Surgery For Systolic Heart Failure
In advanced cases of systolic heart failure, surgery may be a good treatment option. Your doctor will recommend surgery based on your exact symptoms and the cause of your condition. Surgical options include:
- Corrective surgery to fix an underlying problem, such as heart valve repair or replacement or coronary bypass surgery
- Pacemaker to regulate the heartbeat
- Implantable cardioverter defibrillator to monitor the heart for fast rhythm and deliver an electrical shock to reset the heart when necessary
- Left ventricular assist device , which takes over the pumping action of the heart
- Heart transplant to replace the heart with a donated heart from a person who has died
Fluid Overload And Lung Congestion
Fluid overload and lung congestion are unfortunately frequent in people with heart failure and are the most frequent reasons people with heart failure develop symptoms.
With heart failure, the pumping of the heart is less efficient than normal. To compensate for this reduced pumping ability the body attempts to hold on to salt and water. The accumulation of sodium and water can initially improve cardiac function, at least marginallybut eventually, fluid accumulation becomes excessive and leads to several kinds of symptoms. These include:
Medications For Systolic Heart Failure
Depending on the severity of systolic heart failure and its underlying cause, your doctor may prescribe medications. Some of the drug options for treating systolic heart failure include:
- Angiotensin-converting enzyme inhibitors and angiotensin receptor blockers relax the blood vessels to lower blood pressure.
- Beta blockers make the heart beat more slowly and with less force.
- Aldosterone blockers help the body release sodium and water.
- Angiotensin receptorneprilysin inhibitors reduce excess fluid in the body and relax blood vessels, making it easier for your heart to pump blood.
You May Like: How To Stop Hormonal Heart Palpitations
When To See A Doctor
If you notice that you are more tired than usual even with a good night’s sleep or you are having trouble completing your normal activities, you should visit your doctor.
Heart failure can be a slow-moving process, or it can develop as a result of an acute event like a heart attack. You should immediately go to the emergency department or call 911 if you have the following:
- New chest pain, or chest pain that lasts longer than 15 minutes and is not improved with medications or rest
- Severe chest pain, especially if it comes with sweating, nausea, weakness, or shortness of breath
- A heart rate over 120 beats per minute
- Sudden weakness or paralysis
Some Predictors Of Poor Outcome In Chronic Heart Failure
- High NYHA functional class
- Reduced sodium concentration
- Raised plasma catecholamine and natriuretic peptide concentrations
Survival can be prolonged in chronic heart failure that results from systolic dysfunction if angiotensin converting enzyme inhibitors are given. Longitudinal data from the Framingham study and the Mayo Clinic suggest, however, that there is still only a limited improvement in the one year survival rate of patients with newly diagnosed symptomatic chronic heart failure, which remains at 60-70%. In these studies only a minority of patients with congestive heart failure were appropriately treated, with less than 25% of them receiving angiotensin converting enzyme inhibitors, and even among treated patients the dose used was much lower than doses used in the clinical trials.
Also Check: What Should My Heart Rate Be
What Is The Importance Of Ejection Fraction
Your ejection fraction is one way to measure the severity of your condition. If its below normal, it can mean that you have heart failure. Your ejection fraction tells your healthcare provider how good of a job your left or right ventricle is doing at pumping blood. Usually, your EF number is talking about how much blood your left ventricle is pumping out because its your heart’s main pumping chamber.
Several non-invasive tests can measure your EF. With this information, your healthcare provider can decide how to treat you or find out if a treatment is working as it should.
A normal left ventricular ejection fraction is 53% to 70%. An LVEF of 65%, for example, means that 65% of the total amount of blood in your left ventricle is pumped out with each heartbeat. Your EF can go up and down, based on your heart condition and how well your treatment works.
Myocytes And Myocardial Remodeling
In the failing heart, increased myocardial volume is characterized by larger myocytes approaching the end of their life cycle. As more myocytes drop out, an increased load is placed on the remaining myocardium, and this unfavorable environment is transmitted to the progenitor cells responsible for replacing lost myocytes.
Progenitor cells become progressively less effective as the underlying pathologic process worsens and myocardial failure accelerates. These featuresnamely, the increased myocardial volume and mass, along with a net loss of myocytesare the hallmark of myocardial remodeling. This remodeling process leads to early adaptive mechanisms, such as augmentation of stroke volume and decreased wall stress and, later, to maladaptive mechanisms such as increased myocardial oxygen demand, myocardial ischemia, impaired contractility, and arrhythmogenesis.
As heart failure advances, there is a relative decline in the counterregulatory effects of endogenous vasodilators, including nitric oxide , prostaglandins , bradykinin , atrial natriuretic peptide , and B-type natriuretic peptide . This decline occurs simultaneously with the increase in vasoconstrictor substances from the RAAS and the adrenergic system, which fosters further increases in vasoconstriction and thus preload and afterload. This results in cellular proliferation, adverse myocardial remodeling, and antinatriuresis, with total body fluid excess and worsening of heart failure symptoms.
You May Like: What Is The Normal Heart Rate For An Infant
Medications For Heart Failure
Certain medications can help treat heart failure and its underlying cause:
- Aldosterone blockers block the effects of the hormone aldosterone, encouraging the body to release sodium and water. They also help prevent scarring in the heart.
- Angiotensin receptor-neprilysin inhibitor : Treatment with sacubitril-valsartan reduces excess fluid in the body and relaxes blood vessels. This makes it easier for your heart to pump blood. Alternatives to ARNIs include angiotensin-converting enzyme inhibitors andangiotensin receptor blockers .
- Beta blockers make the heart beat more slowly and with less force. They also help keep heart rhythm regular.
- Sodium-glucose transport protein 2 inhibitors are diabetes drugs that have recently been found to be very beneficial in heart failure. They help remove glucose via the kidneys into the urine.
Other medications can relieve the heart failure symptoms:
- Diuretics reduce the amount of fluid in the body.
- Vasodilators dilate the blood vessels and reduce the hearts workload.
- Digoxin helps the heart beat stronger with a more regular rhythm.
- Anti-arrhythmics control arrhythmia and maintain normal heart rhythm.
Nyha Functional Classification System
The New York Heart Association functional classification considers heart failure symptoms that happen during exercise to determine stage. Patients can go back and forth between stages depending on how well-controlled symptoms are on a given day.
- Stage 1: The person has heart disease, but it isnt yet causing symptoms or limiting activities.
- Stage 2: The person has mild symptoms that only slightly limit activity.
- Stage 3: The person has significant limitations to activities. He or she is only comfortable when resting.
- Stage 4: The person has major limitations and experiences symptoms when at rest.
Recommended Reading: Is Heart Valve Replacement Open Heart Surgery
Sensitivity Specificity And Predictive Value Of Symptoms Signs And Chest X Ray Findings For Presence Of Heart Failure In 1306 Patients With Coronary Artery Disease Undergoing Cardiac Catheterisation
| Clinical features |
| 32 |
Oedema
Swelling of ankles and feet is another common presenting feature, although there are numerous non-cardiac causes of this symptom. Right heart failure may manifest as oedema, right hypochondrial pain , abdominal swelling , loss of appetite, and, rarely, malabsorption . An increase in weight may be associated with fluid retention, although cardiac cachexia and weight loss are important markers of disease severity in some patients.
Is It An Emergency
If you or someone in your care has chest pains, difficulty breathing, or severe bleeding, it could be a life-threatening emergency. Call 9-1-1 or the local emergency number immediately.
If you are concerned about a possible poisoning or exposure to a toxic substance, call Poison Control now at 1-800-567-8911.
Thanks to our partners and endorsers:
Recommended Reading: Does Melatonin Slow Your Heart Rate
Systolic And Diastolic Failure
Systolic and diastolic heart failure each result in a decrease in stroke volume. This leads to activation of peripheral and central baroreflexes and chemoreflexes that are capable of eliciting marked increases in sympathetic nerve traffic.
Although there are commonalities in the neurohormonal responses to decreased stroke volume, the neurohormone-mediated events that follow have been most clearly elucidated for individuals with systolic heart failure. The ensuing elevation in plasma norepinephrine directly correlates with the degree of cardiac dysfunction and has significant prognostic implications. Norepinephrine, while directly toxic to cardiac myocytes, is also responsible for a variety of signal-transduction abnormalities, such as downregulation of beta1-adrenergic receptors, uncoupling of beta2-adrenergic receptors, and increased activity of inhibitory G-protein. Changes in beta1-adrenergic receptors result in overexpression and promote myocardial hypertrophy.
Common Causes Of Lower Limb Oedema
- Gravitational disorderfor example, immobility
- Congestive heart failure
- Venous thrombosis or obstruction, varicose veins
- Hypoproteinaemiafor example, nephrotic syndrome, liver disease
- Lymphatic obstruction
Fatigue and lethargy
Fatigue and lethargy in chronic heart failure are, in part, related to abnormalities in skeletal muscle, with premature muscle lactate release, impaired muscle blood flow, deficient endothelial function, and abnormalities in skeletal muscle structure and function. Reduced cerebral blood flow, when accompanied by abnormal sleep patterns, may occasionally lead to somnolence and confusion in severe chronic heart failure.
Also Check: Reversing Congestive Heart Failure
History And Physical Exam
A clinician listens to your heart and lungs and measures your blood pressure and weight. They will also ask about your:
- Familys medical history, especially previous cardiac problems
- Medications, including prescriptions, over-the-counter drugs and supplements
- Personal medical history
Blood tests can measure several things related to heart failure:
- Sodium and potassium levels
- Creatinine, which helps measure how well your kidneys are working
- B-type natriuretic peptide , a hormone released from the ventricles in response to increased wall tension that occurs with heart failure
Atrial Natriuretic Peptide And B
ANP and BNP are endogenously generated peptides activated in response to atrial and ventricular volume/pressure expansion. ANP and BNP are released from the atria and ventricles, respectively, and both promote vasodilation and natriuresis. Their hemodynamic effects are mediated by decreases in ventricular filling pressures, owing to reductions in cardiac preload and afterload. BNP, in particular, produces selective afferent arteriolar vasodilation and inhibits sodium reabsorption in the proximal convoluted tubule. It also inhibits renin and aldosterone release and, therefore, adrenergic activation. ANP and BNP are elevated in chronic heart failure. BNP especially has potentially important diagnostic, therapeutic, and prognostic implications.
For more information, see the Medscape Drugs & Diseases article Natriuretic Peptides in Congestive Heart Failure.
You May Like: What Is The Normal Resting Heart Rate For A Woman
Nurse Teaching On Complications Of Congestive Heart Failure
Effectively contracting and optimally functioning heart muscle is needed to pump blood from one chamber in the heart to the next in orderly fashion, pump blood into the lungs for oxygen pick-up, and pump oxygen rich blood to the vital organs and tissues in the body. Congestive heart failure is an abnormal condition of the heart, in which the heart muscle is damaged. The signs and symptoms could slightly vary depending on the severity of damage and the chambers affected. Overall, damaged heart muscle cannot contract effectively, contributing to poor contractions and inadequate pumping activity of the involved heart chambers. This post discussed complications of congestive heart failure if this situation is not controlled and the damage continues further.
In summary, complications of congestive heart failure can be listed as below
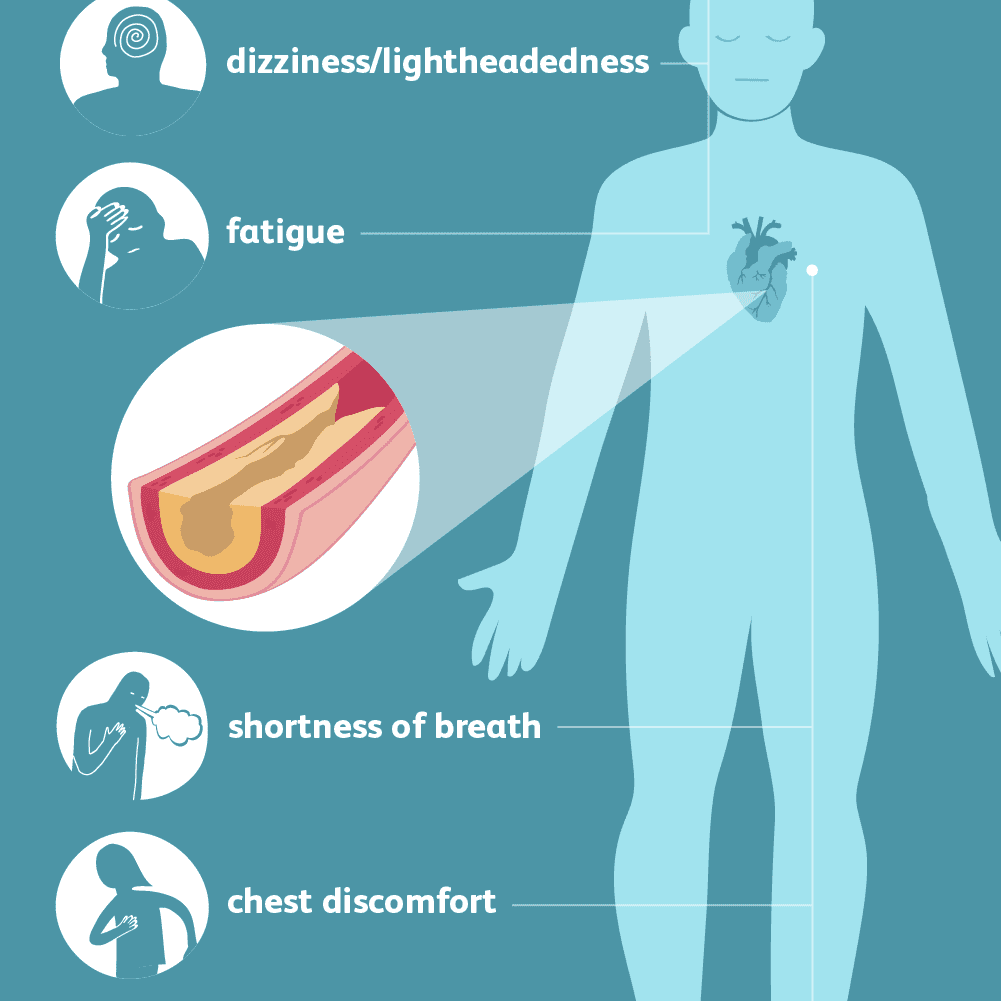
Hypotension:
Reduced output of blood from the heart due to congestive heart failure, can result in low blood volume in circulation, low blood pressure, and hypotensive symptoms of dizziness and lightheadedness. Also, reduced blood supply to brain, secondary to hypotension and reduced output from heart, can contribute to altered level of consciousness. Eventually, this increase risk for falls and accidents.
Compromised end organ function:
Exacerbation of SOB:
Chest pain and discomfort:
Worsening of heart failure:
Increased weakness and fatigue:
Arrhythmia:
Blood clot formation:
Acute weight gain:
Complications Of Heart Failure
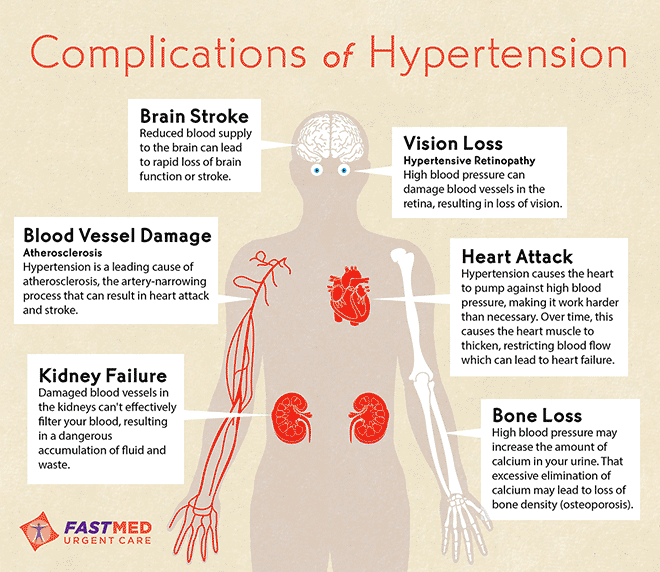
When the heart is damaged or weak and has to work too hard it can lead to symptoms and a decreased quality of life. Lifestyle factors including smoking, obesity, a high-fat diet, and physical inactivity can also make heart failure worse.3
Complications can be life-threatening so it is important to identify them early.4 Common complications include:
- Cardiac arrhythmias- Heart rhythm problems from either the top chambers or bottom chambers can cause worsening of heart failure and other complications. Atrial fibrillation can cause palpitations, fainting, and lead to strokes. Ventricular tachycardia or ventricular fibrillation can cause palpitations, fainting or even sudden death.4,5 An irregular or fast heartbeat can negatively affect the hearts ability to pump sufficient blood to nourish the body.3
- Anemia- Develops when there is a decrease in the oxygen-carrying hemoglobin in red blood cells. It can cause weakness and fatigue and result in a faster heart rate.4
- Stroke- If the brain is deprived of oxygen when blood volume is low or cut off you can experience a stroke. This can result in a loss of motor function, ability to communicate ability and even death.4
- Heart valve problems- If there are mechanical issues with your heart valves it can affect the heart’s pumping ability. It can trigger arrhythmias, make HF worse, and may require surgery to repair.4,5
Also Check: Congestive Heart Failure Risk Factors
What Causes Heart Failure
Although the risk of heart failure doesnt change as you get older, youre more likely to have heart failure when youre older.
Many medical conditions that damage the heart muscle can cause heart failure. Common conditions include:
- Tobacco and recreational drug use.
- Medications. Some drugs used to fight cancer can lead to heart failure.
How Is Congestive Heart Failure Diagnosed
Patients will typically have an intake visit with a heart specialist and nurse or physicians assistant. During this visit, the doctor will review the patients prior records and his or her current health status. This allows the doctor to establish a picture of where the patient is along the spectrum, and make a plan for prognosis and treatment.
The process often takes more than one meeting and involves both the patients local cardiologist or referring physician.
Recommended Reading: How Low Should Your Heart Rate Be
Treatment For Systolic Heart Failure
If you have systolic heart failure, your doctor will offer treatments to address the underlying causes, relieve your symptoms and improve your overall health. Treatment often involves a combination of therapies that may include:
- Lifestyle changes
- Recognize small warning signs in your body, such as swelling or weight gain.
Can Heart Failure Be Prevented
You may be able to prevent or delay heart failure if you:
- Work with your provider to manage any health conditions that increase your risk of developing heart failure
- Make healthy changes in your eating, exercise, and other daily habits to help prevent heart disease
NIH: National Heart, Lung, and Blood Institute
Also Check: What Happens When Your Heart Rate Is Too High
What Are The Complications Of Heart Failure
Some of the complications from heart failure include:
- Irregular heartbeat.
- History of taking drugs that can damage your heart muscle, such as some cancer drugs.
Stage B
Stage B is considered pre-heart failure. It means your healthcare provider has given you a diagnosis of systolic left ventricular dysfunction but youve never had symptoms of heart failure. Most people with Stage B heart failure have an echocardiogram that shows an ejection fraction of 40% or less. This category includes people who have heart failure and reduced EF due to any cause.
Stage C
People with Stage C heart failure have a heart failure diagnosis and currently have or previously had signs and symptoms of the condition.
There are many possible symptoms of heart failure. The most common are:
- Shortness of breath.
- Need to urinate while resting at night.
- Rapid or irregular heartbeats .
- A dry, hacking cough.
- A full or hard stomach, loss of appetite or upset stomach .
There may be times that your symptoms are mild or you may not have any symptoms at all. This doesn’t mean you no longer have heart failure. Symptoms of heart failure can range from mild to severe and may come and go.
Unfortunately, heart failure usually gets worse over time. As it worsens, you may have more or different signs or symptoms.Its important to let your doctor know if you have new symptoms or if your symptoms get worse.
Symptoms Of Reduced Pumping Capability
The most prominent symptoms are:
- Extreme weakness and fatigue
- Muscle weakness and muscle wasting
- Lethargy and inanition
- Extreme weight loss
Obviously, symptoms like this are not compatible with a long life. Unless the cardiac function can be improved, or unless cardiac transplantation or a ventricular assist device can be used, once a person with heart failure develops these kinds of symptoms, death usually follows relatively soon.
You May Like: What Is The Standard Heart Rate
What Are The Symptoms Of Heart Failure
The symptoms of heart failure depend on which side of your heart is affected and how serious your condition has become. Most symptoms are caused by reduced blood flow to your organs and fluid buildup in your body.
Fluid buildup happens because the flow of blood through your heart is too slow. As a result, blood backs up in the vessels that return the blood to your heart. Fluid may leak from the blood vessels and collect in the tissues of your body, causing swelling and other problems.
Symptoms of heart failure may include:
- Feeling short of breath when you do things like climbing stairs. This may be one of the first symptoms you notice.
- Fatigue or weakness even after rest.
