An Article From The E
Prof. Josep Brugada ,FESC
AF has been associated with an increase in mortality in patients with CHF. The interaction between AF and CHF means that neither of them can be properly managed without treating both. Prospective, randomised trials to determine the benefit of rate versus rhythm control in patients with CHF and AF are urgently needed.
When Should I Call 911
Atrial fibrillation can cause serious medical complications. So, its essential to learn the warning signs and to share them with your family and friends. In many cases, we need someone else to call 911 for us. Immediately call 911 if you have the following symptoms or if you notice them in someone around you:
Signs of bleeding
- Nausea and vomiting.
- Feeling dizzy or lightheaded.
These symptoms can happen within an hour before having a cardiac arrest. In some cases, these symptoms might not appear at all, and a person could simply faint. If you or a loved one have Afib, its a good idea to talk with your healthcare provider about how to get help in medical emergencies. For those who live alone or spend lots of time alone, there may be no one home to call for help. Medical alert devices may be a life-saving resource.
You May Like: What Is Normal Blood Pressure And Heart Rate
Current Therapeutic Options For Heart Failure In Elderly Patients
F. Guerra
1Cardiology and Arrhythmology Clinic, Department of Biomedical Sciences and Public Health, University Hospital Ospedali Riuniti, Marche Polytechnic University, Ancona, Italy
Academic Editor:
Abstract
Heart failure is a major and growing public health problem with high morbidity and mortality . It affects 1-2% of the general population in developed countries, and the average age at diagnosis is 76 years. Because of a better management of acute phase and comorbidities, HF incidence is increasing in elderly patients, with a prevalence rising to 10% among people aged 65 years or older . Therefore, a substantial number of elderly patients need to be treated. However, because of clinical trial exclusion criteria or coexisting comorbidities, currently recommended therapies are widely based on younger population with a much lower mean age. In this review, we will focus on available pharmacological, electrical, and mechanical therapies, underlining pros, cons, and practical considerations of their use in this specific patient population.
1. Drug Therapy
To date, limited evidence has investigated the effects of the recommended systolic HF therapies in aged patients . However, data from small observational studies and substudies suggest that elderly patients derive similar benefits as younger patients .
2. Anemia and Iron Deficiency
3. Implantable Cardioverter-Defibrillator
5. Left Ventricular Assist Device
7. Conclusions
Dont Miss: What Caused Dmx To Have Heart Attack
Also Check: Why Does My Resting Heart Rate Fluctuate
Outlook For Heart Failure
Heart failure is a serious long-term condition that will usually continue to get slowly worse over time.
It can severely limit the activities you’re able to do and is often eventually fatal.
But it’s very difficult to tell how the condition will progress on an individual basis.
It’s very unpredictable. Lots of people remain stable for many years, while in some cases it may get worse quickly.
Implications For Clinicians Policy Makers And Future Research
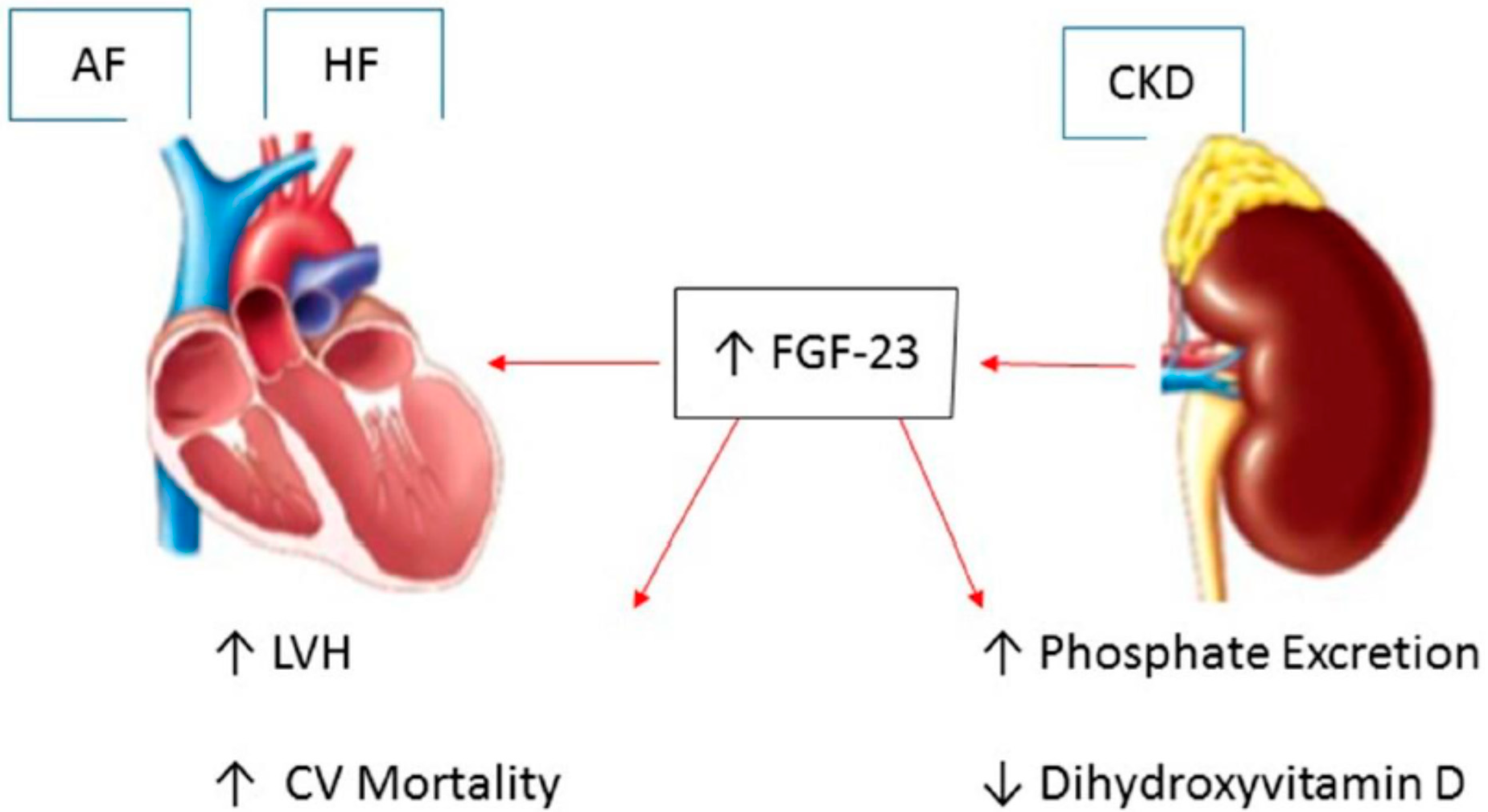
The mechanism by which atrial fibrillation is associated with an increased risk of a range of different cardiovascular diseases is unclear. In the case of myocardial infarction, atrial fibrillation could contribute to demand infarction and the subsequent development of type 2 myocardial infarction.7 It is also possible that the association between atrial fibrillation and non-stroke cardiovascular disease is not causal. Considering our observation that atrial fibrillation is also associated with an increased risk of heart failure, sudden cardiac death, and chronic kidney disease , it seems likely that atrial fibrillation could be acting as a marker for shared underlying risk factors for cardiovascular disease. These include hypertension, which is diagnosed in up to 90% of patients with atrial fibrillation, as well as obesity, diabetes, and obstructive sleep apnoea.125126
Even though the associations we describe cannot indicate causality for the non-stroke outcomes, there is merit in developing clinical risk prediction models for outcomes such as congestive heart failure particularly given our relative and absolute risk estimates. To date, three models have been developed with C statistics ranging from 0.7 to 0.84, but none has been externally validated.127128129 Future models might also benefit from inclusion of non-invasive measures of cardiac function and assessments of novel biomarkers.
What is already known on this topic
What this study adds
You May Like: How To Calculate Max Heart Rate
Focus Issue: Heart Failure Etiology And Outcomesstate
Optimal treatment strategies for patients with HF and AF are unclear.
-
Current rate and rhythm control pharmacotherapies present challenges however, randomized trials of catheter ablation have been promising.
-
Future research should focus on improving long-term outcomes in HF with AF and the effective primary prevention of HF in patients with AF.
Temporal Relations Of Af And Chf
The temporal relations of AF and CHF were examined in a study of 1470 patients with new onset AF or CHF from the Framingham Heart Study . The average follow-up was 5.6 years after the development of AF, and 4.2 years after the development of CHF. Among patients who developed AF, 26% had a prior or concurrent diagnosis of CHF, and 16% of the remaining patients subsequently developed CHF during the follow-up period. Among patients who developed CHF, 24% had a prior or concurrent diagnosis of AF, and 17% developed AF during the subsequent follow-up period. For patients diagnosed with AF, the incidence of developing CHF was 33 per 1000 person-years. Conversely, among individuals diagnosed with CHF, the incidence of developing AF was 54 per 1000 person-years.
The association between AF and the development of CHF was also analyzed in a study of 3288 patients diagnosed with AF at the Mayo Clinic . Twenty-four percent developed CHF during a mean follow-up of 6.1 years, with an incidence of 44 per 1000 patient-years. A spike in the incidence of CHF was seen early after the diagnosis of AF, with 7.8% of cases occurring within the first 12 months, and approximately 3% per year thereafter. Patients with lone AF fared well, as only about 2% developed CHF within 5 years of being diagnosed with AF .
Don’t Miss: What Does Heart Rate Variability Tell You
Afib And Congestive Heart Failure
Considering overall heart health, there are often other heart issues that go along with atrial fibrillation. A common condition those living with AFib often face is congestive heart failure, commonly known as CHF. CHF often refers to a weak heart but can also signify a stiff heart, meaning it doesnt pump blood efficiently throughout the body.
This can lead to back-flow, causing fluid buildup in the lungs or swelling of the legs, which are the most common symptoms of congestive heart failure.
Left Ventricular Systolic Function
-
In patients carefully screened to exclude coronary artery disease and hypertension, there is little change in left ventricular systolic function with increasing age, although cardiac output may decrease in parallel with a reduction in lean body mass.w7 The determinants of cardiac output which may be influenced by age include heart rate, preload and afterload, muscle performance, and neurohormonal regulation.
-
Increases in heart rate in response to exercise or stress caused by non-cardiovascular illnesses, particularly infections, are attenuated with increasing age.w8 Stroke volume increases only by moving up the Frank Starling curve.w9w10 Thus end diastolic volume increases. These age related changes in cardiac response to exercise are mimicked by adrenergic blockade,w11 but adrenergic agonists do not reverse this aging process.w12 The decline in exercise performance with age may additionally relate to peripheral factors, blood flow, and muscle mass rather than being solely the consequence of cardiac performance changes.
Recommended Reading: What Is Your Max Heart Rate
Things That Raise Your Odds Of Heart Failure And Afib
AFib and heart failure are both common on their own. But many people have both, and doctors aren’t totally clear why. One reason may be that many of the same things raise your chances of having both conditions.
Risks you can’t control. Some things you just can’t change, such as:
- Age. The older you are, the greater the chances you’ll get AFib or heart failure. Most people who have both conditions are older adults.
- Genes. There’s still a lot of research to be done here, but certain differences in your genes may affect how likely it is that you end up with heart failure or AFib.
- Gender. Men are more likely to have these conditions than women.
Heart disease. Your odds for heart failure and AFib go up if you have other heart conditions, such as:
- Coronary artery disease, where plaque builds up in your heart’s arteries and leads to less blood flow
- Cardiomyopathy, which is damage to your heart muscle
- Heart valve problems, such as a leaky valve or a valve that doesn’t fully open
- Myocarditis, where the muscles of your heart get swollen and irritated
Other health conditions. Other health issues can also raise your risk, such as:
Smoking and drinking alcohol. Just on its own, smoking raises your odds for all kinds of heart disease, including AFib and heart failure. But it’s even more dangerous if you have risks in play.
Over time, heavy drinking weakens your heart’s muscles. And for some people, alcohol acts as a trigger for AFib.
Show Sources
What You Need To Know About Heart Failure Treatment For The Elderly
Heart failure is a cardiac condition where the heart does not pump blood as efficiently as it should, resulting in a lack of oxygen and nutrients throughout the body. Though it affects people of all ages, heart failure is the leading cause of hospitalizations in people older than 65. Elderly patients who experience heart failure are likely to already have a chronic cardiovascular condition, but it can also be caused by physical decline due to aging and poor cardiovascular management throughout life. Other risk factors include obesity, a family history of heart failure, hypertension and diabetes.
Early signs of heart failure in the elderly are similar to those found in other age groups, which include worsening or shortness of breath, fatigue, bloating, lack of appetite, persistent cough, lack of appetite and nausea. Other symptoms may include a mental decline or depression.
You May Like: Can Heart Failure Get Better
How Does Afib Lead To Heart Failure
Heart failure means the heart isnt pumping enough blood to meet the body’s needs. AFib can lead to heart failure because the heart is beating so fast that it never properly fills up with blood to pump out to the body.
As a result, when the heart doesn’t efficiently pump the blood forward with strong contractions, symptoms develop because:
- Blood can back up” in the pulmonary veins which can cause fluid to back up into the lungs.
- When AFib causes heart failure, fluid in the lungs can cause fatigue and shortness of breath. Oxygen-rich blood is not being delivered to the body and brain, causing physical and mental fatigue and reduced stamina. Fluid also can build up in the feet, ankles, and legs, causing heart-failure related weight gain.
Symptoms Of Heart Failure
The main symptoms of heart failure are:
- breathlessness after activity or at rest
- feeling tired most of the time and finding exercise exhausting
- feeling lightheaded or fainting
- swollen ankles and legs
Some people also experience other symptoms, such as a persistent cough, a fast heart rate and dizziness.
Symptoms can develop quickly or gradually over weeks or months .
Also Check: When Does A Heart Attack Occur
Management Of Concomitant Heart Failure And Reduced Ejection Fraction And Atrial Fibrillation
Currently, clinicians often manage patients with combined HFrEF and AF by focusing on particular therapeutic aspects that have an evidence-base in one or other of these conditions . Researchers have started to investigate if treatment efficacy differs in patients with concomitant disease, but at present these data are limited. In this section, we summarize the evidence-base for common treatment modalities and suggest a simple clinical mnemonic for the initial management of newly diagnosed concomitant HF and AF. The CAN-TREAT HFrEF + AF algorithm distinguishes the management of these patients from those with sinus rhythm. The presence of haemodynamic instability should be treated with urgent cardioversion . Anticoagulation should be instituted to prevent thromboembolism, and diuretic therapy to normalize fluid balance and reduce symptoms of HF. Subsequent therapy should target an initial heart rate < 110 b.p.m. and initiate RAAS antagonism , though with limited data on efficacy . Early rhythm control in patients with symptoms refractory to rate control, and consideration of advanced HF therapies should follow , with aggressive treatment of other concomitant CV disease, particularly ischaemia and hypertension.
CAN-TREAT initial management algorithm for patients with newly identified heart failure and reduced ejection fraction and atrial fibrillation. ACEi, angiotensin converting enzyme inhibitors ARB, angiotensin receptor blockers CV, cardiovascular.
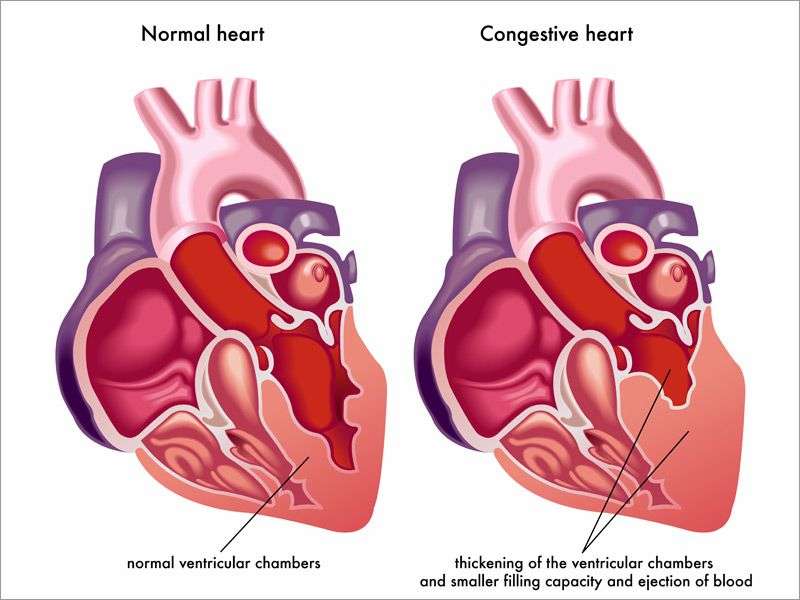
What Is Heart Failure
Heart failure, or congestive heart failure, is a long-term condition that gets worse over time. Although the name sounds like your heart has stopped working, heart failure means your heart isnt able to pump blood as well as it should. When your heart has less pumping power, that can damage your organs and fluid can collect in your lungs.
Also Check: How Long Before Heart Attack Do Symptoms Occur
What Are The Types Of Heart Failure
There are many causes of heart failure, but the condition is generally broken down into these types:
Left-sided heart failure
Heart failure with reduced left ventricular function The lower left chamber of your heart gets bigger and cannot squeeze hard enough to pump the right amount of oxygen-rich blood to the rest of your body.
Heart failure with preserved left ventricular function Your heart contracts and pumps normally, but the bottom chambers of your heart are thicker and stiffer than normal. Because of this, your ventricles can’t relax properly and fill up all the way. Because there’s less blood in your ventricles, your heart pumps out less blood to the rest of your body when it contracts.
Right-sided heart failure
Heart failure can also affect the right side of your heart. Left-sided heart failure is the most common cause of this. Other causes include certain lung problems and issues in other organs.
Mechanisms And Pathophysiology Of Atrial Fibrillation In Heart Failure
Heart failure and AF share risk factors and common pathophysiologic processes . Hypertension, smoking, obesity, diabetes, renal impairment, sleep apnoea, and coronary artery disease are all associated with an increased risk of developing both HF and AF.16 In HF, neurohormonal imbalance and activation of the reninangiotensinaldosterone system leads to maladaptive physiological changes including increased filling pressures and afterload. These can lead to increased left atrial stretch and fibrosis, contributing to the development of conduction abnormalities and facilitating the initiation and maintenance of AF.1721 The reninangiotensinaldosterone system also directly contributes to proarrhythmic remodelling, with angiotensin II causing atrial fibrosis and anisotropic conduction.22 Patients with HF also demonstrate altered calcium handling and calcium overload, which can lead to after-depolarizations and arrhythmia.23
You May Like: Does Eating Raise Heart Rate
Understanding Heart Failure In The Elderly
When a person has heart failure , it means that their heart is unable to pump enough blood throughout their body. Heart failure usually develops over time. As the heart weakens, it either cannot fill with enough blood, pump with enough force or both. While this cardiovascular condition sounds scary, heart failure does not imply that the heart has stopped working or is about to stop working.
Control Of Fast Ventricular Rate
Digitalis glycosides are ineffective in converting AF to sinus rhythm . Digoxin is also ineffective in slowing a rapid ventricular rate in AF if there is associated fever, hyperthyroidism, acute blood loss, hypoxia, or any condition involving increased sympathetic tone . However, digoxin should be used to slow a fast ventricular rate in AF unassociated with increased sympathetic tone, hypertrophic cardiomyopathy, or the Wolff-Parkinson-White syndrome, especially if there is LV systolic dysfunction.
The usual initial dose of digoxin given to undigitalized patients with AF is 0.5 mg orally. Depending on the clinical response, a second oral dose of 0.25 mg may be administered in 6 to 8 hours, and a third oral dose of 0.25 mg may be given in another 6 to 8 hours to slow a rapid ventricular rate. The usual maintenance oral dose of digoxin administered to patients with AF is 0.25 mg to 0.5 mg daily, with the dose decreased to 0.125 mg to 0.25 mg daily for older patients who are more susceptible to digitalis toxicity .
Amiodarone is the most effective drug for slowing a rapid ventricular rate in AF . However, its adverse effect profile limits its use in the treatment of AF. Oral doses of 200 mg to 400 mg of amiodarone daily may be administered to selected patients with symptomatic life-threatening AF refractory to other drugs.
Don’t Miss: Why Does Left Arm Go Numb During Heart Attack
Atrial Fibrillation And Congestive Heart Failure Trial
| The safety and scientific validity of this study is the responsibility of the study sponsor and investigators. Listing a study does not mean it has been evaluated by the U.S. Federal Government. Read our disclaimer for details. |
| First Posted : January 17, 2008Last Update Posted : February 8, 2008 |
| Phase | ||
|---|---|---|
| Atrial FibrillationCongestive Heart Failure | Other: Rate vs rhythm control strategies for atrial fibrillationOther: Rate vs rhythm control strategies in atrial fibrillation | Phase 4 |
Congestive heart failure and atrial fibrillation are two important and growing problems in medicine and cardiology. Both conditions often co-exist and complicate each other’s management. Two therapeutic strategies are available for patients with AF and CHF: the first aims at restoring and maintaining sinus rhythm, whereas, the second focuses exclusively on optimizing ventricular rate. The primary objective of the Atrial Fibrillation and Congestive Heart Failure trial is to compare these two widely-used treatment strategies with respect to cardiovascular mortality.
Hypothesis: Restoring and maintaining sinus rhythm reduces cardiovascular mortality compared to a rate control treatment strategy in patients with AF and CHF.
