Sympathetic Adrenergic Nerves Innervate The Sa And Av Nodes Conduction Pathways And Myocytes In The Heart These Adrenergic Nerves Release The Neurotransmitter Norepinephrine Which Binds To Specific Receptors In The Target Tissue To Produce Their Physiological Responses Neurotransmitter Binding To Receptors Activates Signal Transduction Pathways That Cause The Observed Changes In Cardiac Function
Adrenergic receptors are receptors that bind adrenergic agonists such as the sympathetic neurotransmitter NE and the circulating hormone epinephrine . The most important adrenoceptor in the heart is the 1-adrenoceptor. When activated by a 1-agonist such as NE or EPI, heart rate is increased , conduction velocity is increased , contractility is increased , and the rate of myocyte relaxation is increased .
There are also 2-adrenoceptors in the heart and stimulation by 2-agonists has similar cardiac effects as 1-adrenoceptor stimulation. The 2-adrenoceptors become functionally more important in heart failure because 1-adrenoceptors become down regulated.
NE can also bind to 1-adrenoceptors found on myocytes to produce small increases in inotropy. Circulating catecholamines released by the adrenal medulla also bind to these same alpha and beta adrenoceptors in the heart.
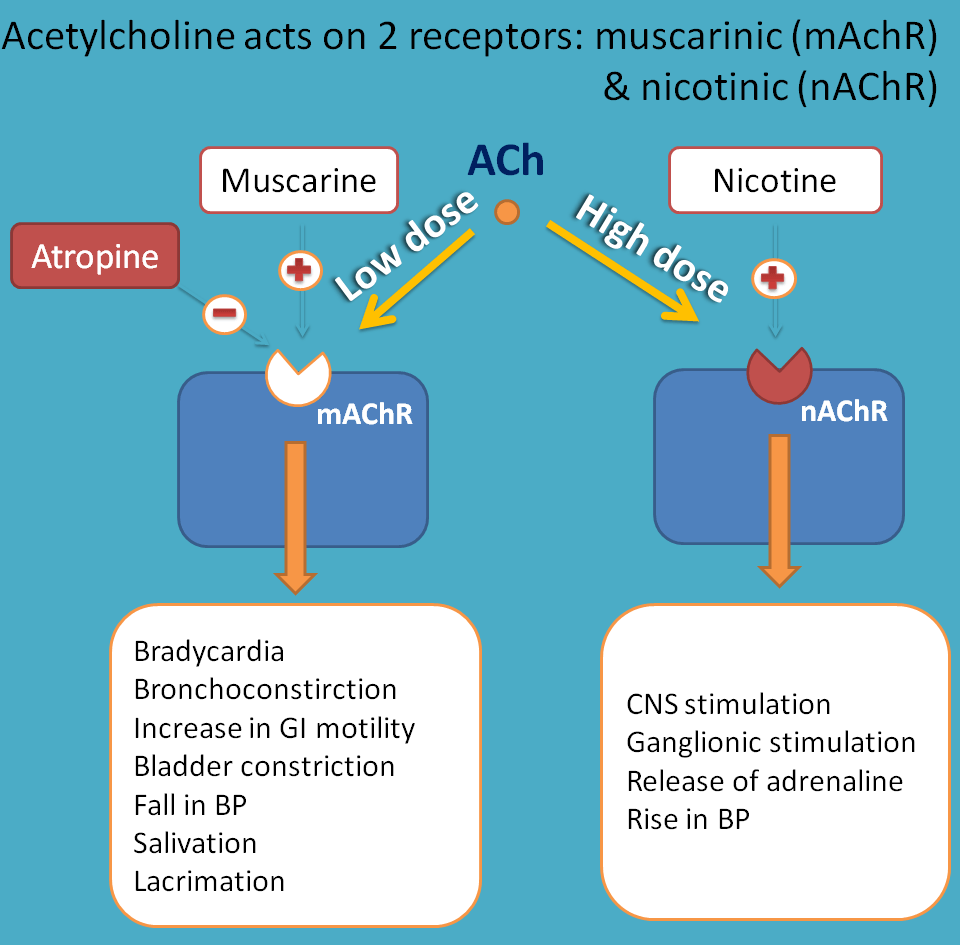
In addition to sympathetic adrenergic nerves, the heart is innervated by parasympathetic cholinergic nerves derived from the vagus nerves. Acetylcholine released by these fibers binds to muscarinic receptors in the cardiac muscle, especially at the SA and AV nodes that have a large amount of vagal innervation. ACh released by vagus nerve binds to M2 muscarinic receptors, a subclass of cholinergic receptors. This;produces negative chronotropy and dromotropy in the heart, as well as negative inotropy and lusitropy in the atria .
Revised 4/23/2014
What Is Acetylcholine Function Benefits + Dosage Of This Neurotransmitter
If youre familiar with nootropics supplements supplements that are capable of helping increase alertness, attention, learning and memory then you may have come across the compound called acetylcholine . What is acetylcholine exactly?
As one of the most abundant and important neurotransmitters in the body, acetylcholine plays a role in helping us focus, learn and memorize information. Its also needed to support muscle contractions, help with arousal and sleep, and facilitate the release of other important chemicals, such as dopamine and serotonin.
While acetylcholine supplements are not available , there are certain nutrients you can take in supplement form to boost synthesis of ACh, as well as foods to include more of in your diet.
Functions In The Peripheral Nervous System
Our peripheral nervous system could not carry out a large part of its functions if it did not have the presence of this neurotransmitter. The tasks it carries out are as many as relevant to our subsistence and well-being:
- It transmits the signals between our brain and the heart muscles.
- Likewise, it is that bridge between the brain, nerves, muscles, and bones that shape each of our movements.
- In the cardiovascular system, it almost always acts as a vasodilator, that is, it reduces and balances the heart rate.
- Also, in the gastrointestinal system, it favors digestive contractions.
- In the urinary tract, it prompts the voluntary sensation of evacuation.
- In addition, and as a curiosity, it should be said that acetylcholine also mediates in that process that also guarantees our survival: the perception of pain.
Also Check: How Can I Lower My Heart Rate From Anxiety
Functions In The Central Nervous System
In the central nervous system, aceticoline acts excitatory. Thanks to its interaction between neurons and nerve cells, it promotes the processes of motivation, excitement and attention.
Not only does it stimulate the activity of the hippocampus to carry out these processes, it also acts on the cerebral cortex so that we shape those higher executive functions, such as problem solving or reflection.
On the other hand, the main cause that cholinergic pathways lose their functionality in the central nervous system and stop communicating with each other is Alzheimers disease.
Acetylcholine and REM sleep
This data is interesting. Acetylcholine promotes REM sleep in our brain, and it does so by concentrating on a very special structure: the basal forebrain. Thanks to this, thanks to the fact that we enter this phase of paradoxical sleep or rapid sleep, we are able to better store the memories and information obtained during the day.
Endocrine functions
A part of our neurotransmitters, such as oxytocin, also act as hormones. In the case of acetylcholine, it must be said that it also has a very important endocrine function: it acts on the pituitary. In this way, you can control the amount of urine excreted, stimulate the production of thyroid hormones, etc.
Why Does The Heart Continue To Beat After Removed From Body
The heart can beat on its own
The heart does not need a brain, or a body for that matter, to keep beating. The heart has its own electrical system that causes it to beat and pump blood. Because of this, the heart can continue to beat for a short time after brain death, or after being removed from the body.
You May Like: What Is A Good Resting Heart Rate By Age
What Are The Effects Of Atropine On The Heart
Atropine is derived from the Atropa belladonna plant and its relatives, which are members of the potentially deadly nightshade family. The effects of atropine on the heart depend on the dosage that is administered. At lower dosages, the drug slows the heart. Higher dosages of atropine cause the heart rate to increase, and an overdose might be fatal.
One of the effects of atropine on the heart, the slowing of the heart rate at low dosages, occurs through central vagal stimulation. The parasympathetic vagus nerve serves to lower the heart rate. Atropine allows the sympathetic nerve to increase its dominance over the parasympathetic. This leads to a temporary rise in the patient’s acetylcholine levels; acetylcholines are the primary neurotransmitters for the parasympathetic nerves.
Increased dosages result in reduced vagal tone and a higher heart rate. An overdose of atropine results in falling arterial pressure and the inability of the heart to pump sufficient blood throughout the body. Other potential effects of atropine on the heart include ventricular fibrillation and tachycardia.
How Does Homeostasis Affect Heart Rate
4.3/5homeostasisheart rateon it here
Answer and Explanation:Homeostasis regulates heart rate by increasing heart rate when cells need more oxygen and decreasing heart rate when they need less oxygen.
Additionally, how does the cardiovascular system maintain homeostasis in the body? The cardiovascular system maintains homeostasis through the circulation of blood and, therefore, oxygen and nutrients to organs and tissues.
One may also ask, how does homeostasis affect heart rate during exercise?
During exercise, your heart rate increases to maintain a state of balance, known as homeostasis. “Homeostasis” means balance or equilibrium. During exercise, blood pressure, pulse and respiration increase to meet the increased demand for oxygen and nutrients by your musculoskeletal system.
How does the body increase heart rate?
The sympathetic nervous system releases the hormones to accelerate the heart rate. The parasympathetic nervous system releases the hormone acetylcholine to slow the heart rate.
You May Like: What Branch Of Medicine Deals With Heart Disease
Regulation Of Pacemaker Activity
The SA node displays intrinsic automaticity at a rate of 100-110 action potentials per minute. This intrinsic rhythm is primarily influenced by autonomic nerves, with vagal influences being dominant over sympathetic influences at rest.;This “vagal tone” reduces the resting heart rate down to 60-80 beats/min.;The SA node is predominantly innervated by efferent branches of the right vagus nerves, although some innervation from the left vagus is often observed.;Experimental denervation of the right vagus to the heart leads to an abrupt increase in SA nodal firing rate if the resting heart rate is below 100 beats/min. A similar response is noted when a drug such as atropine is administered. This drug blocks vagal influences at the SA node by antagonizing the muscarinic receptors that bind to acetylcholine, which is the neurotransmitter released by the vagus nerve. For heart rate to increase during physical activity, the medullary centers controlling autonomic function reduce vagal efferent activity and increase sympathetic efferent activity to the SA node. High heart rates cannot be achieved in the absence of vagal inhibition.
The rate of SA nodal firing can be altered by:
The Autonomic Nervous System
The autonomic nervous system is responsible for controlling many physiological functions. It induces the force of contraction of the heart and its heart rate. In addition, it controls the peripheral resistance of blood vessels. The ANS has both sympathetic and parasympathetic divisions that work together to maintain balance.
Read Also: Is Your Pulse And Heart Rate The Same Thing
How It Functions In The Body
What is the main role of acetylcholine? As a key neurotransmitter, it helps send signals to other cells, including neurons, muscle cells and gland cells.
It also modulates the release of other neurotransmitters, including dopamine, norepinephrine, and serotonin.
The network of nerve cells that use the neurotransmitter acetylcholine is referred to as the cholinergic system.
Some of the functions that acetylcholine has include:
- Stimulating skeletal muscles to contract.
- Inhibiting activation of the cholinergic system.
- Supporting neuroplasticity, specifically in the hippocampal and cortical regions. Neuroplasticity is defined as the ability of the brain to form and reorganize synaptic connections in response to learning or experience.
- Protecting against age-related declines in memory, including decline associated with Alzheimers disease.
- Supporting executive functions, which are considered higher-order cognitive processes. These processes are related to impulse control, planning, attention, decision-making and so on.
- Helping to guide vision-related attention.
- Regulating motivation, arousal and certain stages of sleep.
Health And Performance Considerations
Higher heart rates may be an indication of poor heart function and higher than usual stress being placed on the hearts ability to circulate blood. This may further indicate heart disease conditions.
From a performance stand point knowing specific heart rate training zones can optimize our bodys ability to adapt to performance requirements. Determining these zones can be done through many different methods, including VO2 or lactate testing, formulas and general training regimens. It then becomes necessary to monitor intensity in order to optimize your chances for success. To monitor your intensity there are several methods available to you. First is the perceived exertion method in which you rate your perception of how hard you are exerting yourself during a workout. The acronym for this is RPE . The scale on which to base your perceptions range from 1 – 10. See below.
The scale can be broken down as follows:
;;;;;0: Nothing
Recommended Reading: What Causes Your Heart Rate To Drop
Excised Perfused Heart Preparations
Mice were anesthetized with 4% isoflurane. After confirming a surgical plane of anesthesia, hearts were rapidly excised, and the aorta was cannulated. Hearts were then retrogradely perfused via Langendorff at constant pressure between 60 and 80 mmHg using a modified Krebs-Henseleit solution . Perfusate was buffered to a pH between 7.35 and 7.45, warmed to 37°C, and oxygenated with 95% O2/5% CO2. Before beginning each protocol, perfused hearts were allowed to stabilize at normal sinus rhythm for at least 5 min. Hearts were then positioned with the RA/SVC junction face up for photoactivation. Table 1 lists the number of animals used in each perfused heart study.
Why Is My Heart Beating So Fast While Resting
According to the Harvard Medical School, rapid heartbeat can be caused by stress, anxiety, dehydration, low potassium, low blood sugar, too much caffeine, hormonal changes and certain prescriptions and over-the-counter drugs. Other conditions that may cause heart flutters may include anemia or hyperthyroidism.
Also Check: Which Of The Following Signs Is Commonly Observed In Patients With Right-sided Heart Failure
Epinephrine Vs Norepinephrine And More
Adrenaline in your bloodstream also triggers the relaxation of smooth muscle cells throughout your body, notes StatPearls. When you experience significant physical or emotional stress, your adrenal gland produces two other hormones, called norepinephrine and dopamine, in addition to adrenaline and cortisol.
Along with adrenaline, norepinephrine and dopamine belong to a class of substances called catecholamines. According to Michigan Medicine, your doctor may test your blood or urine for the presence of excessive catecholamines if you have high blood pressure or a tumor called a pheochromocytoma, which is known to abnormally increase levels of both adrenaline and norepinephrine.
Cardiac Sympathetic Nervous System
The sympathetic nervous system is the component of the ANS that is responsible for controlling the human bodys reaction to situations of stress or emergency , while the parasympathetic nervous system is generally responsible for basal organ system function.
Cardiac sympathetic preganglionic nerves emerge from the upper thoracic segments of the spinal cord . After traveling a short distance, preganglionic fibers leave the spinal nerves through branches called white rami and enter sympathetic ganglia. The cardiac sympathetic neurons form the sympathetic chain ganglia located along the side of the viscera column . These ganglia comprise the sympatheric trunks with their connecting fibers. The postganglionic fibers, extend to the viscera, such as the heart. In general, sympathetic preganglionic neurons are shorter than sympathetic postganglionic neurons .
Sympathetic receptors: There are two types of adrenergic receptors: and . In the cardiovascular system there are 1, 2, 1, and 2 adrenergic receptors .
You May Like: How Long Does End Stage Heart Failure Last
Smoking Cigarettes Should Be Legal
A publicity campaign hoped to scare smokers straight by investing $54million in a commercial of cancer victims showing the truth behind smoking. The commercial was spread across the country; on televised public service announced, billboards and posters. The commercial showed a former smoker Terrie, 51, entering a room, putting on false teeth, pulling on a wig, and exposing the hole in her throat. Terri ‘s hole In her throat is called a stoma; a hole made in front of the neck to create a door for
What Controls Heart Rate
Heart rate is controlled by the two branches of the autonomic nervous system. The sympathetic nervous system and the parasympathetic nervous system . The sympathetic nervous system releases the hormones to accelerate the heart rate. The parasympathetic nervous system releases the hormone acetylcholine to slow the heart rate. Such factors as stress, caffeine, and excitement may temporarily accelerate your heart rate, while meditating or taking slow, deep breaths may help to slow your heart rate.;; Exercising for any duration will increase your heart rate and will remain elevated for as long as the exercise is continued. At the beginning of exercise, your body removes the parasympathetic stimulation, which enables the heart rate to gradually increase. As you exercise more strenuously, the sympathetic system kicks in to accelerate your heart rate even more. Regular participation in cardiovascular exercise over an extended period of time can decrease your resting heart rate by increasing the hearts size, the contractile strength and the length of time the heart fills with blood. The reduced heart rate results from an increase in activity of the parasympathetic nervous system, and perhaps from a decrease in activity of the sympathetic nervous system.
Don’t Miss: Who Invented Open Heart Surgery
Action Potential Characteristics Of Sa Nodal And Atrial Myocytes
Figure 1. Action potential characteristics of isolated rabbit SA nodal and atrial myocytes. Typical action potentials of an isolated SA nodal myocyte and an atrial myocyte. The atrial myocyte was stimulated at 3 Hz. Action potential parameters of SA nodal and atrial myocytes, including maximum diastolic potential , action potential amplitude , maximum upstroke velocity , and action potential duration at 20, 50, and 90% repolarization . The atrial myocytes were stimulated at 3 Hz. Asterisks indicate significant differences between both cell types. Frequency dependence of the action potential parameters of the atrial myocytes. Asterisks indicate significant differences between stimulus frequencies.
How Do You Remember Anticholinergic Drugs
Students often learn the adverse effects of anticholinergics from a mnemonic, e.g.: Blind as a bat, mad as a hatter, red as a beet, hot as a hare, dry as a bone, the bowel and bladder lose their tone, and the heart runs alone. This refers to pupillary dilation and impaired lens accommodation, delusions,
Read Also: What Is Bpm Heart Rate
What Is The Role Of Acetylcholine In Blood Pressure Regulation
I hope this answers your question:
So the heart is an electrically excitable tissue: it pumps due to action potentials that start from specialized heart cells called nodal cells and these nodal cells spread the action potential to surrounding heart cells. These nodal cells are found throughout the heart and they make up what’s called the conducting system. These nodal cells don’t need neural or hormonal input for them to spread action potentials, they have this mechanism to spontaneously start action potentials on their own called a pacemaker potential, BUT they can be influenced by neural or hormonal input. These external inputs change the frequency of the heart beat by influencing the pacemaker potential of the nodal cells.
I unfortunately do not know how acetylcholine affects blood pressure. I’ve read a paper of how acetylcholine induced relaxation in hypertensive rats, but I’m not sure of the mechanism, like how it affects systolic or diastolic BP.
Content Background: Acetylcholine Neurotransmission In The Nervous System
![09 cardiac health, fitness and disease[1] 09 cardiac health, fitness and disease[1]](https://www.healthyheartworld.com/wp-content/uploads/09-cardiac-health-fitness-and-disease1.jpeg)
Definitions:1 a neurotransmitter stored in vesicles of nerve terminals; it is found in neurons within the central nervous system, the somatic nervous system, the parasympathetic nervous system and the sympathetic nervous system.2 the connection between two neurons; neurotransmitters are released from the terminal into the synaptic space and bind to receptors on the neighboring neuron.3 a protein to which hormones, neurotransmitters and drugs bind. They are usually located on cell membranes and elicit a function once bound.4 an atom, radical, or molecule that has gained or lost one or more electrons. Therefore it acquires a net negative or positive charge.5 part of the autonomic nervous system which controls the functions of organs and tissues especially during times of stress, fear and emergencies. It consists of 2 types of neurons, pre-ganglionic and post-ganglionic. The pre-ganglionic neurons release acetylcholine and the post-ganglionic neurons release norepineprine.
Figures:
Figure 5;An acetylcholine synapse; the axon terminal releases acetylcholine, which binds to acetylcholine receptors. From: Gross de Nunez & Schwartz-Bloom, 1997; for full citation, see;Resources
Figure 6Acetylcholine binds to its receptors & opens Na+ channels. The influx of Na+ generates an electrical current across the cell membrane. From: Gross de Nunez & Schwartz-Bloom, 1997; for full citation, see;Resources
PEP
Read Also: Can This 10 Second Trick Prevent Your Heart Attack
