When To Seek Help
Patients with a life expectancy shorter than six months are eligible for hospice care. A hospice provides additional aid and resources to assist the person in living comfortably and with the highest possible quality of life. Hospice caregivers can also help patients and their families plan for future needs and circumstances. They have a unique insight into how to assist those with these difficulties.
Patients with end-stage heart failure need medical continuity throughout outpatient programs. These are just some of the symptoms that hospice care might help with. Positive inotropic drug infusions, anxiolytics, and sleeping medicines are all viable treatments. Its challenging for patients, families, and doctors caring for patients with end-stage heart failure to identify when treatment goals shift from survival to quality of life, allowing for a peaceful and dignified death.
Taking Care Of Yourself
Knowing youre coming towards the end of your life can be scary and upsetting. You may even feel angry. You might find that these feelings are made worse by the constant coverage of the coronavirus pandemic and the discussions about death on the news as well as the unknown, and the thought of leaving family and loved ones behind.
-
Visit our emotional support hub to get help for anxiety, depression and loneliness.
It can really help your mental wellbeing to keep a sense of structure in your life and practice self-care. Depending on your symptoms and how youre feeling, you might not feel up for doing this. But if you can, try to:
-
bathe everyday
-
do gentle activity exercise if you can, or try to move about
-
do things you enjoy hobbies/reading/watching TV
-
keep in contact with family and friends via telephone or social media.
Dont Miss: Can Flonase Cause Heart Palpitations
For Patients With Heart Failure Little Guidance As Death Nears
Americans are living longer with heart disease, managing it as a chronic condition. But there are few rules for these patients as they near the end of life.
Ricky Hurst, whose heart is failing, was told by doctors to get his affairs in order as his condition worsened. More patients like him are living longer with heart failure, but there are no widely accepted guidelines for care as they near death.Credit…Sean Proctor for The New York Times
Supported by
-
Send any friend a story
As a subscriber, you have 10 gift articles to give each month. Anyone can read what you share.
Give this article
By Gina Kolata
Ricky Hursts doctors told him last year that there was nothing more they could do. His heart was failing and he should get his affairs in order. The end was coming.
His family gathered. He spoke to his pastor and resigned himself to death. If it was meant to be, it was meant to be, he said.
But. Mr. Hurst, 56, a former ranger and school football coach in Jackson, Mich., is still alive, although his heart continues to weaken. And patients like him are raising a new dilemma for doctors.
Their disease at that point is called heart failure their weakened heart cannot pump enough blood to supply the bodys needs. The number of Americans with heart failure increased to 6.5 million in 2011-2014 from 5.7 million in 2009-2012, according to the American Heart Association.
And often doctors do not tell patients what to expect.
Recommended Reading: What Is Heart Failure With Preserved Ejection Fraction
Weeks Before Death Symptoms
Several weeks before death, your loved one may start exhibit a range of behavioral changes relating to their sleeping patterns, eating habits and sociability. They may begin to sleep more often and for longer periods. They will start to refuse foods that are difficult to eat or digest, but eventually they will refuse all solid foods. Do not try to force them to eat, as it will only bring discomfort to them. Your loved one may enjoy ice during this time, since it will keep them cool while also hydrating them.
Unfortunately, your loved one may become withdrawn, less active and less communicative. They may spend more time alone introspecting and may turn down company. Some also appear to become comatose and unresponsive, but this is a symptom of withdrawal. Your loved one can still hear you, so speak in a calm, reassuring voice while holding their hand. Children may become more talkative, even if they withdraw from other activities. Its important to let your loved one set their own pace during this time. Your loved one may also start to use metaphorical language, which could be a way of coping with death. It may also be used to allude to a task they feel they need to accomplish, such as seeking forgiveness.
Common symptoms in this period also include physical changes, such as:
- Chronic fatigue
- Swelling of the abdomen, such as edema or ascites
Days Before Death Symptoms
In the days before death, a series of physiological changes will occur. Their pulmonary system will start to degrade and the will become congested, leading to a tell-tale death rattle. Their breathing will also exhibit fluctuations, as they may begin to respirate up to 50 times per minute or as little as six. When exhaling, they may puff their lips. They may also begin to cough more frequently, but in general, the congestion itself is painless.
During their last days, your loved one may begin to experience hallucinations in which they talk to people who arent there or who have also died. It is important to maintain a close eye on your loved one if they begin exhibiting these symptoms. There is no guarantee for how long they may have left, and some people pass through this process faster than others.
Some common symptoms those a few days from death experience include:
- A drop in blood pressure
- The body temperature changes frequently
- Skin changing color or becoming blotchy
- Erratic sleeping patterns
Read Also: How To Lower Heart Rate With Exercise
Caring For Someone With Heart Failure Towards The End Of Life
Please be aware – this information is for healthcare professionals.
You can use our My Learning form to reflect on how this page has helped with your continuing professional development.
If you’re a patient, or a family member or friend, you can find more information on heart failure from the British Heart Foundation .
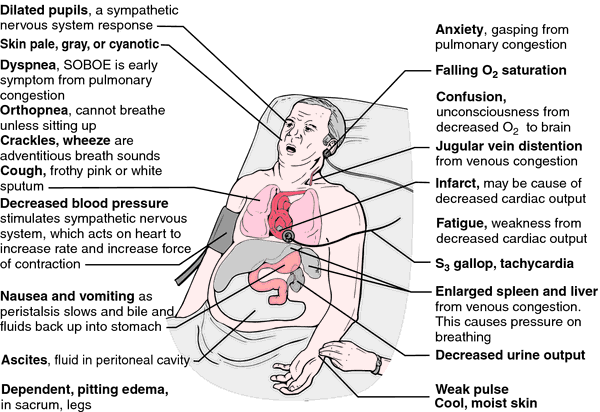
Heart failure means the heart is not pumping blood around the body as well as it should. People with heart failure may have symptoms such as fatigue, breathlessness and oedema . Here, we’ll talk about knowing when a patient with heart failure is near the end of life, and how to support them.
This information is about supporting adults with advanced heart failure.
On this page:
Thinking About What Care And Treatment You Would Like
For different heart conditions, there are different things you might need to consider when approaching the end of life:
-
Some people with heart failure are at risk of dying suddenly because they may develop a life-threatening heart rhythm. This can lead to a cardiac arrest. You may want to think about what you would want to happen if you had a cardiac arrest and whether you would want to have CPR or not. Without CPR, your heart rhythm would not be restored, and you would die.
-
If you have an ICD fitted, you might want to discuss whether to deactivate it . This would mean that if you were to have a cardiac arrest, your ICD wouldnt be there to restore your heart rhythm which would help to minimise any discomfort or distress. Read our ICD deactivation FAQs for more information.
-
Antibiotics are given to help your body fight infection. You may decide to refuse antibiotics.
Its good idea to involve loved ones in these kinds of decisions so theyre aware of your wishes. You might also want to discuss matters like organ donation and how you intend for your wishes to be recorded.
Don’t Miss: What Is Normal Resting Heart Rate By Age
End Of Life Care Through Your Loved Ones Dying Process
Hospice care allows you to share your loved ones most difficult journey with them, which can make it easier for you and them to obtain closure. Providing a high quality of life should be your main focus, which may be easier early on when you can still participate in a range of activities together. To properly care for them later in the dying process, make sure they are hydrated and fed without forcing anything on them. It will be normal for your loved one to become somewhat dehydrated during their final days. You may also have to clean them and move them to avoid bedsores.
Maintaining good communication with your loved one can help you provide them with the best possible support during their last days. In doing so, you may find that you both may want to spend time alone. This can help both of you cope with the dying process and allow you to better appreciate the time you have together. Your loved one can also let you know of any medical care they wish to receive or refuse should they become unresponsive.
When Is The Right Time To Ask About Hospice For End
Determining when hospice care is appropriate for end-stage congestive heart failure can be difficult for patients, families and even physicians. Congestive heart failure in its final stages is often unpredictable, and symptoms can vary.
Typically, patients experience a recurring cycle of dramatic decline followed by a period of recovery. As a result, the majority of heart disease patients who could benefit from hospice care never receive essential emotional and physical support.
Read Also: Congestive Heart Failure And Copd
What Does Moving To Hospice Care Involve
If you and your family have made the decision to pursue hospice care while receiving inpatient care, a case manager or social worker can help facilitate the process. If you are at home and would like to transition to hospice care, hospice agencies can help make the arrangements. Hospice agencies will review your needs and have a doctor order the appropriate medications for you. These medications will focus not on treating your condition, but on managing your symptoms and comfort as much as possible.
Hospice For Heart Disease & End
If you are reading this, it is likely you or someone you love has been waging a difficult physical and emotional battle against heart failure or some form of heart disease. Your search for comfort, support and answers does not stop when you accept that you must learn to live with heart disease. Thats when VITAS can help.
Hospice helps patients and their families deal with the significant impact of heart disease after curative treatment has stopped. On this page, we’ve provided answers to these questions:
- When is the right time to ask about hospice?
- What can hospice do for a person with heart disease?
- What can hospice do for the family of a person with heart disease?
- What are the overall benefits of hospice care?
- How can I approach my hospice discussion with family members and loved ones?
You May Like: What Are Symptoms Of Heart Failure
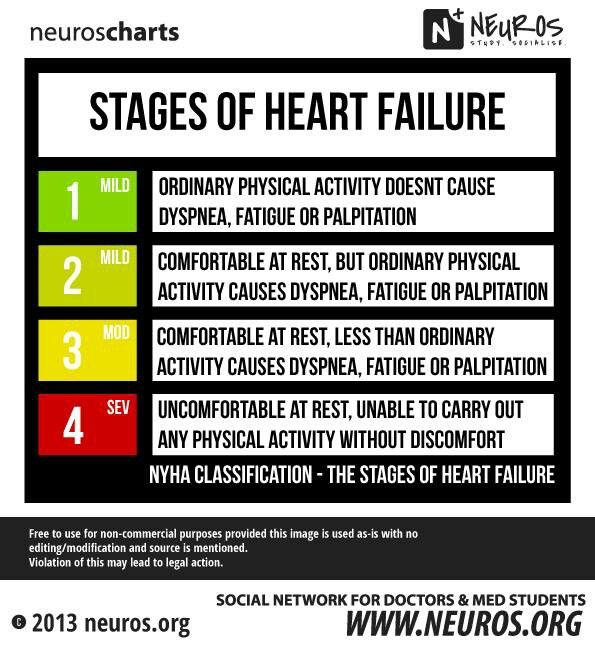
Stage 3 Of Congestive Heart Failure
Its not uncommon for congestive heart failure to be accompanied by other heart conditions. If you are diagnosed with stage three CHF, along with another heart condition, its likely that youll have difficulty performing regular tasks. Small bouts of exercise or minimal doses of physical activity will cause the same symptoms mentioned in stage two fatigue, shortness of breath, and heart palpitations. In stage three, lifestyle changes are not as effective, and a surgical procedure may be necessary. However, its never too late to talk to a doctor about your heart condition and what the future may look like.
What You Can Do For Your Loved One
In addition to symptom management, its important for the family caregiver to learn how to recognize the end-of-life signs for CHF, and when they should contact hospice. Hospice care will be able to address the specific needs of CHF patients in their final days, and help them to get the most out of what time they have left.
Recommended Reading: Does Xanax Help Heart Palpitations
How Can I Approach A Hospice Discussion With Family Members And Loved Ones
The final months of life are frequently marked by strong emotions and hard decisions. Talking about hospice, even with those closest to you, can be difficult. Here are some tips to get the discussion started.
For patients speaking to families
Education is key. Educate yourself first. By now, youve probably done some research online. It may be helpful to read and share Considering Hospice: A Discussion Guide for Families at HospiceCanHelp.com. This discussion guide is a tool for you to print out and use in a family discussion.
Determine what your family members know. Before bringing up hospice, make sure your family members and caregivers have a clear understanding of your health status. People handle difficult information in different ways. If family members do not accept or understand your prognosis, ask your physician, clergy, a VITAS social worker or a trusted friend to speak with them on your behalf.
Discuss your goals for the future, as well as theirs. As a patient, your greatest concern might be to live without pain, to stay at home or not to be a burden. Ask your family members/caregivers about their concerns as they consider the coming days, weeks and months. Explain that hospice is not giving up. It is an active choice to ensure that everyones needs are met.
For families speaking to patients
You May Like: Tylenol And Heart Palpitations
Cold Hands And Feet And Skin Mottling
Emilija Manevska / Getty Images
Hands and feet may become colder and the skin may look blotchy and purplish . It happens because the heart is no longer able to pump blood as well. As a result, blood pressure goes down and the skin grows colder.
This mottling may slowly work its way up the arms and legs. The lips and nail beds can turn blue or purple too.
You May Like: What Is Happening During The pause Phase When The Heart Is Resting (relaxing)
Dying From Heart Failure: Lessons From Palliative Care
Increasing interest and research into the care of the dying over the past 25 years have resulted in better symptom control, psychological support, and choice for people dying from cancer and their families.1 Little attention has been paid, however, to patients with other life threatening diseases, such as AIDS, neurological conditions, respiratory failure, and heart failure. Palliative care, with its emphasis on the care of patients whose prognosis is limited, on quality of life, and on a multidisciplinary approach, may benefit patients other than those with cancer. One such group is patients dying from heart failure.
Heart failure is the only major cardiovascular disease with increasing prevalence, incidence, and mortality. Incidence and prevalence both increase dramatically over the age of 75 yearsup to 43.5 and 190 per 1000 population respectively.2 With age adjusted mortality from cardiovascular disease declining and the size of the elderly population growing, the absolute number of individuals living with compromised cardiac function is expected to increase dramatically over the next few decades.3 Modern treatments for heart failure slow but do not arrest progression of the disease. Despite the wealth of therapeutic advances, quality of life in chronic heart failure is poor4 and discomfort and distress often worse than in cancer.5
What Happens If You Have Heart Failure
People with heart failure have weak hearts that dont work as well as they should. Over time, the illness causes significant damage to the body.
In the first stages, the heart is less effective. It stretches, grows bigger, and pumps faster to compensate for the lack of strength. The body also changes, with arteries getting smaller and blood being directed away from certain body parts. Many people with heart failure dont know they have a problem in these early stages.
Towards the end stages of CHF, symptoms will worsen even if lifestyle changes are made, and the body will be unable to compensate for the loss of blood flow. As soon as that happens, the person may start to feel tired, have trouble breathing, and have other problems.
People can get help managing their end stages congestive heart failure symptoms and slowing down the progress of their condition with a variety of treatments. Its a long-term condition that cant be cured, as well as heart failure. People will eventually reach the end stages of heart failure.
Even when the person is lying down, they feel a shortness of breath. Their symptoms can change rapidly over a short period of time.
Don’t Miss: What Is Your Heart Rate Supposed To Be
How Long Can You Live With End
Heart failure is a chronic, progressive condition that worsens with each flare-up. Your outlook and prognosis are better if you are healthy overall, you have been following your treatment plan, and you are responding well to your treatments. Being willing to pursue invasive treatments like a heart transplant will also increase your life expectancy.
Comforting A Loved One With End Stage Heart Failure
According to the American Heart Association, the number of adults in the United States with heart failure rose by 800,000 over the last five years. About 10 percent of the 5.7 million people in the country currently living with heart failure in its end stages. Heart failure also tends to occurs at equal rates in men and women. If you have a family member who is suffering from end stage heart failure, you may be concerned about how to make sure that he or she is as comfortable possible. Hospice care can provide what your loved will need as his or her deals with the end stages of heart failure.
Have a loved one with end stage heart failure?call us at 509-5276 or contact us online.
Recommended Reading: How Does Fitbit Calculate Resting Heart Rate
