What Is Chronic Obstructive Pulmonary Disease
Chronic obstructive pulmonary disease, better known as COPD, is a progressive lung disease that affects a persons ability to breathe. While the main cause of COPD is smoking, other risk factors can include excessive exposure to:
- Toxic fumes and gases introduced in the workplace
- Second-hand air pollutants
- Smoke from fires
Over time, this disease can rear its head in two ways: chronic bronchitis or emphysema. Most people living with COPD will experience a combination of both conditionsinvolving a productive cough that produces mucus and permanent damage to the lungs. Because symptoms of COPD develop slowly, most diagnoses occur later in life. According to medical professionals, this makes COPD one of the most common diseases affecting seniors today. Therefore, if you notice any of the following long-term symptoms in your elderly loved one, you should have a healthcare provider test for lung function and capacity:
- Wheezing
- Recurring respiratory infections
Advice For The Caregiver
When it comes to monitoring your loved ones COPD symptoms, understanding the triggers that can worsen the diseasesuch as CHFcan help ensure they receive the best medical treatment. While there is no cure for COPD, there are treatment plans and therapies that can help the slow the progression of the disease. This involves recognizing, tracking, and introducing preventatives to deter additional complex medical conditions, like CHF and upper respiratory infections, from exacerbating the condition. Some treatment options that you can introduce as a caregiver, include:
- Encouraging healthy habits. Light exercise, positive thinking, and well-balanced meals can do wonders for those with progressive health conditions. Its also imperative that caregivers do their best to sway smoking habits in those with COPDone of the leading causes of the disease.
- Organizing the home. By keeping the home organized, you can save your patient precious time and energy in searching for what they need.
- Improving indoor air quality. Air quality is especially important to consider when caring for someone with COPD, as it can affect their ability to breathe. Consider investing in air purifiers and keep windows closed.
At the end of the day, the best thing a COPD caregiver can do is be prepared. As a progressive disease, COPD will eventually worsen. If you notice any of these severe symptoms, reach out to a healthcare provider:
- Trouble performing routine activities
Copd Vs Chf: Similarities And Differences
Chronic obstructive pulmonary disease and congestive heart failure can leave you feeling short of breath. These two serious conditions share many symptoms and common risk factors. But the causes and treatments of each are very different.
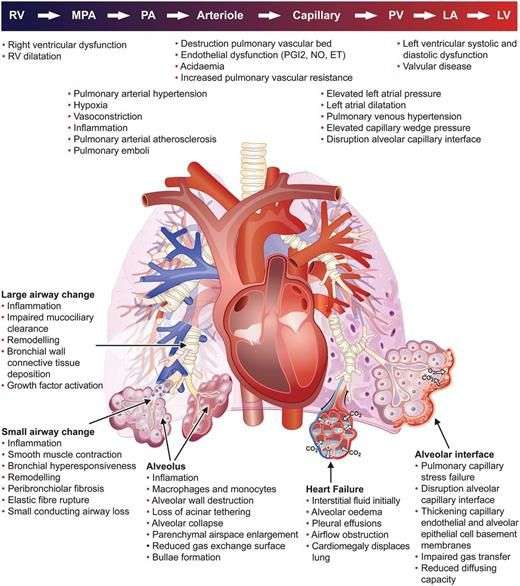
COPD is a term for several types of serious respiratory conditions that block airflow to the lungs. The two main COPD conditions are chronic bronchitis and emphysema. These diseases leave your lungs unable to work at full strength, making it difficult to breathe.
With bronchitis, the airways that extend from your trachea into your lungs become irritated.
Emphysema occurs when serious damage is done to the tiny air sacs in your lungs where oxygen and carbon dioxide are exchanged.
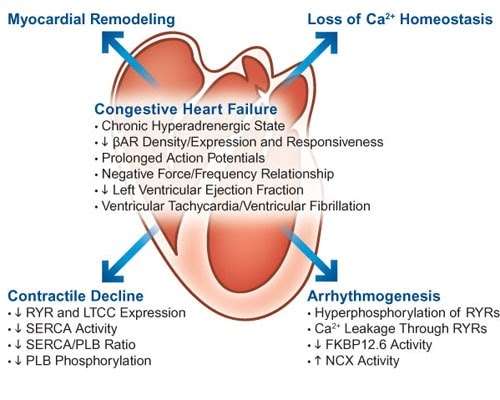
CHF occurs when your heart becomes too weak to pump blood through your body. When blood isnt pumped out of the heart effectively, fluid levels build up or become congested.
When blood backs up or pools in the heart, the heart beats more rapidly and expands to handle the greater volume of blood. This makes heart failure worse.
Similar symptoms
Shortness of breath and wheezing are symptoms of both COPD and CHF. Breathing difficulties are usually experienced after physical activity and tend to develop gradually.
At first, you may notice feeling out of breath after simple activities such as climbing a set of stairs. As COPD and CHF worsen, shortness of breath or wheezing may occur with little physical effort.
You May Like: How Is Congestive Heart Failure Treated
Why A Cough May Be An Important Sign Of Heart Failure
If you have a long-term cough with congestive heart failure, that cough is something to pay attention to. It’s called a cardiac cough and it may indicate that:
- Your heart condition is getting worse
- Treatment isn’t working as well as it needs to be
- You’re having side effects from your heart-failure medication
- You have undiagnosed heart failure
This article explores the symptoms and causes of a cardiac cough and when to get medical help for it.
Verywell / Laura Porter
Reninangiotensinaldosterone System Inhibitors Aceis And Arbs
The reninangiotensinaldosterone system has been implicated in various processes in the lungs that may be important in the pathogenesis of COPD, including the induction of pro-inflammatory modulators, the generation of reactive oxygen species and the development of pulmonary fibrosis . Data on the effects of RAAS inhibitors in patients with COPD are limited, although a couple of small studies have indicated a potential benefit on pulmonary function and haemodynamics . More recently, an analysis of the Multi Ethnic Study of Atherosclerosis , including individuals in the general population aged 4584 years who had no clinical evidence of CV disease, found that baseline use of an ACEI or ARB protected against the progression of emphysema, especially when prescribed at high doses . The authors attributed the effects of such RAAS inhibitors to inhibition of transforming growth factor- signalling in the lung, thereby reducing the progression of airspace enlargement.
You May Like: Women’s Heart Attack Warning Signs
Causes Of Cardiac Coughing
Congestive heart failure causes excess fluid to build up in your body. That adds to your blood volume and can ease the strain on your heart.
When this fluid builds up in the alveoli in your lungs, it’s called lung congestion. The cardiac cough is your body’s attempt to clear out the fluid.
Causes of lung congestion include:
- Worsening heart failure
- Your prescription heart medication not working as effectively as it should
- Not taking your heart medication as prescribed
- A side effect of angiotensin-converting enzyme inhibitors, a type of medication commonly prescribed for heart failure
The cough from ACE inhibitors tends to be a dry, hacking cough. If it’s bad enough, you may need to switch to a different heart medication.
If you suspect this side effect, let your healthcare provider know right away. Don’t stop taking your heart medication without their approval, even if you think it’s triggering your cough.
Restrictive Pulmonary Function Tests
Restrictive ventilatory defects predominate in patients with stable HF.48 FEV1 and FVC were normal or proportionately reduced in a multicentre study of 130 patients.49 Contributory factors include interstitial fibrosis,50 respiratory muscle weakness,45,51,52 cardiomegaly, and pulmonary congestion.53 FEV1 and FVC may also be proportionately reduced with a normal ratio in patients with severe chronic obstructive pulmonary disease and gas trapping. Usually in such cases increased total lung capacity and residual volume help diagnose obstruction.39 However, restricted lung volumes mask hyperinflation and thus the diagnosis of chronic obstructive pulmonary disease in patients with concurrent HF.6
Recommended Reading: How To Tell Your Heart Rate
What Are The Radiological Findings Of Congestive Heart Failure
The radiological tests conducted and their findings are as mentioned below:
Chest X-Ray
A chest X-ray can be used to view both the heart and lungs. The chest X-ray can assess the size of the heart and the fluid accumulation in the lungs.
Based on the progression of CHF, 3 phases have been described, which are as follows:
– Phase 1: Vascular Phase
-
This represents the first phase of CHF and signifies pulmonary venous hypertension.
-
Cardiomegaly is evident.
-
Prominent upper pulmonary vessels, in contrast to lower blood vessels, are evident in healthy individuals.
-
Hilar level sees an increase in the artery to bronchus ratio, which appears as white round densities.
-
The pulmonary artery is more prominent in diameter than the bronchi .
-
Hilar haziness and fullness: Pulmonary veins are enlarged, and fluid is seen collecting around the vessels.
-
Vascular redistribution is not seen in supine X-rays .
– Phase 2: Interstitial Phase
-
Kerley lines .
-
They occur due to interstitial edema and amplified lymphatic drainage.
-
The bronchial wall thickening appears as a white rim around the bronchioles, which appear dark.
-
Thickening of the fissures between the lobes of the lungs.
– Phase 3: Alveolar Phase
Computed Tomography
-
CT is not generally recommended to diagnose heart failure. However, it can reveal any congenital or valvular diseases if present.
-
Thickening of the septal lines will be evident.
-
Ground-glass opacity appearance .
Magnetic Resonance Imaging
Stress Test
Coronary Angiogram
Recognising And Managing Comorbid Copd And Cvd
Comorbidity in COPD is common and can be fatal. Therefore, in order to treat patients appropriately, physicians should proactively search for prevalent and clinically important comorbidities such as CVD. The three most commonly occurring cardiac comorbidities of COPD are AF, HF and IHD . However, non-specific symptoms such as dyspnoea and fatigue are common to all four diseases and acute exacerbations of each of these conditions can result in exacerbation of respiratory symptoms. Indeed, acute respiratory symptoms invariably have mixed pulmonary and cardiac origin . Diagnosing and managing comorbid COPD and CVD and their exacerbations thus remain challenging .
Read Also: Can Anesthesia Cause Heart Attack
How Do You Know Which Is Which
Unfortunately, because the symptoms are so similar, it’s hard for you to know which condition you might be experiencing, or which one is causing your symptoms to worsen. This is why you’ll need the advice of your doctor. The doctor will perform a physical exam to detect uniquely-CHF symptoms such as rales or leg swelling. They may also look for heart rhythm irregularities or swelling of the neck veins. Chest x-rays, echocardiograms, and certain blood tests can also be used to detect CHF.
Theoretical And Clinical Study Benefits Of
There are several theoretical reasons why -blockers could be protective in the COPD population . COPD and heart disease share environmental risk factors and both share pathophysiological factorshigh adrenergic activation and increased systemic inflammation.,, A deterioration or exacerbation of either disease will increase both the adrenergic and inflammatory state, which could potentially worsen the other condition. Furthermore, -adrenergic activation and immunomodulation are linked. -blockers have been shown to reduce cytokines in patients with heart failure and improve outcomes in sepsis. So, first, -blockers may reduce the background risk of exacerbation of both COPD and heart disease by lowering both the background adrenergic and inflammatory states .
Second, during an exacerbation of COPD, there are yet higher circulating catecholamines. This increases the risk of myocardial ischaemia, tachycardias, deterioration in heart failure and hypertension . -Blockers could counteract all of these endogenous exacerbation-associated cardiovascular risks.
Recommended Reading: Why Use A Heart Rate Monitor
Follow Your Treatment Plan
Both COPD and CHF are serious chronic conditions that can affect your breathing and your quality of life. They are similar in terms of symptoms and outlook, and many patients do suffer from both conditions. While they can occur independently, it’s important to understand how they are connected too.
Your best bet if you have both COPD and CHF is to follow your treatment plans to the best of your ability, practice a healthy lifestyle, and keep in close contact with your health care team. All of those things can help prevent exacerbations. Plus, take action right away if you start to notice your symptoms worsening at all or if new symptoms arise. That can help flare-ups from spiraling out of control.
Problems Diagnosing Heart Failure With Preserved Ejection Fraction In Patients With Chronic Obstructive Pulmonary Disease
Defining and identifying HF with preserved ejection fraction is controversial and problematic in any population. These difficulties are magnified in patients with chronic obstructive pulmonary disease. BNP levels are moderately elevated in both HF-PEF and cor pulmonale.3638 One small study compared 17 patients with chronic obstructive pulmonary disease against 9 patients with HF-PEF, defined by clinical and radiological pulmonary oedema responding to treatment, sinus rhythm, and preserved LV ejection fraction. BNP levels were significantly higher in those with HF-PEF .34 However, BNP was < 100 pg/ml in four of the nine patients with HF-PEF, while few patients with chronic obstructive pulmonary disease had significant pulmonary hypertension . More robust studies are required to determine the diagnostic accuracy of BNP for HF in patients with chronic obstructive pulmonary disease and varying levels of pulmonary hypertension.
Also Check: How Do You Calculate Your Target Heart Rate
If You Think You Have Heart Failure
Because the symptoms of heart disease and heart failure frequently overlap with symptoms of COPD, it’s important that you pay close attention to your body and report any of the following findings to your healthcare provider:
- Chest pain or discomfort
- Fatigue, lethargy, or daytime sleepiness
- Muscle wasting
- Dyspnea, orthopnea, or paroxysmal nocturnal dyspnea
- Swelling in the lower extremities
Just like COPD, early diagnosis of heart disease or heart failure is important. The earlier you’re diagnosed, the earlier you can seek treatment.
Untreated heart problems can worsen your COPD symptoms and your overall prognosis. In fact, people with both conditions often fare worse, having longer hospital stays and a higher mortality rate than people who have COPD or heart problems alone.
Pharmacological Management Of Copd And Cvd
With the close association between COPD and CVD, it is possible that treatments for one condition may influence the other and appropriate treatment of all conditions is therefore essential. Improvements in survival following hospital discharge for acute COPD exacerbation have been attributed to better management of COPD and associated comorbidities, including the use of CV therapies such as angiotensin-converting enzyme inhibitors , angiotensin receptor blockers , -blockers and statins . However, the treatment of CV conditions in patients with COPD is associated with therapeutic challenges, most notably the co-administration of 1-blockers and 2-agonists. -blockers are widely prescribed in the treatment of CVD and -agonists represent a cornerstone of COPD treatment however, the two have opposing pharmacological actions and physicians may be concerned that treatment of one condition may worsen the other .
Don’t Miss: How To Rule Out Heart Attack At Home
Easyliving Interventions: Managing Chf At Home
Our nurse develops a detailed and clinically-driven care plan, including signs and symptoms to monitor.
Our caregivers provide in-home CHF support, including:
- Meal Preparation – Help clients prepare healthy meals with reduced sodium and other dietary guidelines. Monitor fluid intake as indicated by the care plan.
- Companionship/Observation – Provide socialization and stress reduction. Help monitor client breath sounds, oxygen saturation, vitals, weight gain and swelling.
- Medication Assistance – Ensure clients are taking medications properly and report any concerns.
- Toileting – Carry out the toileting plan such as use of a bedside commode and accessing the bathroom regularly as diuretics will cause frequent urination. Ensure proper hygiene to prevent UTIs and other issues.
- Housekeeping – Help keep the home clean and orderly. Complete household tasks to reduce stress and exertion that can cause shortness of breath, dizziness and falls.
- Encourage active and passive exercises to help prevent worsening of the condition.
- Assist with other supportive services such as elevation and positioning, safely getting about the home, and more.
Remote Patient Monitoring/Care Technology
With EasyLiving’s Care Technology, we track and monitor vital signs for any potential concerns. We offer a comprehensive care management program to monitor/manage your condition, give you the support you need, identify resources throughout different stages, and coordinate your care team.
Should Patients With Chronic Obstructive Pulmonary Disease Be Screened For Heart Failure
Asymptomatic LVSD fulfils the WilsonJunger criteria for successful screening: the condition is medically important and clearly defined, with effective treatment, an established natural history and early asymptomatic stage, detectable by an acceptable and safe, valid and reliable test applicable to the target population, resulting in cost-effective screening for which adequate resources exist. The predictive value of screening is critically dependent on disease prevalence. The high prevalence of LVSD in patients with COPD thus favours success. Sequential peptide testing and then echocardiography may counter the inherent limitations of peptides or echocardiography alone in pulmonary disease. Robust randomized trials are required to determine the efficacy and cost-effectiveness of such screening. Such a trial is currently being planned.
Also Check: Left Sided Heart Failure Treatment
Copd And Chf Often Occur Together
Experts are not entirely sure exactly why people with COPD can also have heart failure. But as mentioned earlier, the lung damage from COPD does place extra stress on the heart. In the end, both conditions result in respiratory symptoms. When they occur together, studies show that the risk of negative outcomes is much increased4
Congestive Heart Failure Lung Sounds
Congestive heart failure lung sounds
Congestive Heart Failure Lung Sounds. Chest pain that radiates through the upper body. As the disease progresses and the bases fill with fluid, basilar sounds will become diminished or absent with crackles heard in the upper lobes. Swelling in the hands, feet, and. These sounds can also occur if a foreign.
Adventitious Sounds: Types, Diagnosis, When To Seek Help From verywellhealth.com
People with congestive heart failure often have pulmonary edema. This includes asthma, emphysema, pneumonia, acute bronchitis, chronic bronchitis, congestive heart failure, and more. Short of breath, especially when lying. One with pneumonia, one with interstitial pulmonary fibrosis , and one with congestive heart failure . Background although congestive heart failure patients typically present with abnormal auscultatory findings on lung examination, respiratory sounds are not normally subjected to additional analysis. First and second heart sounds normal and unsplit.
Also Check: What Is The Normal Heart Rate Per Minute
Chronic Obstructive Pulmonary Disease
In England, the Department of Health estimates that 3.2 million people have COPD and 40% of these patients also have heart disease, especially heart failure., People with COPD and heart disease have a particularly high risk of death from heart disease and stroke . As -blockade is highly desirable in this high-risk group, it is therefore very important to sort out the thorny issue of whether any, some or all of these patients can be given a -blocker and how this can be safely achieved in everyday clinical practice and not just within a carefully monitored study population.
The definition of COPD includes airflow limitation that is not fully reversible. Theoretically, patients with COPD have significant fixed, irreversible airways obstruction and therefore little reversibility and so -blockade should pose no risk. Global initiative for chronic obstructive lung disease recommend that ideally the obstruction should be measured postbronchodilator , although for practical reasons this is not always followed in the real world. The problem is that possibly half of patients with a diagnosis of COPD have some significant reversibility and up to 50% of patients change from being irreversible to reversible between visits, making it difficult for the clinician to be certain of a real fixed component.
