease, chronic lung disease, high cholesterol and kidney disease.
- Diuretic to reduce or relieve symptoms.
YOU ARE THE MOST IMPORTANT PART OF YOUR TREATMENT PLAN!
It is up to you to take steps to improve your heart health. Take your medications as instructed, follow a low-sodium diet, stay active or become physically active, take notice of sudden changes in your weight, live a healthy lifestyle, keep your follow-up appointments, and track your symptoms. Talk to your healthcare team about questions or concerns you have about your medications, lifestyle changes or any other part of your treatment plan.
Read Also: Can Acid Reflux Cause Heart Palpitations
Swelling In The Ankle Region
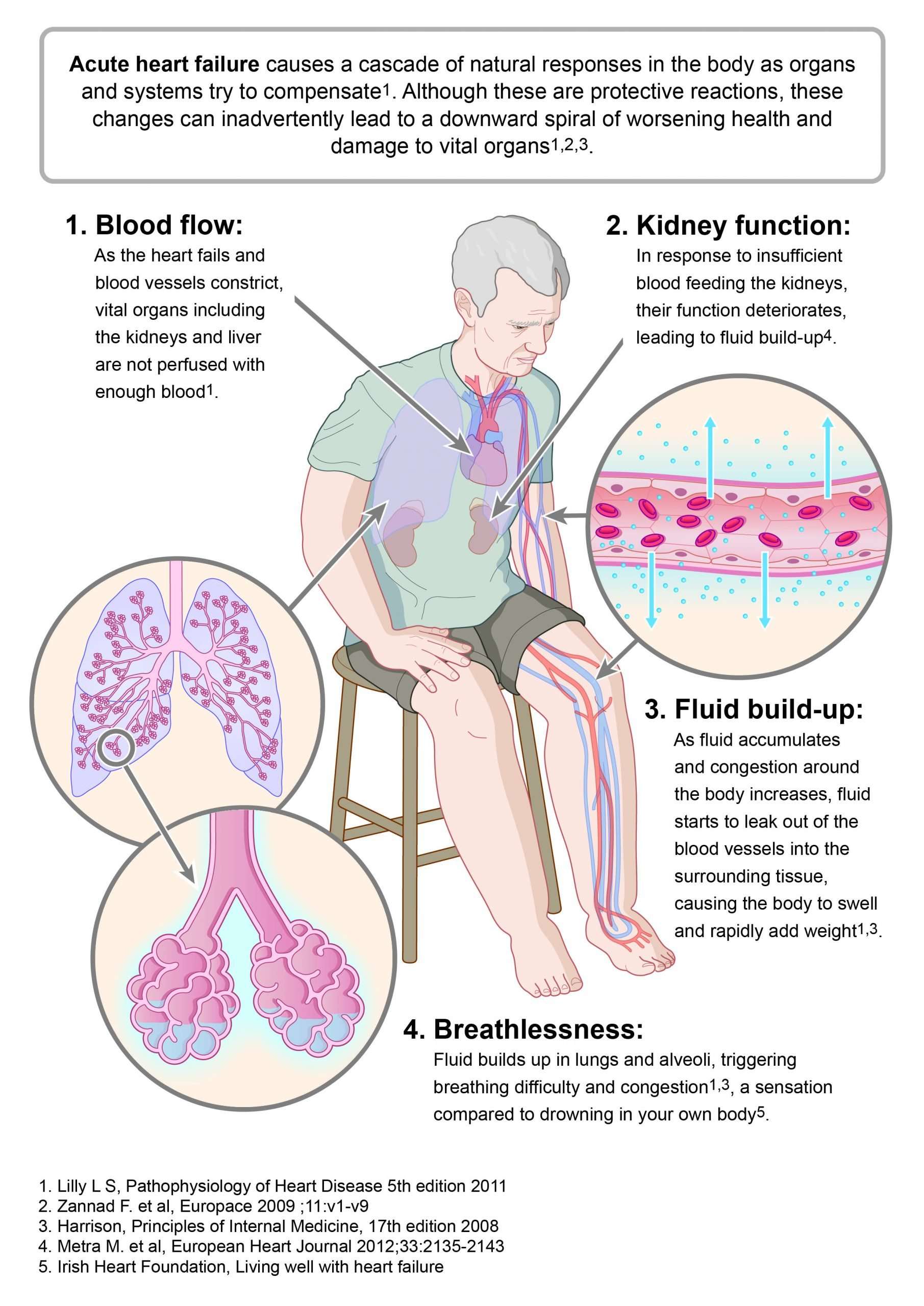
Fluid tends to get accumulated at the dependent region of the body because of heart failure. This is because of the failure of the heart to pump the blood forward, leading to the accumulation of blood in the veins. This leads to distension of veins and due to elevated venous pressure, fluid tends to get accumulated in the intercellular spaces. This leads to pitting oedema at the dependent region of the body, most commonly at the ankle. Increasing oedema is a sign of worsening heart failure.
How Long Can A Chihuahua Live With Heart Failure
How Long Can A Chihuahua Live With Heart Failure?
Is dying of congestive heart failure painful? Pain. Some people with heart failure can experience pain or discomfort towards the end of their life. They should be assessed using a pain scale. Pain-relieving medicines can be used to relieve pain and discomfort this can include opioid and non-opioid medicines .
Can dogs survive congestive heart failure? PROGNOSIS. The development of heart failure represents a specific measurable point in the development of heart disease. For DMVD, the average survival of dogs with CHF is 9 months. However, within survival times in this group vary widely, with some patients living over 3 years.
What are the last stages of congestive heart failure in dogs? A dog with congestive heart failure may cough, have trouble breathing, experience fatigue, loss of appetite, or might die suddenly. Depending on the underlying cause, treatment can help reverse congestive heart failure, and medications are available to help relieve its symptoms.
Also Check: How Long Does End Stage Heart Failure Last
Can You Reverse Chf
Yes, it is achievable to reverse the effects of congestive heart failure. According to a book written by Dean Ornish , MD, the president and founder of the Preventive Medicine Research Institute, a few of the patients reversed the symptoms by making lifestyle changes along with alteration to the diet.
When To Get Medical Advice
See a GP if you experience persistent or gradually worsening symptoms of heart failure.
Call 999 for an ambulance or go to your nearest A& E department as soon as possible if you have sudden or very severe symptoms.
A number of tests can be used to help check how well your heart is working, including blood tests, an ECG and an echocardiogram.
You May Like: Mayo Clinic Heart Rate
Future Directions: Towards An Agreed Definition Of In
The in-hospital WHF definitions used in trials to date have combined several elements: slow response to treatment, failure to respond to treatment, and actual worsening despite treatment. Because of varying trial inclusion criteria, there is a lack of precision in understanding who the patients are, how severe their fluid retention was at inclusion, and how these patients responded to treatment. For example, there may well be a difference between a patient âfailing to respondâ when they start with modest ankle oedema vs. anasarca.
We propose that in-hospital WHF should encompass the notion of failing to respond, as well as clinical worsening and be termed âpoorly responsiveâ HF. The concept of PRHF can be applied to patients meeting the following criteria: evidence of sufficiently severe fluid retention that, in the treating physician’s view, the patient requires i.v. diuretic therapy and the patient is already receiving treatment with reasonable baseline therapy . In patients meeting both these criteria, PRHF can then be defined as either the failure to have a clinically meaningful, or perhaps even specified , net loss of fluid and/or the need for intensification of diuretic therapy, ventilatory support, or mechanical support.
Stage D And Reduced E
Patients with Stage D HF-rEF have advanced symptoms that do not get better with treatment. This is the final stage of heart failure.
Stage D treatment
The usual treatment plan for patients with Stage D heart failure includes:
- Treatments listed in Stages A, B and C.
- Evaluation for more advanced treatment options, including:
- Heart transplant.
- Research therapies.
You May Like: Can Gerd Cause Heart Flutters
Diagnosis Of Acute Heart Failure
Acute heart failure, as well as some of its complications such as pulmonary edema, is a very serious condition. Medical attention should be sought immediately if AHF is suspected.
Diagnosis is based on the symptoms, patient history and physical examination for signs that the heart is failing to pump enough blood.
Diagnostic tests can identify what type of heart failure is involved and which ventricle or side of the heart is involved, as treatments can differ. Tests that may be ordered include:
- Electrocardiogram , which uses electrodes to monitor electrical activity in the heart
- Blood oxygen levels should also be monitored
- Various blood tests can show underlying causes for heart failure or reveal effects of complications
- Chest X-ray, which can be useful to monitor response to treatment
- Echocardiogram , which builds a picture of the heart as it pumps blood and can help identify the type of failure
- MRI or computerised tomography scans can show damage to heart muscle
- Nuclear ventriculography, which uses radioactive materials injected into the bloodstream to form an image of the heart moving
Types of heart failure which may occur in combination can be diagnosed by scanning, and testing the capabilities of the heart include:
How Is Chf Diagnosed
After reporting your symptoms to your doctor, they may refer you to a heart specialist, or cardiologist.
The cardiologist will perform a physical exam, which will involve listening to your heart with a stethoscope to detect abnormal heart rhythms.
To confirm an initial diagnosis, a cardiologist might order certain diagnostic tests to examine your hearts valves, blood vessels, and chambers.
There are a variety of tests used to diagnose heart conditions. Because these tests measure different things, your doctor may recommend a few to get a full picture of your current condition.
Read Also: Does Tylenol Increase Heart Rate
How Does Heart Failure Affect Quality Of Life And Lifestyle
With the right care and treatment plan, heart failure may limit your activities, but many adults still enjoy life. How well you feel depends on how well your heart muscle is working, your symptoms and how well you respond to and follow your treatment plan. This includes caring for yourself and living a healthy lifestyle .
Because heart failure is a chronic long-term illness, talk to your doctor and your family about your preferences for medical care. You can complete an advance directive or living will to let everyone involved in your care know your desires. A living will details the treatments you do or dont want to prolong your life. It is a good idea to prepare a living will while you are well in case you arent able to make these decisions at a later time.
Reviewed by a Cleveland Clinic medical professional.
References
What Are Common Warning Signs Of Heart Failure
- print page
- Bookmark for later
If you have been diagnosed with heart failure , your healthcare team will teach you how to manage your condition. Each person experiences heart failure differently. It is important to know what your specific symptoms are, recognize changes in your condition, and when to call your healthcare provider.1-2 If you experience changes in your condition or the sudden development of any of these warning signs, call your healthcare provider. Dont delay.2
There are general signs of heart failure that are important to know. If you suspect that you may be experiencing heart failure, you should schedule a physical with your primary care provider to assess what may be going on. A good diagnosis is dependent on good symptom reporting. Make note of how you are feeling and when you are experiencing symptoms.
Recommended Reading: Can Acid Reflux Cause Heart Palpitations
Symptoms Of Heart Failure Getting Worse
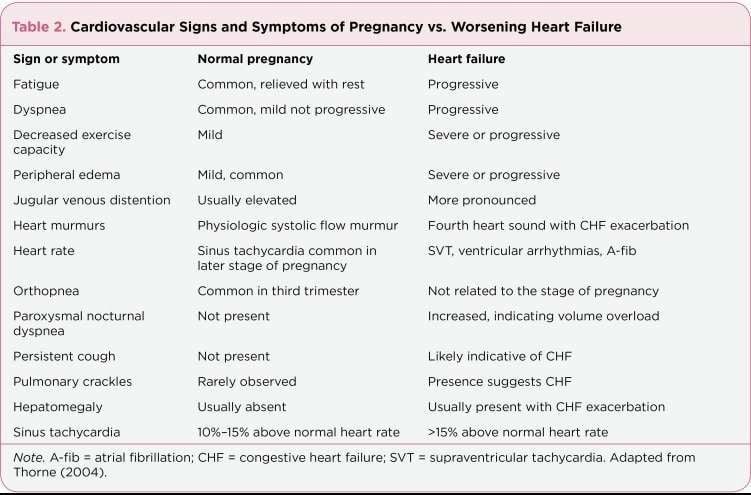
Heart failure may have conditions either as chronic or as acute depending on the stage of the condition or the progression timeline of the heart failure. Sign and symptoms that my observed more so on elderly people suffering from heart failure include
- Shortness of breath when they lie down
- Fatigue and body weaknesses
- Reduced ability to exercise.
- Chest pains and fainting if the heart failure is caused by a heart attack.
However, sources suggest that it is better for the patient to seek a physician for a checkup if they notice severe signs such as fainting or severe weakness, chest pains, irregular or rapid heartbeats that are connected with shortness of breath, and coughing up of pinky, foamy mucus.
Signs Symptoms And Complications
Symptoms of heart failure depend on the type of heart failure you have and how serious it is. If you have mild heart failure, you may not notice any symptoms except during hard physical work. Symptoms can depend on whether you have left-sided or right-sided heart failure. However, you can have symptoms of both types. Symptoms usually get worse as your heart grows weaker.
Heart failure can lead to serious and life-threatening complications.
Don’t Miss: Can Dehydration Cause Increased Heart Rate
Get Support And Know Your Options
Living with heart failure may cause fear, anxiety, depression, and stress. Talk to your healthcare team or a professional counselor. They can help you find or learn ways to cope.
- Get treatment for depression. If you are depressed, your doctor may recommend medicines or other treatments that can improve your quality of life.
- Join a patient support group. You can learn how other people who have similar symptoms have coped with them. Your doctor may be able to help you find local support groups, or you can check with an area medical center.
- Seek support from family and friends. Letting your loved ones know how you feel and what they can do to help can help lower your stress and anxiety.
- Know your treatment options. If your heart failure is very serious, palliative or hospice care can improve your quality of life and help make your daily life more comfortable. This type of care focuses on managing your symptoms, helping you avoid unnecessary tests or treatments, and providing support to your loved ones.
Heart Failuresigns And Symptoms
Heart failure is a condition in which the heart fails to function properly. The terms “heart failure” and “congestive heart failure ” don’t mean that the heart has actually “failed” or stopped but mean one or more chambers of the heart “fail” to keep up with the volume of blood flowing through them.
Heart failure is brought on by a variety of underlying diseases and health problems.
Your condition may involve the left side, the right side or both sides of the heart. Each side has two chambers:
- An atrium or upper chamber
- A ventricle or lower chamber
Any one of these four chambers may not be able to keep up with the volume of blood flowing through it.
Two types of heart dysfunction can lead to heart failure, including:
- Systolic Heart Failure This is the most common cause of heart failure and occurs when the heart is weak and enlarged. The muscle of the left ventricle loses some of its ability to contract or shorten. In turn, it may not have the muscle power to pump the amount of oxygenated and nutrient-filled blood the body needs.
- Diastolic Failure The muscle becomes stiff and loses some of its ability to relax. As a result, the affected chamber has trouble filling with blood during the rest period that occurs between each heartbeat. Often the walls of the heart thicken, and the size of the left chamber may be normal or reduced.
Read Also: Can Flonase Cause Heart Palpitations
Caring For Someone With Heart Failure Towards The End Of Life
Please be aware – this information is for healthcare professionals. We also have information for the public.
You can use our My Learning form to reflect on how this page has helped with your continuing professional development.
Someone with heart failure may experience symptoms such as fatigue, breathlessness, oedema and pain. Towards the end of life, health and social care professionals can support the person by helping to manage their symptoms and talking to them about how they want to be cared for, now and in the future.
On this page:
What You Need To Know About Heart Failure Treatment For The Elderly
Heart failure is a cardiac condition where the heart does not pump blood as efficiently as it should, resulting in a lack of oxygen and nutrients throughout the body. Though it affects people of all ages, heart failure is the leading cause of hospitalizations in people older than 65. Elderly patients who experience heart failure are likely to already have a chronic cardiovascular condition, but it can also be caused by physical decline due to aging and poor cardiovascular management throughout life. Other risk factors include obesity, a family history of heart failure, hypertension and diabetes.
Early signs of heart failure in the elderly are similar to those found in other age groups, which include worsening or shortness of breath, fatigue, bloating, lack of appetite, persistent cough, lack of appetite and nausea. Other symptoms may include a mental decline or depression.
You May Like: Ibs And Palpitations
When Should I Ask For Help
If you feel you need more support to support the patient, speak to their GP, cardiology team or specialist team.
Some parts of the country have specialist heart failure nurses who can be involved in a persons end of life care, so you may want to see if there is one covering your locality. They can visit people at home, in hospital or a hospice and give the person and their family support and guidance.
If the persons heart failure is due to an inherited heart condition such as hypertrophic cardiomyopathy, their family may have concerns about what the future holds for themselves. Give the family an opportunity to voice their worries and, if its appropriate, mention the possibility of referring immediate family members to a clinic which specialises in inherited heart conditions. This may be done when the person was initially diagnosed.
Inherited heart conditions services offer specialist assessment and investigations, genetic counselling and testing. GPs can refer to this service. Additionally signpost your patient to the British Heart Foundation Genetic Information Service , which offers information and support and helps with referrals.
