Diuretics And Mortality In Heart Failure Patients
Diuretic drugs are medications that help the kidneys remove excess fluid from the body, helping to lower blood pressure and decrease edema and fluid overload. They do this by stimulating the kidneys to excrete sodium . Sodium molecules associate with water, so when they’re eliminated by the kidneys, they take water with them. This reduces the amount of excess fluid in the blood and in the body. Heart failure often gives rise to fluid overload, and people with heart failure are commonly treated with diuretic drugs. Recent evidence suggests, however, that long-term, aggressive use of diuretics in patients with heart failure may not be prudent.
As heart failure progresses, a number of symptoms related to fluid overload can appear. Excess fluid can enter the tiny air sacs in the lungs and reduce the amount of oxygen that can enter the blood, causing shortness of breath . Fluid can accumulate in the lungs when a patient lies down at night and make nighttime breathing and sleeping difficult , or even cause the patient to wake up suddenly gasping for air . Fluid overload can also occur in the lower limbs and/or abdomen. One million people are hospitalized each year in the United States for heart failure, 90 percent of them for symptoms related to fluid overload.
Diuretics To Treat Heart Failure
There are different classes of diuretics and each works in a distinct way in the kidneys to remove fluid buildup from the body which reduces pressure on blood vessel walls.2-3 As the kidneys eliminate the excess water from the blood, the total blood volume that the heart has to pump is reduced, which causes blood pressure to go down and makes it easier for the heart to pump forward.4
The different kinds of diuretics include carbonic anhydrase inhibitors, loop diuretics, potassium-sparing diuretics, and thiazide diuretics.3
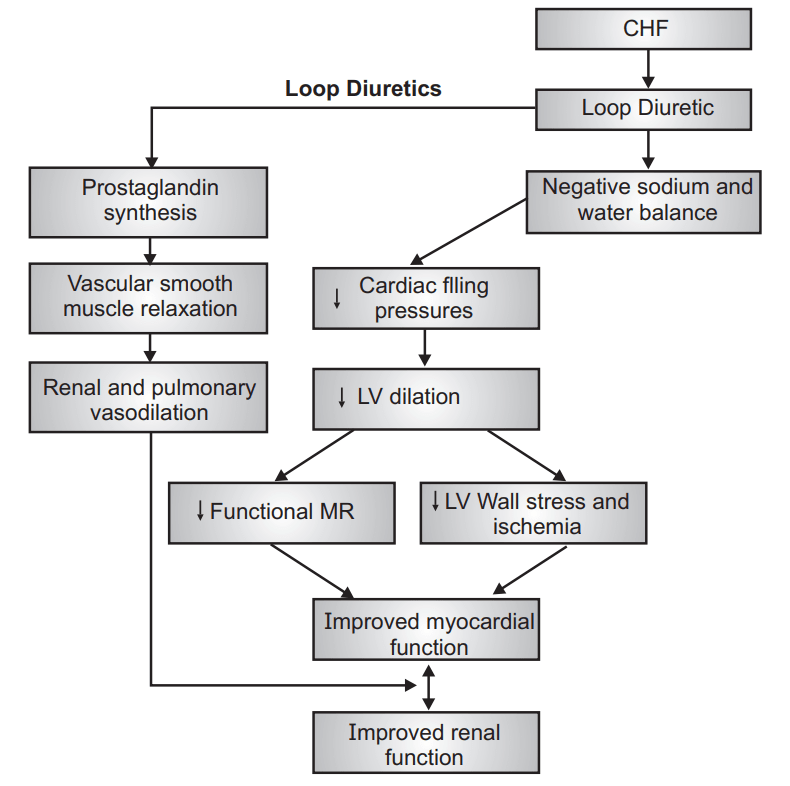
Loop diuretics are the preferred diuretic for use in patients with heart failure. They are also used to treat hypertension and edema due to chronic kidney disease.4 They cause the kidneys to excrete more urine, decreasing the volume of water in the body thus lowering blood pressure.4
Potassium-sparing diuretics, like an aldosterone antagonist, also reduce the amount of water in the body without also losing potassium.4 They are often prescribed with another diuretic to better control blood pressure and to help prevent low potassium levels.4
Carbonic anhydrase inhibitors help remove sodium, potassium, and water from the kidneys. Relatively weak diuretics, they are also are effective at reducing fluid levels in the eyes and are prescribed to treat glaucoma and sometimes used off-label to treat altitude sickness.4
Diuretic Therapy In Hf
Diuretics are a wide group of different drugs used in diverse therapeutic settings. In HF, they are used as first-line therapy to relieve symptoms and signs, and to reduce the episodes of decompensation, thus preventing hospitalization. They induce a rapid improvement of dyspnea and increase exercise tolerance, but evidence on their ability to prevent mortality is still controversial . In the short term, they affect symptoms of fluid congestion, since they reduce the volume overload by increasing urinary flow and water excretion.
As shown in Table 1, most of diuretics act at different sites in the nephron by reducing sodium chloride reabsorption that in turn results in an increase of urinary sodium and water loss. Diuretics work on specific transporters that reabsorb sodium and chloride. With the exception of spironolactone and its analogue, all the transporters specifically inhibited by diuretics are on the luminal face of the tubule. Therefore, to reach their target, diuretics must diffuse or be secreted into the tubular fluid . Among the different groups of drugs, those of interest in HF therapy are loop diuretics , thiazides, potassium-sparing diuretics and carbonic anhydrase inhibitors.
Table 1. Pharmacology of Diuretics
|
2,00% |
FENa = fractional excretion of sodium HCTZ = hydrochlorothiazide MRA = mineralocorticoid receptor antagonists.
Table 2. Common side effect of diuretics
|
Loop diuretics |
|
Azotemia, vaginal bleeding |
Read Also: Whats Congestive Heart Failure
Intravenous Bolus Injection Or Continuous Infusion Of A Loop Diuretic
Impaired absorption of loop diuretics in subjects with CHF results in decreased and delayed peak concentrations in the urine, although the absolute bioavailability does not change significantly when compared with normal subjects. A moderate increase in dose or switching to intravenous administration may obviate this problem.
Venous capacitance increases and pulmonary artery pressure decreases within minutes of a bolus infusion of furosemide in patients with congestive symptoms due to acute myocardial infarction or valvular disease. This finding may explain why patients with pulmonary oedema experience rapid relief of symptoms after administration of intravenous furosemide, even before significant diuresis occurs.
Ototoxicity may occur after rapid intravenous injection of a high dose of a loop diuretic, usually in patients receiving other ototoxic drugs, particularly aminoglycoside antibiotics. Hearing loss and tinnitus are usually transient.
Iv Bolus Injection Or Continuous Infusion Of A Loop Diuretic
As previously discussed, one mechanism of diuretic resistance in CHF patients is impaired absorption of loop diuretics without an absolute change in their bioavailability, compared with normal subjects.40,41 This leads to the delayed and decreased peak concentrations in the urine. This problem may be obviated by moderately increasing the dose or switching the route of drug administration to IV.35 Within minutes after a bolus injection of furosemide in patients having congestive symptoms caused by acute ischemia or valvular heart disease, pulmonary artery pressure decreases and venous capacitance increases.42 This finding may help to explain why the patients with pulmonary edema show quick symptom relief even before achieving significant diuresis after getting IV furosemide.1 The concern with rapid IV injection of a loop diuretic in high doses is the development of ototoxicity, especially in patients simultaneously receiving other ototoxic drugs, such as aminoglycosides.43 Therefore, it is necessary to be cautious while considering a bolus infusion of high-dose furosemide and to avoid this complication, the maximum recommended rate of furosemide infusion is 4 mg/min.43 It is recommended to infuse furosemide slowly when doses are higher than 80 mg to avoid an abrupt increase in peak serum concentration.44
You May Like: Which Of The Following Is Not A Technique Used To Diagnose Heart Disease
Selection Of Drugs For Heart Failure
Choice of drug depends on the type of heart failure along with individual patient characteristics. The most common classification of heart failure currently in use stratifies patients into
-
Heart failure with reduced ejection fraction Heart failure with preserved ejection fraction Heart failure is a syndrome of ventricular dysfunction. Left ventricular failure causes shortness of breath and fatigue, and right ventricular failure causes peripheral and abdominal… read more
-
Heart failure with preserved ejection fraction Heart failure with preserved ejection fraction Heart failure is a syndrome of ventricular dysfunction. Left ventricular failure causes shortness of breath and fatigue, and right ventricular failure causes peripheral and abdominal… read more
-
Heart failure with mildly reduced ejection fraction Heart failure with mildly reduced ejection fraction Heart failure is a syndrome of ventricular dysfunction. Left ventricular failure causes shortness of breath and fatigue, and right ventricular failure causes peripheral and abdominal… read more
Heart failure with reduced ejection fraction
In HFrEF standard of care includes the following four classes of therapies, considered to be ‘foundational therapies’ for HFrEF management:
-
Renin-angiotensin-aldosterone system inhibitor
-
Aldosterone antagonist
Other therapies are used in patient-specific settings .
Heart failure with preserved ejection fraction
Heart failure with mildly reduced ejection fraction
What If No Diuretics Work
What if no diuretics work? This is what I would consider an urgent to an emergency situation. You need to call your doctor immediately or go to an emergency room. Be upfront and honest about what you have been and are taking and responses you have had to each medication. You also want to make sure they check kidney function. It is possible you are having acute kidney failure, which sometimes can be reversed, or have chronic kidney failure, which needs to be addressed right away.
Make sure you are keeping your doctor up to date on how your diuretics are working and make sure to talk about kidney function and alternatives every visit. It doesnt hurt to ask what they think about maybe scaling back to see what happens or maybe even alternating diuretics to help preserve kidney function.
Also Check: What Is An Irregular Heart Rate
Loop Diuretics: Not The Only Ones Thiazide Or Thiazide
There are other classes of diuretics that can be useful in the management of HF, especially in diuretic resistance, a problem that will be dealt with later.
Thiazide diuretics encompass a large class of agents that block the sodium-chloride co-transporter in the distal convoluted tubule , thus exhibiting a synergistic action with the LD, which cause sodium avidity in the distal tubule. The different molecules have a similar blocking effect on NCC, but they differ in terms of half-lives and off-target effect . In contrast with LD, metolazone and chlortalidone have a slow gastrointestinal absorption and a longer half-life, while chlorothiazide has a shorter half-life, differences that should be remembered when co-administered with LD. It is known that the natriuresis induced by these agents is lower compared to LD but the rationale for their use in HF is based on the finding of increased distal nephron sodium avidity in the case of loop diuretic administration . Furthermore, there is evidence that these drugs are effective even in patients with glomerular filtration less than 30 ml/min . However, they should be used with caution, remembering that they are more often associated with hypokalemia and hyponatremia . Therefore, they should be used as a second-line agent in a stepped pharmacologic Algorythm, in case of congestion “resistant” to high doses of LD, as recommended by the Heart Failure Society of America .
Box : Practical Approach To Diuretic Resistance
-
Assess compliance with salt restriction and medicine intake. If necessary, measure the amount of salt and diuretic in the urine.
-
Discontinue NSAIDs.
-
Adjust the dose of the diuretic in patients with renal impairment.
-
Switch to intravenous administration to overcome problems associated with impaired absorption.
-
As it avoids postdiuretic salt retention, a continuous intravenous infusion of a loop diuretic may succeed where other treatments have failed.
-
Combine loop diuretics with other diuretics, preferably a thiazide diuretic.
You May Like: Women’s Heart Attack Warning Signs
Which Is The Best Strategy For Using Diuretics In Decompensated Chronic Heart Failure
Bonasia Vincenzo
Second Unit of Internal Medicine, Department of Internal Medicine, Azienda Sanitaria Universitaria Integrata di Udine, Piazzale Santa Maria della Misericordia, 15, 33100 Udine, Italy
Del Torre Martina
Second Unit of Internal Medicine, Department of Internal Medicine, Azienda Sanitaria Universitaria Integrata di Udine, Piazzale Santa Maria della Misericordia, 15, 33100 Udine, Italy
De Carli Marco
Second Unit of Internal Medicine, Department of Internal Medicine, Azienda Sanitaria Universitaria Integrata di Udine, Piazzale Santa Maria della Misericordia, 15, 33100 Udine, Italy
DOI: 10.15761/FDCCR.1000127
Congestion In Heart Failure
It has been difficult to demonstrate a uniform benefit with respect to any individual therapeutic intervention in patients with AHF . This is probably due to a wide range of pathophysiologies that result in a common phenotypic appearance of pulmonary congestion and peripheral edema . Although pulmonary and systemic congestion may be the most overt findings, these may be the tip of the iceberg reflecting significant congestion of multiple organs, including the kidneys. Many cardiac and extracardiac factors can lead to congestion: left ventricular adverse remodeling, hypertrophy, and stiffness coronary artery disease and microvascular ischemia decreased systemic vascular compliance reduced venous capacitance and excessive preload superimposed right ventricular dysfunction and pulmonary hypertension. Neurohormonal determinants include renin-angiotensin activation, nervous sympathetic overdrive, increased arginine-vasopressin activity, endothelin secretion, and increased immune cell signaling. Clinically, the patient with AHF can be categorized into a two-by-two table according to good or poor systemic perfusion and to the presence or absence of congestion . Those with both poor perfusion and congestion have the worst overall risk for short- and long-term mortality as well as worsened renal function after the initiation of intravenous loop diuretics.
Fig. 1
Recommended Reading: How Painful Is A Heart Attack
Loop Diuretic Use In Acute Decompensated Heart Failure
The limited evidence to guide diuretic use in heart failure is reflected in contemporary practice guidelines, which give diuretics a class I recommendation but based on level B or C evidence.23,24 Furthermore, high diuretic doses, which stimulate the renin-angiotensin-aldosterone and sympathetic nervous systems, have been associated with worse outcomes, raising the possibility that they should be avoided.2527 The Diuretic Optimization Strategies Evaluation study evaluated the optimal approach to diuretic dosing and route of administration for patients with acute decompensated heart failure.28 Using a 2 × 2 factorial double dummy design, DOSE randomized 308 acute decompensated heart failure patients to furosemide, given as twice daily intravenous boluses or continuous infusion, and either low doses or high doses .
Heart Failure With Hfpef
The role of spironolactone in the treatment of heart failure due to ventricular diastolic dysfunction and preserved systolic function is an area of ongoing research.
The association between hyperaldosteronism and development of myocardial fibrosis in human and experimental animal models of hypertension is well established.19 Small studies in humans with HFpEF have shown that MR blockade with spironolactone improved diastolic function.20,21
However, in a recently completed large study in humans with HFpEF, the addition of spironolactone to existing heart failure therapy did not result in a significant survival benefit or reduction in hospitalization for heart failure, although there were substantial geographic differences in patient response.22 The incidence of hospitalization for heart failure was lower in the spironolactone group.
You May Like: Congestive Heart Failure Shortness Of Breath
Other Approaches And Future Directions
Mechanical ultrafiltration is theoretically attractive to remove salt and water, with less stimulation of the renin-angiotensin-aldosterone sytem and a lower risk for rehospitalization70,71. A trial comparing ultrafiltration versus a stepped pharmacologic approach in heart failure and cardiorenal syndrome showed similar fluid removal but more renal dysfunction and adverse events with ultrafiltration.63 A larger trial was stopped early by the study sponsor.72 At present, ultrafiltration in heart failure patients seems indicated primarily as part of comprehensive dialytic treatment of combined heart and kidney failure.
The combination of hypertonic saline with high loop diuretic doses has been proposed to mitigate renal dysfunction and promote natriuresis,75 although this has not yet been tested in a robust trials. Finally, furosemide has been reformulated for subcutaneous delivery, which may allow delivery of IV-like diuresis outside of the hospital setting, with potentially important implications for care delivery and cost. This approach is now being tested in a multi-center randomized controlled trial .
How To Evaluate Diuretic Response
The mostly used parameters to evaluate response to diuretic therapy are usually body weight and daily diuresis. Even though it seems easy to gather them, this does not always correspond to reality. As a matter of fact, daily weight is a measure which must be taken in a precise way in order to be helpful, meaning weighing the patient with the same device, same clothes, etc. moreover, daily weight does not always reflect changes in body fluid volumes and it can be influenced by other factors. Post-discharge changes in body weight only predicted re-hospitalization and were unrelated to mortality in one study , highlighting the limits of examining body weight alone. Other Authors found that diuretic dose did not predict weight loss .
As a result, considerable discrepancy between fluid balance and weight loss is a common issue in patients treated for acute decompensated HF. Awareness of the limits inherent to these commonly used metrics and efforts to develop more reliable measures of diuresis are critical for both patient care and research in acute decompensated HF .
A position statement from the Heart Failure Association of the European Society of Cardiology proposed a flowchart on the use of diuretics in HF and how to evaluate the response to diuretic therapy using these measures that we have summarized in Figure 1 .
Figure 1. Proposed Algorythm on the use of diuretics in heart failure and on the evaluation of response to diuretic therapy
|
Study |
Recommended Reading: Potassium And Heart Rate
Common Side Effects Of Diuretics
Common side effects of diuretics include muscle weakness, fatigue, or low potassium. Most people experience an increased frequency of urination. Medications can take time to work properly and get adjusted. Diuretics tend to work quickly and doses may need to be adjusted frequently. If you find that frequently going to the bathroom interferes with your sleep or certain activities, talk to your doctor about adjusting the medication schedule.1
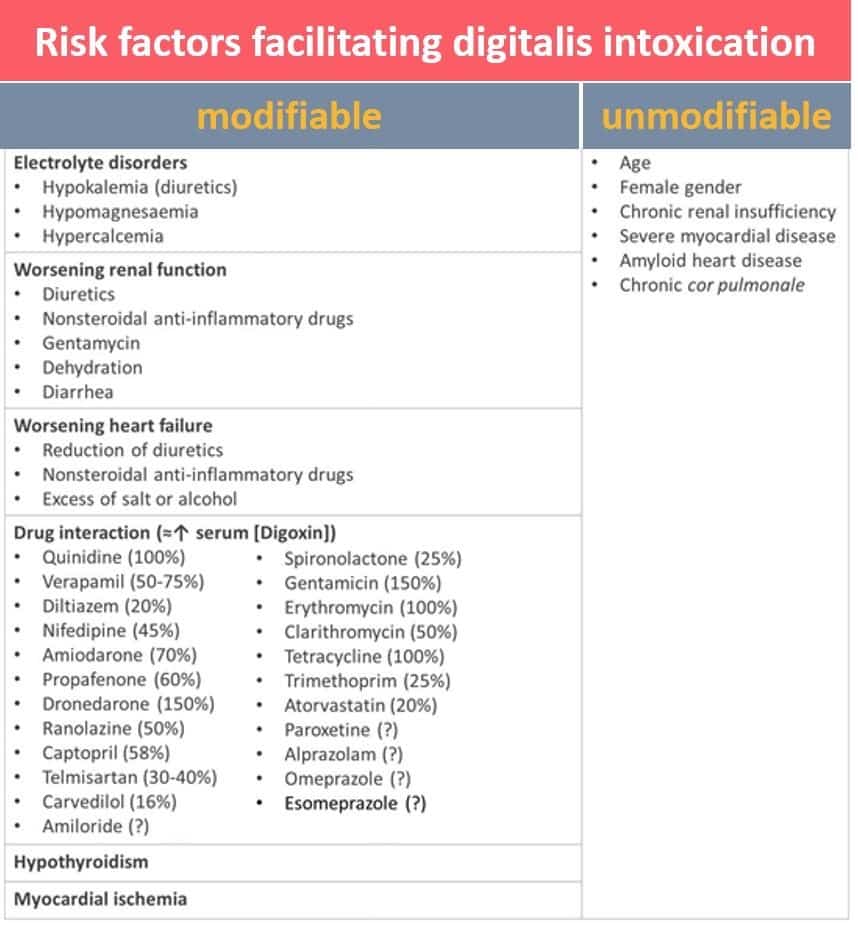
Various diuretics may have drug interactions with other medicines you are taking. Be sure to mention to your doctor all medications, vitamins, minerals, over the counter products, or herbal supplements you take including:4
- Antidepressants, if you take thiazide or loop-acting diuretics
- Cyclosporine, if you take potassium-sparing diuretics
- Digitalis, if you have low potassium levels
- Other high blood pressure drugs
Depending on the diuretic prescribed some people may need to take a potassium supplement or make dietary changes. Your health care provider will decide whether or not you should take potassium.1 As with most heart failure medications, your doctor will generally order regular blood tests to evaluate its effectiveness and any side effects.1
It is important to take all medicines as prescribed. This will improve the effectiveness of the medication and may reduce any complications. If you have difficulty taking medications, do not stop on your own, contact your health care team for assistance.
Diuretic Treatment And Diuretic Resistance In Heart Failure
- Bernhard K KrämerCorrespondenceRequests for reprints should be addressed to Bernhard K. Krämer, MD, Klinik und Poliklinik für Innere Medizin II, Klinikum der Universität Regensburg, Franz-Josef-Strauß-Allee 11, D-93053 Regensburg, GermanyAffiliations
Also Check: Types Of Heart Surgeries
