Dilated Cardiomyopathy And Reduced Ejection Fraction
Hello all,
So I will start by telling you how I came to find out about my heart condition. I am a recovering addict, and my drugs of choice were heroin and cocaine. In 2016, I was hospitalized for an abnormal heart rhythm, and a couple of weeks later I went to see my cardiologist. He told me I had a heart disease called dilated cardiomyopathy and congestive heart failure.
At the time I blew it off and didn’t start taking the meds. Then in 2021, I had an echocardiogram done, and my ejection fraction was at 42%. That is a little low but not a big concern. Then in September 2022, I repeated the echocardiogram. My EF was 25%, and the walls of my heart were pumping very poorly. My doctor put me on lisinopril and metropolol, and now my EF is at 20%.
My biggest question is, is there anyone out there who has a story like mine? What happened to you? What’s going to happen to me? My cardiologist is horrible at answering questions or helping me, so any answers would be very appreciated!
Thank you.
Why Is The Term Ejection Fraction Important
Assessment of EF has been used in drug trials during the last decades when attention was mainly focused on patients with HFrEF. Only recently, have we recognized the frequency of heart failure symptoms due to impaired relaxation of the heart muscle as opposed to reduced contraction . These different categories of patients usually require somewhat different drug treatment. In that most of the research on treatment has been performed on patients with HFrEF, the evidence confirming effective treatment is best for these patients and therefore treatment guideline recommendations are strongest for patients with HFrEF. However, more recently, there is great interest in research into the most effective therapy in patients with HFpEF. Currently, treatment is based on treating the individuals symptoms.
This single and simple measurement of EF by echocardiography is a helpful tool for clinicians designing an individual management plan for patients with heart failure.
What Are The Complications Of Heart Failure
Some of the complications from heart failure include:
- Irregular heartbeat.
- History of taking drugs that can damage your heart muscle, such as some cancer drugs.
Stage B
Stage B is considered pre-heart failure. It means your healthcare provider has given you a diagnosis of systolic left ventricular dysfunction but youve never had symptoms of heart failure. Most people with Stage B heart failure have an echocardiogram that shows an ejection fraction of 40% or less. This category includes people who have heart failure and reduced EF due to any cause.
Stage C
People with Stage C heart failure have a heart failure diagnosis and currently have or previously had signs and symptoms of the condition.
There are many possible symptoms of heart failure. The most common are:
- Shortness of breath.
- Need to urinate while resting at night.
- Rapid or irregular heartbeats .
- A dry, hacking cough.
- A full or hard stomach, loss of appetite or upset stomach .
There may be times that your symptoms are mild or you may not have any symptoms at all. This doesn’t mean you no longer have heart failure. Symptoms of heart failure can range from mild to severe and may come and go.
Unfortunately, heart failure usually gets worse over time. As it worsens, you may have more or different signs or symptoms.Its important to let your doctor know if you have new symptoms or if your symptoms get worse.
Also Check: Digns Of Heart Attack
Pulmonary Hypertension Due To Left Atrial Disease
Reduced left atrial compliance is common in both HFpEF and HFrEF and is manifest by large V waves in the PCWP tracing in the absence of mitral regurgitation. However, isolated or predominant left atrial pathology can occur following left atrial radiofrequency ablation or surgical MAZE procedure performed for atrial arrhythmias. These patients may present with dyspnea on exertion, elevated PAPs, and large V waves on pulmonary capillary wedge pressure tracings that accentuate with volume load.75 While little is known about this entity, as it is associated with extensive left atrial scar formation it is difficult to treat.
What Is The Outlook With Heart Failure
With the right care, congestive heart failure wont stop you from doing the things you enjoy. Your prognosis, or outlook for the future, will depend on:
- How well your heart muscle is working.
- How well you respond to your treatment plan.
- How well you follow your treatment plan.
One study says that people with heart failure have a life span 10 years shorter than those who dont have heart failure. Another study showed that the survival rates of people with chronic heart failure were 80% to 90% for one year, but that dropped to 50% to 60% for year five and down to 30% for 10 years.
A different study found that people who had heart failure and were discharged from the hospital had expected life spans ranging from three to 20 years, depending on various factors like age and gender. Its important to look at your specific situation when considering your prognosis.
Also Check: Open Heart Surgery For Blocked Arteries
Heart Failure With Preserved Left Ventricular Function
With this type of heart failure, you have a preserved, or normal, ejection fraction. It occurs when your left ventricle doesnt relax properly.
This may be due to a thickened heart muscle or heart muscle stiffness. It can lead to less blood being pumped from your heart to the rest of your body.
Symptoms may include fatigue and shortness of breath during exercise. HFpEF can be the result of aging, diabetes, or high blood pressure.
As we age, our hearts do too. Heart walls thicken and lose some of their capacity to contract and relax as efficiently as they should.
But a low ejection fraction reading can also indicate some form of heart damage, including:
- Cardiomyopathy.Cardiomyopathy is a weakening of the heart muscle caused by thickening or dilation of the heart muscle. This makes it harder for your heart to pump properly.
- Heart attack and coronary artery disease. A heart attack occurs when one or more of your arteries become blocked, causing damage to the heart muscle. Coronary artery disease can narrow or block your hearts left and right arteries, making it more difficult for blood to flow to your heart.
- Heart valve disease. This occurs when one or more of the valves in your heart dont open or close properly. This can disrupt the blood flow through your heart and body.
What Is Low Ejection Fraction
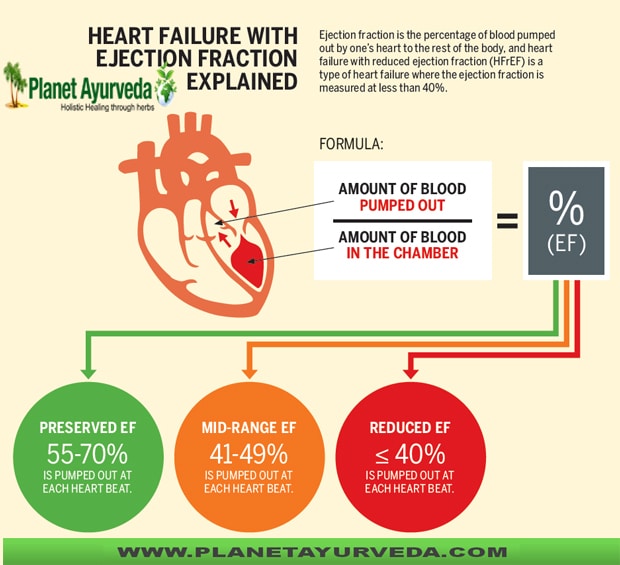
Ejection fraction measures how well your heart is functioning. Its expressed as a percentage and indicates how much blood your heart is pumping out with each contraction.
For example, an ejection fraction of 60% means your heart is pumping 60% of your blood out of your left ventricle every time your heart beats. Generally, a normal range for ejection fraction is between 55% and 70%.
Low ejection fraction, sometimes called low EF, is when your ejection fraction falls below the normal range. It means your heart isnt functioning as well as it should. Your doctor will want to thoroughly check you for a heart condition to find the cause.
A low number can be serious. If your ejection fraction is 35% or below, youre at high risk of developing a dangerous arrythmia or even heart failure.
Recommended Reading: Rapid Heart Rate Anxiety
Titration Schedules And Drug Sequences Examined
shows the conventional sequence of treatments using, in order a RASi, a beta-blocker, an MRA, an ARNI , and an SGLT2i. also shows an accelerated approach to up-titration of the conventional sequence , drug sequencing starting with an ARNI , rather than a RASi, and up-titrating all drugs rapidly, as in Sequence 1a , and the four new treatment sequences found to be most advantageous over the accelerated conventional sequence . In Sequences 25, the order in which the treatments of interest were used was varied from Sequence 1b. The principal scenario reported here assumes that each treatment exerted its full effect from halfway through the up-titration period .
Medication sequences and duration of up-titration periods: Sequences 1, 1a, 1b, 25, and duos 16. The colour boxes indicate different medications, i.e. pink for renin-angiotensin system inhibitor, orange for beta-blocker, green for mineralocorticoid receptor antagonist, red for angiotensin receptorneprilysin inhibitor, and blue for sodiumglucose cotransporter-2 inhibitor. ARNI, angiotensin receptorneprilysin inhibitor BB, beta-blocker MRA, mineralocorticoid receptor antagonist RASi, reninangiotensin system inhibitor SGLT2i, sodiumglucose cotransporter-2 inhibitor.
The results of applying each of the different treatment sequences on the two endpoints of interest are shown in and and the difference in numbers of events and event-free survival after 12 months in .
Ejection Fraction And Heart Failure: What Does It Mean
- Ejection fraction is a measurement used to assess heart failure.
- Heart failure can be present in people who have normal or low ejection fractions.
- In clinical trials, the currently available heart failure treatments have shown benefits only in people with reduced EF.
Heart failure, also known as congestive heart failure or chronic heart failure, occurs when the heart cannot pump blood properly. If you have heart failure, you may have heard your doctor mention ejection fraction a way of measuring how effectively your heart pumps blood. This article will explain what ejection fraction is and why it matters if you have heart failure.
Read Also: Heart Rate Cardio
Low Ejection Fraction Diagnosis
With advanced technology in labs that are among the best-equipped in the country, well use one or more imaging tests to precisely measure your ejection fraction. These tests may include:
- Radiographic imaging, such as a CT scan or MRI
- Echocardiogram, a heart ultrasound
- Nuclear cardiology imaging, which uses a safe dose of radioactive material to evaluate blood flow through your heart
- Cardiac catheterization, a minimally invasive procedure where we gently guide a thin tube, or catheter, with a tiny camera through a blood vessel to your heart
Find out more about our heart and vascular testing and diagnosis.
What Results Can I Expect
Although individual results may vary, the efforts you put into improving your hearts ejection fraction can have additional positive results. You may also discover that you feel better and experience fewer symptoms as well. The investment you are making to help yourself recover is your best pathway for taking control of your health.
Connect with others on our Support Network where people are encouraging each other every day to achieve their best health.
Recommended Reading: How Much Do Beta Blockers Lower Heart Rate
What Causes Heart Failure
Although the risk of heart failure doesnt change as you get older, youre more likely to have heart failure when youre older.
Many medical conditions that damage the heart muscle can cause heart failure. Common conditions include:
- Tobacco and recreational drug use.
- Medications. Some drugs used to fight cancer can lead to heart failure.
Low Heart Ejection Fraction
Hearing your heart ejection fraction is low can generate a lot of questions, like why its low and what can you do to improve it. At Aurora, diagnosing and treating heart conditions is our specialty. With unparalleled expertise, were one of the most active cardiovascular programs in Wisconsin. Our experienced team is here to get you the answers and the right care you need to keep your heart ejection fraction within normal range.
Read Also: Do Heart Attacks Last For Days
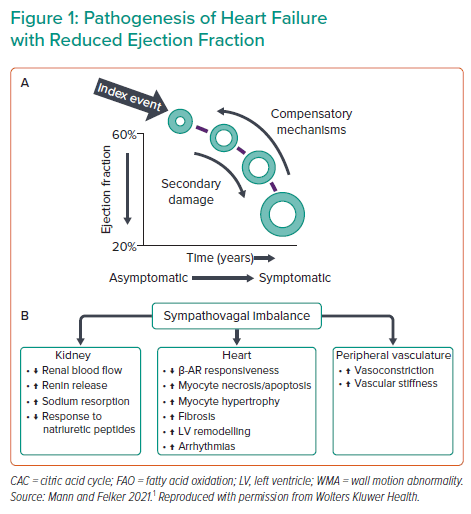
Four Pillars Of Disease
The neurohormonal model of heart failure is key to understanding the efficacy of disease-modifying medical therapy and is summarised in . More recent evidence for the significant benefits related to reducing heart failure admissions associated with SGLT2i expands our understanding of the pathophysiology of heart failure and cements these agents as fundamental keystones in the management of HFrEF.
Beta-blockers indicated in HFrEF
The use of B may worsen acute heart failure and so clinical assessment is required to ensure that the patient with HFrEF is not decompensated at the time of B initiation. Patients may often feel less well for 4872 hours following initiation of B or dose escalation and they should be warned of this to improve compliance with life-saving therapy. Where patients with HFrEF have decompensated on stable doses of B, they should be continued at the same dose, while managing the decompensation. Dose titration should be to the maximum tolerated with a target resting heart rate of 6070 bpm in sinus rhythm. Use of B in patients with HFrEF with AF is recommended, although prognostic benefits are less well proven and aggressive rate control does not appear to provide any significant benefits when compared with more modest rate control. Some patients may not tolerate B at higher doses and where the heart rate remains above 70 bpm then the If channel blocker, Ivabradine, may be used to slow the sinus rate and improve symptoms and mortality.
Clinical Characteristics Of Hfmref
Proper characterization and phenotyping of HFmrEF is important because it might support treatment recommendations based on available data and inform the design of future interventional trials in HFmrEF by facilitating appropriate trial selection criteria. HFmrEF is often defined as intermediate because this classification makes intuitive sense, or as a milder form of HFrEF because of some distinct clinical and treatment response similarities to HFrEF. Both of these approaches are overly simplistic and ignore the extensive emerging research that characterizes HFmrEF in detail in relation to HFrEF and HFpEF. Figure provides a conceptual representation of HFmrEF in relation to HFrEF and HFpEF, and Figs , provide detailed characteristics from specific data sets.
Fig. 1: Phenotype, risk of cause-specific outcomes and effect of therapies in HFrEF, HFmrEF and HFpEF.
Previous research has also assessed the degree of neurohormonal activation across the EF spectrum, showing higher circulating neurohormone levels in patients with HFrEF than in those with HFmrEF or HFpEF,,. The higher neurohormonal activation in HFrEF might reflect the greater HF severity and be a marker of higher rates of cardiovascular events in patients with HFrEF than in patients with HFmrEF or HFpEF, as well as the observed efficacy of neurohormonal inhibition in patients with HFrEF, and potentially in those with HFmrEF, but not in patients with HFpEF ,,.
Don’t Miss: Why Is My Resting Heart Rate Going Up
Monitoring Treatment For All Types Of Heart Failure
Clinical review
1.7.1 All people with chronic heart failure need monitoring. This monitoring should include:
-
a clinical assessment of functional capacity, fluid status, cardiac rhythm , cognitive status and nutritional status
-
a review of medication, including need for changes and possible side effects
-
an assessment of renal function. Note: This is a minimum. People with comorbidities or co-prescribed medications will need further monitoring. Monitoring serum potassium is particularly important if a person is taking digoxin or an MRA.
1.7.2 More detailed monitoring will be needed if the person has significant comorbidity or if their condition has deteriorated since the previous review.
1.7.3 The frequency of monitoring should depend on the clinical status and stability of the person. The monitoring interval should be short if the clinical condition or medication has changed, but is needed at least 6-monthly for stable people with proven heart failure.
1.7.4 People with heart failure who wish to be involved in monitoring of their condition should be provided with sufficient education and support from their healthcare professional to do this, with clear guidelines as to what to do in the event of deterioration.
Measuring NT-proBNP
1.7.5 Consider measuring NT-proBNP as part of a treatment optimisation protocol only in a specialist care setting for people aged under 75 who have heart failure with reduced ejection fraction and an eGFR above 60 ml/min/1.73 m2.
Managing All Types Of Heart Failure
When managing pharmacological treatment, follow the recommendations in the NICE guidelines on medicines adherence and medicines optimisation.
Pharmacological treatment
Diuretics
1.6.1 Diuretics should be routinely used for the relief of congestive symptoms and fluid retention in people with heart failure, and titrated according to need following the initiation of subsequent heart failure therapies.
1.6.2 People who have heart failure with preserved ejection fraction should usually be offered a low to medium dose of loop diuretics . People whose heart failure does not respond to this treatment will need further specialist advice.
Calcium-channel blockers
1.6.3 Avoid verapamil, diltiazem and short-acting dihydropyridine agents in people who have heart failure with reduced ejection fraction.
Amiodarone
1.6.4 Make the decision to prescribe amiodarone in consultation with a specialist.
1.6.5 Review the need to continue the amiodarone prescription at the 6monthly clinical review.
1.6.6 Offer people taking amiodarone liver and thyroid function tests, and a review of side effects, as part of their routine 6monthly clinical review.
Anticoagulants
1.6.7 For people who have heart failure and atrial fibrillation, follow the recommendations on anticoagulation in the NICE guideline on atrial fibrillation. Be aware of the effects of impaired renal and liver function on anticoagulant therapies.
Vaccinations
See NICE’s guidance on smoking and tobacco and alcohol.
Air travel
Driving
Read Also: What Happens To The Resting Heart Rate As A Result Of Regular Endurance Exercise
Treating Heart Failure With Reduced Ejection Fraction In People With Chronic Kidney Disease
1.5.1 For people who have heart failure with reduced ejection fraction and chronic kidney disease with an eGFR of 30 ml/min/1.73 m2 or above:
-
offer the treatment outlined in the section on treating heart failure with reduced ejection fraction and
-
if the person’s eGFR is 45 ml/min/1.73 m2 or below, consider lower doses and/or slower titration of dose of ACE inhibitors or ARBs, MRAs and digoxin.
1.5.2 For people who have heart failure with reduced ejection fraction and chronic kidney disease with an eGFR below 30 ml/min/1.73 m2, the specialist heart failure MDT should consider liaising with a renal physician.
1.5.3 Monitor the response to titration of medicines closely in people who have heart failure with reduced ejection fraction and chronic kidney disease, taking into account the increased risk of hyperkalaemia.
