Management Of Acute Decompensated Heart Failure
The Heart Failure Society of America guidelines recommend the following treatment goals for patients with acute decompensated heart failure :
- Symptomatic improvement
- Restoration of normal oxygenation
- Identification of the etiology and addressing precipitating factors
- Optimization of long-term oral therapy
- Minimization of side effects
- Identification of patients in whom revascularization or device therapy may be beneficial
- Risk stratification for venous thromboembolism and potential need for anticoagulation
- Patient education regarding medications and self-management of heart failure
- Initiation of a disease management program, where possible
HFSA indications for hospital admission in patients with ADHF are as follows :
- Evidence of severely decompensated heart failure, including hypotension, worsening renal function, and altered mentation
- Dyspnea at rest
- Hemodynamically significant arrhythmia, including new onset of rapid atrial fibrillation
- Acute coronary syndromes
The American College of Cardiology Foundation/American Heart Association comments regarding adjustment of maintenance heart failure medications in patients admitted with ADHF are as follows:
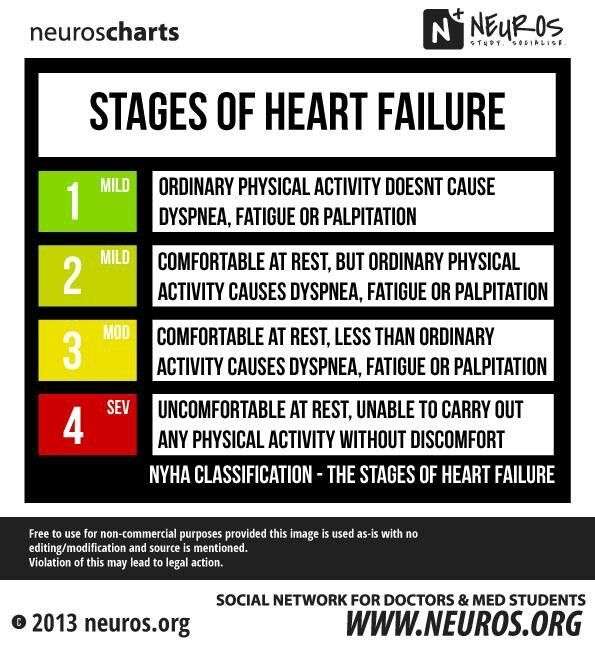
The New York Heart Association Classifies The Stages Of Heart Failure As Follows: 2
No limitation of physical activity. Ordinary physical activity does not cause undue fatigue, palpitation, dyspnea .
Slight limitation of physical activity. Comfortable at rest. Ordinary physical activity results in fatigue, palpitation, dyspnea .
Unable to carry on any physical activity without discomfort. Symptoms of heart failure at rest. If any physical activity is undertaken, discomfort increases.
American College Of Cardiology/american Heart Association/heart Failure Society Of America Recommendations For Genetic Evaluation And Testing
Genetic screening and counseling are recommended for first-degree relatives of selected individuals with genetic or inherited cardiomyopathies to detect cardiac disease and to encourage review of therapies for lowering HF progression and sudden death.
It is reasonable to refer select patients with nonischemic cardiomyopathy for genetic counseling and testing to identify conditions that could guide treatments for patients and family member.
Read Also: What Is Normal Heart Rate Per Minute
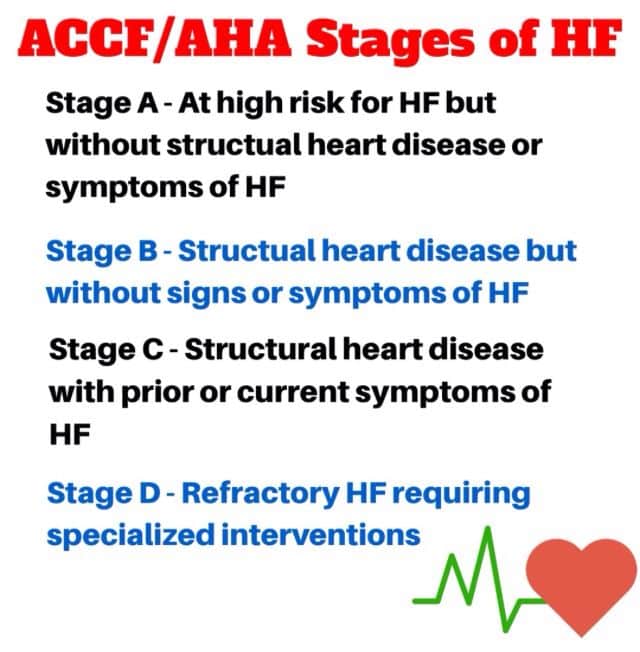
Stages Of Heart Failure
The stages classified by the AHA and ACC are different than the New York Heart Association clinical classifications of heart failure that rank patients as class I-II-III-IV, according to the degree of symptoms or functional limits. Ask your doctor what stage of heart failure you are in.
Stage A
Presence of heart failure risk factors but no heart disease and no symptoms
Stage B
Heart disease is present but there are no symptoms
Stage C
Structural heart disease is present AND symptoms have occurred
Stage D
Presence of advanced heart disease with continued heart failuresymptoms requiring aggressive medical therapy
Document Review And Approval
The full clinical practice guideline was reviewed by 2 official reviewers nominated by the AHA 1 official reviewer nominated by the ACC 2 official reviewers from the Heart Failure Society of America 1 official Joint Committee on Clinical Practice Guidelines reviewer and 32 individual content reviewers. Authors relationships with industry and other entities information is published in Appendix 1 of the full guideline . Reviewers relationships with industry and other entities information is published in Appendix 2 of the full guideline .
You May Like: How Do You Slow Down Your Heart Rate
Acc/aha Heart Failure Classification
The American College of Cardiology/American Heart Association classification of heart failure has four stages. They are listed below.
Stage A: Patients at risk for heart failure who have not yet developed structural heart changes Stage B: Patients with structural heart disease who have not yet developed symptoms of heart failureStage C: Patients who have developed clinical heart failureStage D: Patients with refractory heart failure requiring advanced intervention
Note that the ACC/AHA classification is much different than the New York Heart Association functional classification system, in that there is no moving backwards to prior stages. Once symptoms develop, stage C heart failure is present and stage B will never again be achieved. In the NYHA classification, in contrast, patients can move between class I and class IV relatively quickly, as these are all designated on symptoms alone.
Figure 1 Heart Failure Stages And Classes
The stages above describe the range from a high risk of developing heart failure on through advanced heart failure. The stages are correlated to treatment plans. The stages are also progressive, as HF worsens, you advance to the next stage of heart failure. There is no reversal through the stages. The objective is that with treatment, progression through the stages may be delayed.4
Also Check: Garmin Heart Rate Variability
Heart Failure Symptoms By Class And Stage
- Bookmark for later
Heart failure is a complex, chronic syndrome that gets worse over time. During the diagnostic process, physicians classify each case of heart failure. The American College of Cardiology/American Heart Association and the New York Heart Association have complementary classification systems.1-4
The ACC/AHA stages reflect the range from a high risk of developing heart failure to advanced heart failure and are associated with an approach to treatment plans.1-4 The New York Heart Association clinical classifications of heart failure reflect the severity of symptoms or functional limits due to heart failure.1-2 A diagnosis can have an assignment of a stage and a class.
Universal Definition And Classification Of Heart Failure: A Step In The Right Direction From Failure To Function
- A
Quick Takes
- The proposed universal definition describes HF as a clinical syndrome with symptoms and/or signs caused by a structural and/or functional cardiac abnormality and corroborated by elevated natriuretic peptide levels and/or objective evidence of pulmonary or systemic congestion.
- HF stages have been revised to emphasize symptomatic nature of HF as a clinical syndrome: At risk for HF , PreHF , Symptomatic HF and Advanced HF .
- Classification of HF according to LVEF now includes:
- HFrEF: symptomatic HF with LVEF 40%
- HFmrEF: symptomatic HF with LVEF 41-49%
- HFpEF: symptomatic HF with LVEF 50%
- HFimpEF: symptomatic HF with a baseline LVEF 40%, a 10-point increase from baseline LVEF, and a second measurement of LVEF > 40%
A revised classification of HF by left ventricular ejection fraction was also proposed and is as follows:
Figure 1. Courtesy of Gibson GT, Blumer V, Mentz RJ, Lala A.
Figure 1
The new Universal Definition and Classification of HF represents a landmark advancement in our field. The standardization of the definition of HF is valuable for several reasons:
References
Recommended Reading: What Should Your Heart Rate Be When Walking
Purpose Of The Executive Summary
The purpose of the 2022 AHA/ACC/HFSA Guideline for the Management of Heart Failure is to provide an update and to consolidate the 2013 ACCF/AHA Guideline for the Management of Heart Failure for adults and the 2017 ACC/AHA/HFSA Focused Update of the 2013 ACCF/AHA Guideline for the Management of Heart Failure into a new document. Related ACC/AHA guidelines include recommendations relevant to HF and, in such cases, the HF guideline refers to these documents. For example, the 2019 primary prevention of cardiovascular disease guideline includes recommendations that will be useful in preventing HF, and the 2021 valvular heart disease guideline provides recommendations for mitral valve clipping in mitral regurgitation .
Areas of focus include:
Left ventricular assist device use in stage D HF.
The intended primary target audience consists of clinicians who are involved in the care of patients with HF. The focus of the full clinical practice guideline is to provide the most up-to-date evidence to direct the clinician in patient decision-making. This executive summary provides readers with the Top 10 items that they should know about the 2022 HF guideline and incorporates material from the full guideline along with each statement.
What Is Shared Decision
When heart failure progresses to an advanced stage, there are still many treatment options. The decisions ranging from do everything possible to strive for comfort arent easy. Thats why the American Heart Association released recommendations that serve as a roadmap to decision-making in advanced heart failure.
The goal? A partnership between you and your doctor, where medical options are honestly discussed, and decisions are made based on what you want. Shared decision-making means you dont have to make decisions on your own.
Doctor-patient conversations about treatment options, their risks and benefits as well as future what-if scenarios should happen early and often, according to experts who helped draft the AHA recommendations. This early dialogue means youre not blindsided when a big medical event happens that requires tough decision-making.
Doctors provide the medical facts and figures, while you provide your personal goals and preferences. Together and often with input from family and friends you and your doctor build a care plan.
Also Check: Can Teenagers Get Heart Attacks
Classes Of Heart Failure
Doctors usually classify patients’ heart failure according to the severity of their symptoms. The table below describes the most commonly used classification system, the New York Heart Association Functional Classification1. It places patients in one of four categories based on how much they are limited during physical activity.
| Class | Patient Symptoms |
| I | No limitation of physical activity. Ordinary physical activity does not cause undue fatigue, palpitation, dyspnea . |
| II | Slight limitation of physical activity. Comfortable at rest. Ordinary physical activity results in fatigue, palpitation, dyspnea . |
| III | |
| IV | Unable to carry on any physical activity without discomfort. Symptoms of heart failure at rest. If any physical activity is undertaken, discomfort increases. |
| Class | |
| No objective evidence of cardiovascular disease. No symptoms and no limitation in ordinary physical activity. | |
| B | Objective evidence of minimal cardiovascular disease. Mild symptoms and slight limitation during ordinary activity. Comfortable at rest. |
| C | Objective evidence of moderately severe cardiovascular disease. Marked limitation in activity due to symptoms, even during less-than-ordinary activity. Comfortable only at rest. |
| D | Objective evidence of severe cardiovascular disease. Severe limitations. Experiences symptoms even while at rest. |
For Example:
- A patient with severe anginal syndrome but angiographically normal coronary arteries is classified:
- Functional Capacity IV, Objective Assessment A
New Hf Definition Stage Updates Outlined In 2022 Acc/aha/hfsa Guidelines
The new guidelines also call for better incorporation and addressing of social determinants of health.
During a panel at the American College of Cardiologys 70th Scientific Session, experts highlighted updates to the 2022 American Heart Association /ACC/Heart Failure Society of America guidelines for the management of heart failure and offered a new definition of the condition.
The syndrome of HF is defined as a complex clinical syndrome with symptoms and signs that result from structural or functional impairment, said Biykem Bozkurt, MD, PhD, guideline writing committee vice-chair and professor of Medicine-Cardiology at Baylor College of Medicine.
With regard to terminologies for HF trajectory, the guidelines emphasized the use of persistent HF as opposed to stable HF, as the term stable creates inertia, while persistent HF requires optimization, Bozkurt added. The phrase HF in remission is also preferred over HF in recovery as the majority of patients who withdraw from therapy will relapse.
Among the updates included are a redefinition of HF stages to emphasize prevention and the addition of sodiumglucose co-transporter 2 inhibitors for the treatment of symptomatic HF.
This latter inclusion comes off the heels of an FDA approval for empagliflozin, for a broader range of patients with HF, including those with preserved ejection fraction a condition with a poor prognosis and very limited treatment options.
Recommended Reading: How To Reduce Resting Heart Rate
Heart Failure Society Of America Recommendations For Genetic Evaluation Of Cardiomyopathy
Note the following :
- For all patients with cardiomyopathy, obtain a detailed family history for at least 3 generations
- Carefully assess the patient’s medical history as well as that of asymptomatic first-degree relatives, with special focus on heart failure symptoms, arrhythmias, presyncope, and syncope.
- Screen asymptomatic first-degree relatives for cardiomyopathy
- Screen for cardiomyopathy at intervals in asymptomatic at-risk relatives who are known to carry the disease-causing mutation 00174-0/fulltext#sec18.1″ rel=”nofollow”> HFSA Guideline Approach to Medical Evidence for Genetic Evaluation of Cardiomyopathy )
- Screen for cardiomyopathy in asymptomatic at-risk first-degree relatives who have not undergone genetic testing or in whom a disease-causing mutation has not been identified.
Note: Due to the complexity of genetic evaluation, testing, and counseling of patients with cardiomyopathy, it is recommended that patients be referred to centers with expertise in these matters and in family-based management.
What Do The Classifications Really Mean
Heart failure is staged and classified by healthcare providers but what do they really mean. HF exists along a continuum. It can go from non-existent to mild to moderate to advanced, all over a period of time. Managing heart failure depends on the stage and can include the use of medications, lifestyle behaviors, and cardiac devices.
Mild heart failure may be evident when you experience minimal symptoms, such as shortness of breath, when involved in certain kinds of physical activity or maybe present without any symptoms. With early diagnosis, lifestyle changes, and medication, people with mild to moderate heart failure generally lead normal lives. Moderate heart failure is often classified along with mild HF. The same treatment approach is indicated.
Refractory congestive heart failure occurs when symptoms continue to be present even after routine treatment. This is also called advanced heart failure or end-stage heart failure. It occurs when a person is not responding to or getting worse despite treatment.
Read Also: Why Is Heart Rate Important
Acc/aha Joint Committee Members
Joshua A. Beckman, MD, MS, FAHA, FACC, Chair
Patrick T. OGara, MD, MACC, FAHA, Immediate Past Chair
Sana M. Al-Khatib, MD, MHS, FACC, FAHA
Anastasia L. Armbruster, PharmD, FACC
Kim K. Birtcher, PharmD, MS, AACC
Joaquin E. Cigarroa, MD, FACC
Lisa de las Fuentes, MD, MS, FAHA
Anita Deswal, MD, MPH, FACC, FAHA
Dave L. Dixon, PharmD, FACC
Lee A. Fleisher, MD, FACC, FAHA
Federico Gentile, MD, FACC
Zachary D. Goldberger, MD, FACC, FAHA
Bulent Gorenek, MD, FACC
Adrian F. Hernandez, MD, MHS
Mark A. Hlatky, MD, FACC, FAHA
José A. Joglar, MD, FACC, FAHA
W. Schuyler Jones, MD, FACC
Joseph E. Marine, MD, FACC
Daniel B. Mark, MD, MPH, FACC, FAHA
Debabrata Mukherjee, MD, FACC, FAHA
Latha P. Palaniappan, MD, MS, FACC, FAHA
Tanveer Rab, MD, FACC
Erica S. Spatz, MD, MS, FACC
Jacqueline E. Tamis-Holland, MD, FAHA, FACC
Duminda N. Wijeysundera, MD, PhD
Y. Joseph Woo, MD, FACC, FAHA
Former Joint Committee member current member during the writing effort.
Stages And Classes Defined
Heart failure is generally classified by the severity of a patients symptoms. The most common classification system is the New York Heart Association Functional Classification. There are four levels of clinical classification used to stratify both the presence of symptoms and limitations experienced during physical activity. The severity of symptoms is made by comparison to normal breathing, shortness of breath, and/or angina .1
The symptoms of heart failure associated with function during physical activity are an important indicator of disease progression and prognosis.1-2
- Class I: No limitation of physical activity. Ordinary physical activity does not cause symptoms of HF.
- Class II: Slight limitation of physical activity. Comfortable at rest, but ordinary physical activity results in symptoms of HF.
- Class III: Marked limitation of physical activity. Comfortable at rest, but less than ordinary activity causes symptoms of HF.
- Class IV: Symptoms occur even at rest discomfort with any physical activity. Unable to carry on any physical activity without symptoms of HF.
Class I and II are typically categorized as mild heart failure, while class III and IV are considered more severe or advanced heart failure. A person can move back and forth between these classes based on their symptoms. When a patient has a heart failure exacerbation, they will have more symptoms and likely be a higher class, but when their symptoms are better controlled, they will fall into a lower class.1-4
Also Check: Target Heart Rate When Working Out
Even For Advanced Hf There Are Treatment Options
When heart failure progresses to an advanced stage, difficult decisions must be made. Do I want to receive aggressive treatment? Is quality of life more important than living as long as possible? How do I feel about resuscitation?
For advanced heart failure patients and their doctors, making good decisions requires teamwork. Through shared decision-making, doctors and patients consider both the options and the patients preferences before charting a treatment course.
Heart Rhythm Society And The European Heart Rhythm Association Select Recommendations For Genetic Testing For Channelopathies And Cardiomyopathies
Long QT syndrome
Comprehensive or LQT1-3 targeted LQTS genetic testing is recommended for the following:
- Individuals with a strong clinical index of suspicion for LQTS based on the patient’s clinical history, family history, and expressed electrocardiographic phenotype
- Asymptomatic individuals with idiopathic QT prolongation on serial 12-lead ECGs defined as QTc over 480 ms or longer than 500 ms may also be considered in asymptomatic individuals with idiopathic QT prolongation on serial 12-lead ECGs for QTc values over 460 ms or longer than 480 ms
Mutation-specific genetic testing is recommended for family members following identification of the LQTS mutation in an index case.
Catecholaminergic polymorphic ventricular tachycardia
- Comprehensive or CPVT1 and CVPT2 targeted CPVT genetic testing is recommended for any individual with a clinical index of suspicion for CPVT based on the patient’s clinical history, family history, and expressed ECG phenotype during provocative stress testing with cycle, treadmill, or catecholamine infusion.
- Mutation-specific genetic testing is recommended for family members following identification of the CPVT mutation in an index case.
Brugada syndrome
Cardiac conduction disease
Short QT syndrome
ACM / arrhythmogenic right ventricular cardiomyopathy
Left ventricular noncompaction
Restrictive cardiomyopathy
You May Like: What Is Considered Resting Heart Rate
Acc/aha Heart Failure Staging
- Patients with known heart failure.
- Patients at risk for heart failure.
- Developed jointly by the American College of Cardiology and American Heart Association to complement, but not replace, the more widely-used New York Heart Association functional classification.
- Based on expert consensus.
- Matches stage to treatment options, unlike other classification systems.
- Other heart failure classification systems include Forrester Class and NYHA Class.
- Unlike other classification systems, the ACC/AHA stages include patients at risk for heart failure and corresponding management options.
